Falmina (nitroglycerin 0.6 mg) Dailymed
Generic: levonorgestrel and ethinyl estradiol is used for the treatment of Breast Neoplasms Cerebral Arterial Diseases Coronary Artery Disease Hypertension Hypogonadism Liver Diseases Menopause, Premature Menorrhagia Neoplasms, Hormone-Dependent Pregnancy Prostatic Neoplasms Thromboembolism Thrombophlebitis Osteoporosis, Postmenopausal Primary Ovarian Insufficiency Endometrial Neoplasms Hot Flashes Tobacco Use Abortion, Spontaneous Cerebrovascular Disorders Coronary Disease Diabetes Mellitus Heart Valve Diseases Jaundice Kidney Diseases Liver Neoplasms Tobacco Use Disorder Uterine Hemorrhage Adenoma, Liver Cell Headache Disorders
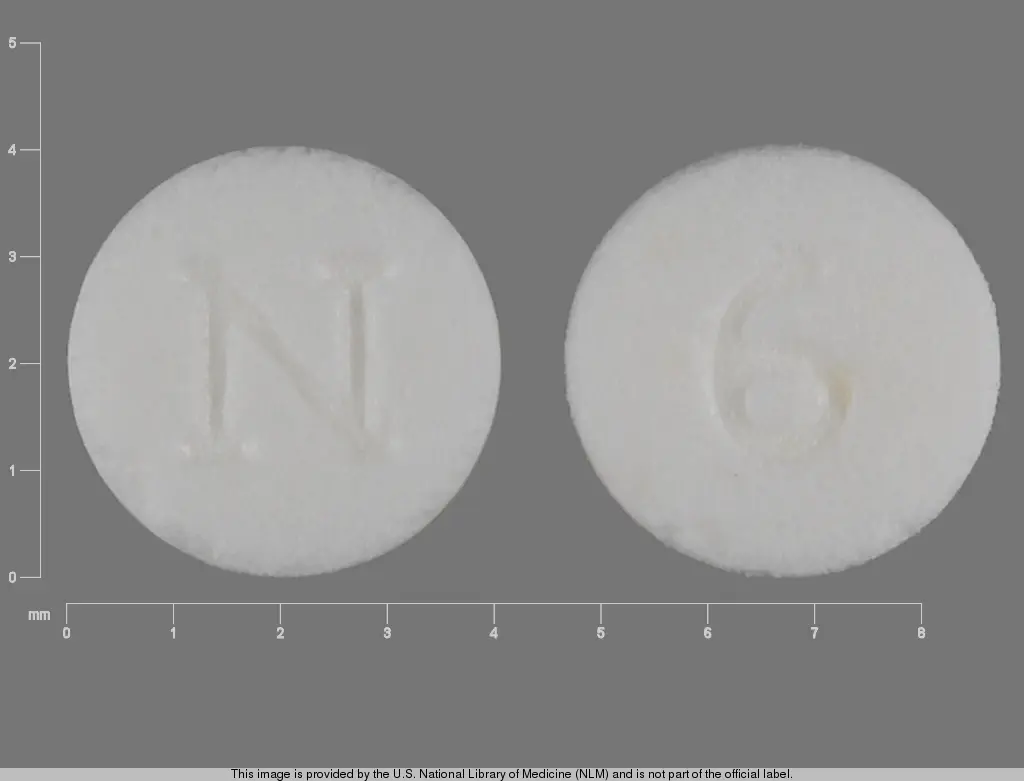
IMPRINT: N 6
SHAPE: round
COLOR: white
All Imprints
frovatriptan succinate 2.5 mg - e 2 5 round white
dipyridamole 75 mg - 19 round orange
aspirin 325 mg - aspirin 44 249 round white
valsartan 80 mg - 7432 tv round pink
calcium fluoride 30 [hp_x] - round white
captopril 100 mg - w 905 round white
levodopa 50 mgentacapone 200 mgcarbidopa 12.5 mg - w782 round brown
calcium acetate 667 mg - p113 round white
lithium carbonate 300 mg - ww 300 round white
cyclophosphamide 25 mg - 54 639 round blue
methylphenidate hydrochloride 10 mg - ciba 3 round green
desloratadine 5 mg - 5 round blue
carvedilol 25 mg - zc42 round white
iloperidone 8 mg - 8 round white
glyburide 2.5 mg - cor 124 round yellow
bismuth subsalicylate 262 mg - rh046 round pink
moexipril hydrochloride 7.5 mg - apo moe 7 5 round white
- r221 round orange
venlafaxine hydrochloride 50 mg - ip 303 round orange
pseudoephedrine hydrochloride 30 mg - tcl016 round red
donepezil hydrochloride 5 mg - i 24 round white
methadone hydrochloride 5 mg - u41 round white
donepezil hydrochloride 10 mg - i 21 round yellow
amlodipine besylate 2.5 mgatorvastatin calcium trihydrate 20 mg - pfizer cdt 252 round white
chlorpheniramine maleate 4 mg - 44 194 round yellow
tamoxifen citrate 20 mg - m 274 round white
hydrochlorothiazide 50 mg - h 3 round orange
pitavastatin calcium 4.18 mg - 4 kc round white
venlafaxine hydrochloride 25 mg - 6147 v round orange
docusate sodium 50 mgsennosides a and b 8.6 mg - tcl081 round orange
quinidine gluconate 324 mg - mp 66 round white
oxycodone hydrochloride 7.5 mgacetaminophen 325 mg - watson 933 round white
cyclobenzaprine hydrochloride 5 mg - tl 211 round orange
trihexyphenidyl hydrochloride 2 mg - 5971 v round white
lamotrigine 50 mg - h009 round orange
rabeprazole sodium 20 mg - 107 round yellow
carbamazepine 200 mg - t 200 mg round pink
enalapril maleate 5 mghydrochlorothiazide 12.5 mg - apo 5 12 5 round red
diclofenac sodium 100 mg - r 717 round yellow
minoxidil 10 mg - dan 5643 10 round white
acetaminophen 500 mg - ap 013 round white
levonorgestrel 0.1 mgethinyl estradiol 0.02 mg - b 965 round pink
clonazepam 0.5 mg - 832 teva round yellow
oxcarbazepine 300 mg - 54 515 round orange
fludrocortisone acetate 0.1 mg - 7033 round white
atovaquone 250 mgproguanil hydrochloride 100 mg - gx cm3 round pink
lamotrigine 50 mg - lamictal xr 50 round green
maprotiline hydrochloride 75 mg - 9 2 m round white
candesartan cilexetil 4 mg - acf 004 round white
memantine hydrochloride 5 mg - m5 v round white
lamotrigine 150 mg - lam 150 apo round yellow
acarbose 50 mg - precose 50 round white
docusate sodium 50 mgsennosides 8.6 mg - tcl 131 round purple
dextroamphetamine saccharate 3.75 mgamphetamine aspartate monohydrate 3.75 mgdextroamphetamine sulfate 3.75 mgamphetamine sulfate 3.75 mg - b 777 1 5 round orange
paroxetine hydrochloride hemihydrate 25 mg - gsk 25 round pink
bupropion hydrochloride 100 mg - wellbutrin 100 round red
memantine hydrochloride 10 mg - m10 x round white
dextroamphetamine saccharate 2.5 mgamphetamine aspartate monohydrate 2.5 mgdextroamphetamine sulfate 2.5 mgamphetamine sulfate 2.5 mg - 1 0 dp round blue
nifedipine 60 mg - 60 adalat cc round pink
lisinopril 10 mghydrochlorothiazide 12.5 mg - lh1 m round white
alprazolam 1 mg - cor 188 round yellow
liothyronine sodium 50 ug - 50 223 round white
venlafaxine hydrochloride 75 mg - 6150 v round orange
metoprolol tartrate 50 mg - c 74 round pink
prednisone 10 mg - west ward 473 round white
trandolapril 2 mg - fx round yellow
pitavastatin calcium 1 mg - 1 kc round white
dextroamphetamine saccharate 3.125 mgamphetamine aspartate monohydrate 3.125 mgdextroamphetamine sulfate 3.125 mgamphetamine sulfate 3.125 mg - 12 5 d p round orange
benztropine mesylate 2 mg - b 1116 round white
chlorpheniramine maleate 12 mg - chlorphen 12 round orange
lisinopril 10 mg - ww 267 round pink
paroxetine hydrochloride hemihydrate 37.5 mg - gsk 37 5 round blue
naproxen 250 mg - 93 147 round red
morphine sulfate 60 mg - m ms 60 round orange
hydrocodone bitartrate 7.5 mgibuprofen 200 mg - 3585 v round white
warfarin sodium 2 mg - ig w 2 round purple
galantamine hydrobromide 12 mg - janssen g 12 round brown
methazolamide 50 mg - eff 20 round white
simvastatin 10 mg - sv 10 round pink
norethindrone 1 mgethinyl estradiol 0.035 mg - b 949 round yellow
potassium chloride 600 mg - ktab round yellow
famciclovir 250 mg - 8118 93 round white
progesterone 100 mg - sv round orange
isosorbide dinitrate 10 mg - gg26 round white
flecainide acetate 50 mg - an 641 round white
buspirone hydrochloride 10 mg - teva 54 round white
topiramate 50 mg - apo tp 50 round yellow
simvastatin 40 mg - sv 40 round pink
isosorbide dinitrate 5 mg - bpi 152 round pink
- b 247 round brown
clonazepam 0.25 mg - b 95 1 4 round white
prednisolone sodium phosphate 30 mg - ora 30 round white
nifedipine 30 mg - m 475 round pink
alendronate sodium 5 mg - 93 5140 round white
chloroquine phosphate 250 mg - 0115 2790 round white
acarbose 25 mg - precose 25 round white
bumetanide 1 mg - e 129 round yellow
levomefolate calcium 0.451 mg - m round orange
flavoxate hydrochloride 100 mg - 58 round white
verapamil hydrochloride 80 mg - watson 343 round white
desipramine hydrochloride 10 mg - 68 7 round blue
levonorgestrel 0.15 mgethinyl estradiol 0.02 mg - tv 076 round pink
atenolol 25 mg - 787 teva round white
dipyridamole 75 mg - c83 round white
hydrocortisone 10 mg - cp 332 round white
desipramine hydrochloride 75 mg - e 722 round blue
citalopram hydrobromide 10 mg - mx31 round orange
lamotrigine 150 mg - taro lmt 150 round white
- 54-980 round blue
topiramate 25 mg - ig 278 round white
hydroxyzine hydrochloride 50 mg - tv 309 round white
cefuroxime axetil 250 mg - w 921 round white
acarbose 25 mg - 54 311 round white
lamotrigine 100 mg - j 246 round white
sennosides a and b 8.6 mg - gpi w2 round brown
metformin hydrochloride 500 mg - h 102 round white
olanzapine 5 mg - m oe1 round yellow
zolpidem tartrate 12.5 mg - a1 round yellow
bupropion hydrochloride 100 mg - g 2442 round yellow
- dan 5540 round white
hydromorphone hydrochloride 4 mg - m 4 round white
phytonadione 5 mg - aton 405 mephyton round yellow
nifedipine 30 mg - 30 adalat cc round pink
tramadol hydrochloride 200 mg - 200 er round white
cinchona officinalis bark 30 [hp_c]coffea arabica fruit 6 [hp_c]strychnos nux-vomica seed 30 [hp_c]matricaria chamomilla flowering top oil 6 [hp_c]artemisia cina flower 30 [hp_c] - none round white
paroxetine hydrochloride hemihydrate 10 mg - zc 15 round white
hydralazine hydrochloride 50 mg - par 028 round orange
benazepril hydrochloride 10 mg - apo be 10 round yellow
propafenone hydrochloride 225 mg - 5125 v round white
eszopiclone 1 mg - 93 e7 round blue
carbinoxamine maleate 4 mg - bp 605 round white
metronidazole 250 mg - 3969 wpi round white
oxybutynin chloride 10 mg - g342 round pink
ethinyl estradiol 0.01 mg - b 556 round yellow
hydrochlorothiazide 6.25 mgbisoprolol fumarate 2.5 mg - ul l round yellow
metoprolol tartrate 100 mg - re 76 round white
aripiprazole 30 mg - tv 7583 round pink
ropinirole hydrochloride 2 mg - 54 231 round orange
- west-ward 248 round yellow
acetaminophen 300 mgcodeine phosphate 15 mg - 2 m round white
calcium carbonate 750 mg - fc round green
levocetirizine dihydrochloride 5 mg - 161 h round white
glipizide 2.5 mg - wpi 900 round orange
torsemide 20 mg - pa 917 round white
olanzapine 7.5 mg - m 335 round white
metformin hydrochloride 500 mg - andrx 674 500 round white
norethindrone acetate 1.5 mgethinyl estradiol 30 ug - b 978 round pink
azathioprine 50 mg - 54 043 round yellow
bupropion hydrochloride 100 mg - apo bup 100 round purple
estradiol 0.5 mg - watson 528 round white
olanzapine 20 mg - tv u4 20 round yellow
levonorgestrel 1.5 mg - g00 round white
nitazoxanide 500 mg - alinia 500 round yellow
zolmitriptan 5 mg - f11 round white
paroxetine hydrochloride hemihydrate 30 mg - m n3 round blue
doxazosin mesylate 8 mg - n 598 8 round white
hydrochlorothiazide 50 mg - 3572 v round orange
levonorgestrel 0.075 mgethinyl estradiol 0.040 mg - dp 511 round white
glipizide 10 mg - 10 round white
norethindrone acetate 1 mgethinyl estradiol 20 ug - b 711 round pink
imipramine hydrochloride 50 mg - par 56 round green
repaglinide 1 mg - p241 round yellow
felodipine 2.5 mg - 450 plendil round green
ciprofloxacin hydrochloride 250 mg - cr 250 round white
pravastatin sodium 10 mg - teva 771 round pink
prednisone 20 mg - tl175 round pink
ethinyl estradiol 0.01 mg - dp 457 round yellow
calcium carbonate 420 mg - az 036 round white
alprazolam 0.5 mg - cor 187 round white
haloperidol 0.5 mg - mylan 351 round orange
midodrine hydrochloride 5 mg - g 422 round orange
carvedilol 12.5 mg - zc41 round white
metformin hydrochloride 850 mg - andrx 675 850 round white
desipramine hydrochloride 25 mg - e 19 round blue
olanzapine 5 mg - tv u1 5 round yellow
felodipine 10 mg - 452 plendil round red
flecainide acetate 50 mg - rx794 round white
fosinopril sodium 40 mg - 202 ig round white
rabeprazole sodium 20 mg - aciphex 20 round yellow
zolpidem tartrate 5 mg - m z1 round purple
metoprolol succinate 100 mg - a ms round white
leucovorin calcium 15 mg - 54 650 round yellow
amoxapine 50 mg - dan 50 5714 round orange
clozapine 100 mg - clozaril 100 round yellow
leucovorin calcium 25 mg - 54 013 round yellow
tramadol hydrochloride 300 mg - 300 er round white
tolterodine tartrate 2 mg - dt round white
doxycycline 50 mg - lci 1335 round yellow
minoxidil 10 mg - 10 mp 89 round white
aspirin 81 mg - az 013 round orange
lorazepam 2 mg - 242 2 watson round white
trandolapril 4 mg - tn4 round white
propranolol hydrochloride 60 mg - 54 85 v round pink
dimethicone 80 mgcalcium carbonate 750 mg - dr round pink
prochlorperazine maleate 10 mg - tl115 round green
dexamethasone 1.5 mg - 54 943 round pink
ranitidine hydrochloride 150 mg - gg 705 round pink
sodium fluoride 0.5 mg - sci 1007 round white
prednisone 5 mg - westward 475 round white
alprazolam 2 mg - sp 324 2 round white
pioglitazone hydrochloride 15 mg - actos 15 round white
aspirin 162 mgacetaminophen 110 mgsalicylamide 152 mgcaffeine 32.4 mg - fr2 round orange
meloxicam 7.5 mg - zc 25 round yellow
metolazone 2.5 mg - m 172 round orange
amlodipine besylate 5 mgolmesartan medoxomil 40 mg - c75 round white
ondansetron hydrochloride 8 mg - r 154 round yellow
diclofenac sodium 75 mgmisoprostol 200 ug - 0398 round white
sitagliptin phosphate 100 mg - 277 round brown
acarbose 25 mg - e71 round white
albuterol sulfate 4 mg - mp 88 round white
topiramate 50 mg - omn 50 round yellow
dextroamphetamine saccharate 5 mgamphetamine aspartate monohydrate 5 mgdextroamphetamine sulfate 5 mgamphetamine sulfate 5 mg - e 401 round orange
trifluoperazine hydrochloride 2 mg - m t4 round white
oxycodone hydrochloride 20 mg - op 20 round pink
citalopram hydrobromide 10 mg - 206 ig round yellow
trazodone hydrochloride 100 mg - pliva 434 round white
zolmitriptan 2.5 mg - zomig 25 round yellow
desipramine hydrochloride 50 mg - e 721 round blue
dextroamphetamine saccharate 7.5 mgamphetamine aspartate monohydrate 7.5 mgdextroamphetamine sulfate 7.5 mgamphetamine sulfate 7.5 mg - e 404 round orange
trazodone hydrochloride 100 mg - apo t100 round white
hydralazine hydrochloride 100 mg - hp 4 round pink
meclizine hydrochloride 25 mg - m mcz 25 round white
levetiracetam 250 mg - m 613 round white
alendronate sodium 35 mg - 637 round white
dexamethasone 0.5 mg - 54 299 round yellow
carbidopa 25 mglevodopa 100 mg - apo 25 100 round yellow
norethindrone 0.5 mgethinyl estradiol 0.035 mg - b 941 round yellow
irbesartan 75 mg - m in1 round white
calcium ascorbate 50 mgcalcium threonate 50 mgcholecalciferol 6 ug.alpha.-tocopherol acetate, dl- 3.5 [iu]pyridoxine hydrochloride 2 mgfolic acid 1 mgcalcium carbonate 250 mgferrous fumarate 40 mgmagnesium oxide 50 mgzinc oxide 15 mgcupric oxide 2 mg - tl014 round grey
hydromorphone hydrochloride 2 mg - p 2 round orange
norethindrone acetate 1 mgethinyl estradiol .02 mg - 93 912 round white
sodium starch glycolate type a corn 3.61 mgpovidone k30 5.415 mgstearic acid 1.805 mgacetaminophen 324.9 mgstarch, corn 25.27 mg - 325 round white
megestrol acetate 20 mg - par 289 round white
propranolol hydrochloride 40 mg - 54 84 v round green
tinidazole 250 mg - tm 250 round pink
lisinopril 40 mg - 3761 round white
escitalopram oxalate 10 mg - 11 36 round white
amitriptyline hydrochloride 75 mg - m 37 round blue
medroxyprogesterone acetate 2.5 mg - g3740 round orange
amlodipine besylate 5 mgvalsartan 160 mghydrochlorothiazide 25 mg - tv 7037 round yellow
trihexyphenidyl hydrochloride 2 mg - dan dan 5335 round white
amitriptyline hydrochloride 100 mg - 2105 v round red
acarbose 100 mg - e73 round white
norethindrone 1 mgethinyl estradiol 0.035 mg - b 943 round orange
lorazepam 2 mg - mylan 777 round white
bisoprolol fumarate 5 mghydrochlorothiazide 6.25 mg - b 50 round pink
oxycodone hydrochloride 15 mg - m 15 round green
repaglinide 1 mg - 745 c round yellow
butalbital 50 mgacetaminophen 325 mgcaffeine 40 mg - lci 1695 round blue
aripiprazole 30 mg - a 011 30 round pink
levonorgestrel 0.15 mgethinyl estradiol 0.03 mg - b 555 round blue
glipizide 10 mg - glipizide xl 10 round white
olanzapine 2.5 mg - m 157 round orange
promethazine hydrochloride 50 mg - zc03 round white
zolmitriptan 5 mg - zomig 5 round pink
acetaminophen 300 mgcodeine phosphate 30 mg - 3 tv 150 round white
nadolol 80 mgbendroflumethiazide 5 mg - kpi 284 corzide 80 5 round white
lamotrigine 200 mg - lamictal xr 200 round blue
albuterol sulfate 2 mg - m 255 round white
bupropion hydrochloride 75 mg - wellbutrin 75 round yellow
carisoprodol 350 mg - dan 5513 round white
hydrochlorothiazide 50 mg - 112 s g round white
cyclophosphamide 50 mg - 54 980 round blue
benztropine mesylate 0.5 mg - cor 143 round white
norethindrone acetate 1 mgethinyl estradiol 20 ug - b 977 round yellow
perindopril erbumine 2 mg - d 5 7 round white
propranolol hydrochloride 10 mg - pliva 467 round orange
pramipexole dihydrochloride 0.25 mg - p2 round blue
amitriptyline hydrochloride 100 mg - gg461 round orange
ropinirole 2 mg - 93 5285 round pink
olanzapine 10 mg - lilly 4117 round white
trihexyphenidyl hydrochloride 2 mg - w 4 round white
repaglinide 0.5 mg - p240 round white
nifedipine 30 mg - eln 30 round brown
trandolapril 4 mg - lu h03 round red
warfarin sodium 10 mg - ig w 10 round white
bismuth subsalicylate 262 mg - ap 045 round pink
ropinirole hydrochloride 4 mg - m re4 round brown
dipyridamole 25 mg - 17 round orange
lithium carbonate 450 mg - 224 g breakline round yellow
estradiol 1 mgnorethindrone acetate 0.5 mg - novo 288 round white
venlafaxine hydrochloride 75 mg - 759 round
enalapril maleate 10 mg - elp 10 round brown
carvedilol 25 mg - g41 25 round white
metoprolol tartrate 50 mg - 477 round white
pitavastatin calcium 2 mg - 2 kc round white
folic acid 1 mg - ig 210 round yellow
meloxicam 7.5 mg - 7 5 round yellow
bupropion hydrochloride 100 mg - a 171 round yellow
chlorpromazine hydrochloride 25 mg - gg476 25 round orange
carbidopa 25 mglevodopa 250 mg - m c53 round green
pramipexole dihydrochloride 0.125 mg - 91 round white
dimenhydrinate 50 mg - 0111 v round white
chlorpromazine hydrochloride 200 mg - gg457 200 round orange
ranitidine hydrochloride 150 mg - apo ran 150 round pink
tramadol hydrochloride 50 mg - m t7 round white
citalopram hydrobromide 40 mg - 208 ig round white
carvedilol 6.25 mg - zc40 round white
labetalol hydrochloride 200 mg - cl38 200 round white
diclofenac potassium 50 mg - 93 948 round orange
fosinopril sodium 20 mg - 201 ig round white
clonazepam 0.125 mg - b 94 1 8 round white
carisoprodol 350 mg - 2410 v round white
candesartan cilexetil 8 mg - acg 008 round pink
risperidone 0.25 mg - 93 221 round yellow
tamoxifen citrate 10 mg - m 144 round white
pyridostigmine bromide 60 mg - mestinon v 60 round white
carbidopa 25 mglevodopa 100 mg - apo 131 round brown
citalopram hydrobromide 10 mg - a 05 round orange
spironolactone 100 mg - searle 1031 aldactone 100 round orange
glipizide 10 mg - 9200 teva round white
nisoldipine 17 mg - sci 501 round yellow
promethazine hydrochloride 25 mg - an 521 round white
olanzapine 7.5 mg - lilly 4116 round white
spironolactone 100 mg - 58 82 v round white
oxycodone hydrochloride 10 mg - op 10 round white
propranolol hydrochloride 80 mg - 54 86 v round yellow
amiodarone hydrochloride 100 mg - as 100 round yellow
levonorgestrel 0.050 mgethinyl estradiol 0.030 mg - dp 510 round pink
mebendazole 100 mg - 93 107 round orange
sennosides a and b 8.6 mg - az217 round brown
estradiol valerate 2 mgdienogest 3 mg - dh round yellow
amlodipine besylate 2.5 mgatorvastatin calcium trihydrate 10 mg - r 407 round white
meloxicam 15 mg - m 89 round yellow
nifedipine 60 mg - b 60 round red
methocarbamol 500 mg - west ward 290 round white
metformin hydrochloride 850 mg - bms 6070 850 round white
aspirin 81 mg - heart round yellow
aripiprazole 15 mg - a 009 15 round yellow
clomiphene citrate 50 mg - watson 781 round white
olanzapine 2.5 mg - c 45 round yellow
dexmethylphenidate hydrochloride 5 mg - 93 5276 round yellow
quinapril hydrochloride 20 mg - lu f03 round yellow
ethynodiol diacetate 1 mgethinyl estradiol 35 ug - b 14 round yellow
griseofulvin 500 mg - ortho 214 round white
cefprozil 250 mg - 93 1077 round orange
felodipine 5 mg - e137 round pink
propranolol hydrochloride 10 mg - mylan 182 10 round orange
eltrombopag olamine 25 mg - gs nx3 25 round orange
clonazepam 2 mg - b 98 2 round white
allopurinol 300 mg - m 71 round white
estradiol 0.5 mg - e 3 m round white
spironolactone 50 mg - mp 542 round white
- 3m tr 50 round white
metoprolol tartrate 100 mg - c 75 round blue
pioglitazone hydrochloride 15 mg - 31 h round white
salsalate 500 mg - bp 507 round yellow
bethanechol chloride 50 mg - lci 1329 round yellow
codeine phosphate 15 mgacetaminophen 300 mg - 2063 v 2 round white
methimazole 5 mg - bp 655 round white
tolterodine tartrate 1 mg - to round white
atovaquone 62.5 mgproguanil hydrochloride 25 mg - gx cg7 round pink
lamotrigine 200 mg - l124 round white
levonorgestrel 0.15 mgethinyl estradiol 0.03 mg - b 992 round pink
metoclopramide hydrochloride 10 mg - teva 2203 round white
venlafaxine hydrochloride 37.5 mg - 6148 v round orange
irbesartan 150 mghydrochlorothiazide 12.5 mg - 54 857 round red
diclofenac sodium 100 mg - dx 41 round pink
risedronate sodium monohydrate 35 mg - teva 7389 round orange
ethinyl estradiol 0.01 mg - tv 077 round yellow
aspirin 325 mg - aspirin 44157 round white
ropinirole hydrochloride 2 mg - 975 hh round pink
nilutamide 150 mg - 168d round white
carbidopa 25 mglevodopa 100 mg - 93 293 teva round yellow
doxycycline 100 mg - i63 round orange
testosterone 30 mg - a round white
benazepril hydrochloride 20 mg - lotensin 20 round pink
simvastatin 40 mg - rx792 round red
trifluoperazine hydrochloride 5 mg - gg55 5 round purple
albuterol sulfate 4 mg - v 4 round green
metformin hydrochloride 500 mg - a 12 round white
topiramate 200 mg - ig 281 round pink
quinidine sulfate 200 mg - dan dan 5438 round white
doxycycline 50 mg - i61 round orange
metformin hydrochloride 500 mg - 574 round white
carbamazepine 100 mg - taro 16 round white
hydrochlorothiazide 50 mg - hp 46 round white
trifluoperazine hydrochloride 5 mg - m t5 round purple
imipramine hydrochloride 50 mg - v13 lu round brown
lamotrigine 25 mg - taro lmt 25 round white
aripiprazole 10 mg - 10 18 round white
propranolol hydrochloride 80 mg - dan 5557 80 round yellow
benztropine mesylate 0.5 mg - b 1114 round white
hydrochlorothiazide 12.5 mglisinopril 10 mg - ww 62 round blue
aspirin 81 mg - 81 round yellow
doxazosin mesylate 1 mg - m d9 round white
mitotane 500 mg - bl l1 round white
lamotrigine 100 mg - par 563 round brown
cetirizine hydrochloride 5 mgpseudoephedrine hydrochloride 120 mg - 5029 5 120 round white
linagliptin 5 mg - d5 round red
estradiol 2 mg - watson 488 round green
bumetanide 2 mg - e 130 round brown
lamotrigine 25 mg - lmt 25 round white
alprazolam 2 mg - r 87 round pink
nifedipine 60 mg - ku 261 round pink
norethindrone acetate 1.5 mgethinyl estradiol 0.03 mg - watson 631 round green
doxycycline hyclate 100 mg - dan 5553 round orange
carvedilol 6.25 mg - m c32 round white
atenolol 100 mg - z 67 round white
demeclocycline hydrochloride 150 mg - an 54 round red
risperidone 0.5 mg - 93 225 round red
bethanechol chloride 50 mg - bcl 50 832 round yellow
bisacodyl 5 mg - tcl 003 round orange
bupropion hydrochloride 150 mg - 141 round white
morphine sulfate 30 mg - m 30 round purple
azilsartan kamedoxomil 80 mg - asl 80 round white
dextroamphetamine sulfate 10 mg - 953 10 b round pink
neomycin sulfate 500 mg - zynova 01 round white
quetiapine fumarate 100 mg - apo que 100 round yellow
quetiapine fumarate 200 mg - apo que 200 round white
finasteride 5 mg - ig 412 round blue
clonidine hydrochloride 0.1 mg - 241 round pink
glipizide 5 mg - gxl 5 round white
- deltasone 20 round orange
guaifenesin 600 mg - l498 round white
amlodipine besylate 5 mg - m a9 round blue
desipramine hydrochloride 10 mg - 341 round white
captopril 12.5 mg - w 7 round white
diclofenac sodium 100 mg - m 355 round yellow
metoprolol tartrate 100 mg - 93 734 round blue
anastrozole 1 mg - adx1 round white
haloperidol 10 mg - mylan 334 round green
imipramine hydrochloride 50 mg - gg 42 round green
desipramine hydrochloride 75 mg - gg166 round white
chlorpromazine hydrochloride 200 mg - 832 200 round brown
adefovir dipivoxil 10 mg - 3 round white
dipyridamole 50 mg - c82 round white
methimazole 10 mg - bp 656 round white
montelukast sodium 5 mg - 54 741 round pink
ramelteon 8 mg - tak ram 8 round orange
fluvastatin sodium 80 mg - lescol xl 80 round yellow
hyoscyamine sulfate 0.125 mg - pad h round white
azilsartan kamedoxomil 40 mgchlorthalidone 12.5 mg - ac 40 12 5 round red
clonazepam 0.5 mg - r 33 round pink
zidovudine 300 mg - 54 777 round white
lovastatin 20 mg - 20 round orange
moexipril hydrochloride 15 mg - g 208 round brown
desogestrel 0.15 mgethinyl estradiol 0.02 mg - dp 021 round white
bupropion hydrochloride 100 mg - e over 410 round blue
fosinopril sodium 40 mg - ig 202 round white
pilocarpine hydrochloride 5 mg - lan 1313 round white
hydrocodone bitartrate 7.5 mgibuprofen 200 mg - 5161 round white
bisoprolol fumarate 5 mghydrochlorothiazide 6.25 mg - e 704 round red
moexipril hydrochloride 7.5 mg - g 209 round pink
hydrocortisone 5 mg - cp 331 round white
olanzapine\ 7.5 mg - 7654 round white
metoprolol tartrate 100 mg - m 47 round blue
propranolol hydrochloride 20 mg - dan 5555 20 round blue
lisinopril 20 mghydrochlorothiazide 25 mg - lh3 m round green
spironolactone 100 mg - an 515 round brown
thioridazine hydrochloride 100 mg - mp 160 round yellow
ascorbic acid 100 mgthiamine mononitrate 1.5 mgriboflavin 1.7 mgniacinamide 20 mgpyridoxine hydrochloride 10 mgfolic acid 1 mgcobalamin 6 ugbiotin 300 ugcalcium pantothenate 10 mgzinc citrate 50 mg - h round yellow
glycopyrrolate 1 mg - k 400 round white
allopurinol 100 mg - zyloprim 100 round white
norethindrone acetate 1 mgethinyl estradiol 0.02 mg - pd 915 round white
doxazosin mesylate 2 mg - m d10 round pink
acetazolamide 125 mg - t52 round white
ribavirin 200 mg - zc19 round pink
clozapine 100 mgaspartame 12.4 mg - a08 round yellow
bisoprolol fumarate 5 mghydrochlorothiazide 6.25 mg - m 503 round blue
estropipate 3 mg - watson 416 round blue
dimethicone 125 mg - ap 040 round white
hydrocortisone 20 mg - ww 254 round white
haloperidol 2 mg - mylan 214 round orange
desipramine hydrochloride 100 mg - e 736 round blue
phenobarbital 16.2 mg - 5011 v round white
aripiprazole 15 mg - ari 15 apo round yellow
ciprofloxacin hydrochloride 250 mg - y101 round white
alprazolam 0.5 mg - r 83 round white
- 3m tr 100 round white
desmopressin acetate 0.2 mg - 0 2 37 av round white
naproxen 250 mg - ip188 250 round white
amlodipine besylate 2.5 mgatorvastatin calcium trihydrate 40 mg - pfizer cdt 254 round white
clobazam 5 mg - lu 5 round white
propafenone hydrochloride 225 mg - mp 512 round white
nifedipine 30 mg - b 30 round red
atovaquone 250 mgproguanil hydrochloride 100 mg - 404 g round pink
buprenorphine hydrochloride 2 mgnaloxone hydrochloride dihydrate 0.5 mg - 154 round white
lisinopril 20 mghydrochlorothiazide 12.5 mg - a 28 round yellow
torsemide 5 mg - pa 915 round white
penicillin v potassium 250 mg - gg949 pvk250 round white
chlorambucil 2 mg - gx eg3 l round brown
pioglitazone hydrochloride 45 mg - actos 45 round white
trazodone hydrochloride 100 mg - mp 114 round white
ketoconazole 200 mg - janssen nizoral round white
prednisone 20 mg - dan dan 5443 round orange
norethindrone 0.5 mgethinyl estradiol 0.035 mg - b 951 round yellow
hydroxyzine hydrochloride 25 mg - 3616 v round green
atenolol 50 mg - d 22 round white
finasteride 5 mg - h 37 round blue
propafenone hydrochloride 150 mg - 5124 v round white
allopurinol 300 mg - n021 round orange
metolazone 5 mg - 644 5 round blue
clopidogrel bisulfate 75 mg - apo cl 75 round pink
morphine sulfate 30 mg - m ms 30 round purple
codeine sulfate 60 mg - 60 54 412 round white
zinc acetate 2 [hp_x]zinc gluconate 2 [hp_x] - rd round red
primidone 50 mg - lan 1301 round white
lamotrigine 150 mg - j 247 round white
simvastatin 5 mg - ll c01 round brown
promethazine hydrochloride 25 mg - gg 225 round white
dimenhydrinate 50 mg - 44 198 round white
simvastatin 40 mg - ll c04 round red
doxycycline hyclate 20 mg - mp 573 round white
potassium chloride 600 mg - kc 8 round blue
chlorpromazine hydrochloride 50 mg - sz 203 round brown
- dp 519 round green
amlodipine besylate 10 mg - s25 round white
alendronate sodium 5 mg - m a6 round white
risperidone 4 mg - p 403 round white
- b 343 round pink
quetiapine fumarate 100 mg - 93 8162 round orange
guanfacine hydrochloride 1 mg - watson 444 round pink
hydrocortisone 5 mg - cortef 5 round white
acyclovir 400 mg - m 253 round white
mirtazapine 45 mg - m 545 round brown
norethindrone 0.75 mgethinyl estradiol 0.035 mg - b 942 round blue
amlodipine besylate 10 mgolmesartan medoxomil 20 mg - c74 round orange
methylphenidate hydrochloride 20 mg - dan 20 5884 round orange
betaxolol hydrochloride 20 mg - e39 round white
thyroid, porcine 15 mg - a tc round brown
busulfan 2 mg - gx ef3 m round white
solifenacin succinate 5 mg - 150 round yellow
perindopril erbumine 8 mg - d 5 9 round white
risperidone 2 mg - 93 7241 round orange
bumetanide 0.5 mg - e 128 round green
terbinafine hydrochloride 250 mg - lamisil 250 round yellow
midodrine hydrochloride 10 mg - e 149 round
isosorbide mononitrate 10 mg - 10 ku 106 round white
levothyroxine sodium 25 ug - synthroid 25 round orange
metformin hydrochloride 500 mg - 397 round white
hydrochlorothiazide 50 mg - westward 257 round orange
dextroamphetamine saccharate 5 mgamphetamine aspartate monohydrate 5 mgdextroamphetamine sulfate 5 mgamphetamine sulfate 5 mg - 2 0 dp round orange
topiramate 50 mg - m t12 round white
bupropion hydrochloride 150 mg - e over 415 round purple
liothyronine sodium 50 ug - kpi 117 round white
baclofen 10 mg - lci 1330 round white
dexmethylphenidate hydrochloride 2.5 mg - 93 5275 round blue
amiodarone hydrochloride 200 mg - as 200 round yellow
carbidopa 10 mglevodopa 100 mg - r 538 round blue
aripiprazole 20 mg - ari 20 apo round white
metronidazole 250 mg - 93 851 round white
bicalutamide 50 mg - bcm 50 round white
prednisone 20 mg - west ward 477 round red
acetaminophen 325 mgchlorpheniramine maleate 4 mgphenylephrine hydrochloride 10 mg - xl3 forte round yellow
iloperidone 12 mg - 12 round white
losartan potassium 25 mg - 11 round white
sumatriptan succinate 25 mg - m s4 round white
cyclobenzaprine hydrochloride 10 mg - pliva 563 round yellow
losartan potassium 100 mghydrochlorothiazide 25 mg - 54 557 round yellow
glycopyrrolate 2 mg - 3181 v round white
glipizide 5 mg - 9201 teva round white
bupropion hydrochloride 100 mg - m 435 round blue
aminocaproic acid 500 mg - vp 045 round white
metformin hydrochloride 850 mg - sg 106 round white
valsartan 160 mghydrochlorothiazide 12.5 mg - m v22 round orange
labetalol hydrochloride 100 mg - watson 605 round brown
guanfacine hydrochloride 3 mg - 853 round yellow
bupropion hydrochloride 150 mg - wellbutrin xl 150 round white
losartan potassium 100 mg - sz 214 round pink
citalopram hydrobromide 10 mg - rdy 342 round brown
erythromycin stearate 250 mg - es round pink
propranolol hydrochloride 80 mg - mylan 185 80 round yellow
metolazone 5 mg - zaroxolyn 5 round blue
glycopyrrolate 2 mg - horizon 205 round white
terbinafine hydrochloride 250 1 - 209 ig round white
bupropion hydrochloride 150 mg - m bu1 round green
risperidone 0.5 mg - sz z1 round pink
carbidopa 25 mglevodopa 250 mg - r 540 round blue
simvastatin 40 mg - a 03 round pink
phenazopyridine hydrochloride 200 mg - 612 round brown
doxycycline 75 mg - lci 1535 round yellow
- 405 n round pink
terbutaline sulfate 5 mg - lci 1311 round white
ketoconazole 200 milligram in 1 tablet - ket 200 apo round white
nadolol 80 mg - 80 z 4237 round white
bisoprolol fumarate 5 mg - m 523 round purple
nifedipine 90 mg - b 90 round yellow
clonazepam 1 mg - r 34 round yellow
donepezil hydrochloride 5 mg - teva 738 round white
amlodipine besylate 5 mgvalsartan 160 mg - tv j2 round yellow
cilostazol 100 mg - m c42 round white
cilostazol 50 mg - e 123 round white
diltiazem hydrochloride 30 mg - m 23 round white
ropinirole hydrochloride 8 mg - m re8 round red
enalapril maleate 2.5 mg - t 2 round yellow
morphine sulfate 15 mg - abg 15 round blue
benazepril hydrochloride 10 mg - e 53 round orange
amiloride hydrochloride 5 mghydrochlorothiazide 50 mg - 555 483 barr round yellow
desipramine hydrochloride 25 mg - 342 round blue
paroxetine hydrochloride hemihydrate 25 mg - m p4 round purple
clonidine hydrochloride 0.2 mg - r128 round orange
glipizide 10 mg - wpi 845 round white
bisoprolol fumarate 10 mg - 93 5271 round white
- b 944 round white
amitriptyline hydrochloride 50 mg - 2103 v round brown
venlafaxine hydrochloride 50 mg - zc 66 round orange
bethanechol chloride 25 mg - pliva 325 round yellow
toremifene citrate 60 mg - to 60 round white
leflunomide 10 mg - hp 43 round white
oxycodone hydrochloride 5 mg - 4810 v round white
amitriptyline hydrochloride 75 mg - 2104 v round orange
guaifenesin 400 mg - 44 532 round blue
labetalol hydrochloride 200 mg - 4365 teva round white
risperidone 0.5 mg - m r5 round brown
meclizine hydrochloride 25 mg - 21g round pink
nadolol 20 mg - kpi 232 corgard 20 round blue
ropinirole hydrochloride 2 mg - cor 204 round pink
lovastatin 20 mg - cti 142 round white
thioridazine hydrochloride 10 mg - mp 12 round yellow
clozapine 25 mg - c 7 m round orange
propafenone hydrochloride 150 mg - gs tf5 round white
melphalan 2 mg - gx eh3 a round white
dicyclomine hydrochloride 20 mg - m d6 round blue
lithium carbonate 300 mg - 54 452 round white
enalapril maleate 20 mg - m e18 round blue
acetaminophen 300 mgcodeine phosphate 30 mg - 3 m round white
bupropion hydrochloride 200 mg - 738 round white
amitriptyline hydrochloride 100 mg - m 38 round orange
primaquine phosphate 15 mg - w p97 round pink
estradiol 1 mg - watson 487 round grey
aripiprazole 20 mg - a 010 20 round white
eletriptan hydrobromide 40 mg - rep40 pfizer round orange
dexamethasone 2 mg - 54 662 round white
digoxin 250 ug - lanoxin x3a round white
fluvoxamine maleate 100 mg - e 157 round brown
lisinopril 5 mg - m l23 round orange
propranolol hydrochloride 20 mg - mylan 183 20 round blue
thioridazine hydrochloride 50 mg - m 59 50 round orange
doxazosin mesylate 1 mg - apo 093 round white
flecainide acetate 50 mg - b 859 round white
doxycycline hyclate 100 mg - ww 112 round orange
dicyclomine hydrochloride 20 mg - lan 1282 round blue
lisinopril 20 mg - w 941 round yellow
triamterene 75 mghydrochlorothiazide 50 mg - watson 348 round yellow
ondansetron 4 mg - z4 round white
propranolol hydrochloride 60 mg - mylan pr60 60 round purple
mirtazapine 30 mg - 93 7304 round white
dronabinol 10 mg - um round orange
nystatin 500000 [usp'u] - mp 83 round brown
risperidone 3 mg - sz z5 round pink
bupropion hydrochloride 200 mg - wpi 3385 round white
lisinopril 2.5 mg - watson 405 round white
lovastatin 10 mg - 926 teva round orange
oxybutynin chloride 5 mg - m o 5 round green
- 633 round white
topiramate 50 mg - ig 279 round yellow
meperidine hydrochloride 100 mg - 382 b round white
azilsartan kamedoxomil 40 mg - asl 40 round white
lovastatin 40 mg - 635 round yellow
bethanechol chloride 5 mg - bcl 5 832 round white
alendronate sodium 70 mg - 638 round white
bupropion hydrochloride 100 mg - wellbutrin sr 100 round blue
nadolol 80 mg - sz467 round white
bupropion hydrochloride 150 mg - a 133 round yellow
- 54-639 round blue
saxagliptin hydrochloride 5 mg - 5 4215 round pink
- dp 331 round green
medroxyprogesterone acetate 10 mg - provera 10 round white
metformin hydrochloride 500 mg - i45 round white
furosemide 80 mg - lasix 80 round white
clarithromycin 250 mg - 54 271 round white
methazolamide 25 mg - eff 21 round white
levonorgestrel 90 ugethinyl estradiol 20 ug - 295 watson round white
hydrochlorothiazide 25 mg - d 27 round pink
mirtazapine 15 mg - tz 1 round white
venlafaxine hydrochloride 225 mg - os304 round white
lisinopril 40 mg - rx535 round yellow
imatinib mesylate 100 mg - nvr sa round yellow
aspirin 325 mg - t round orange
lisinopril 20 mghydrochlorothiazide 12.5 mg - lh2 m round yellow
hydrocortisone 20 mg - cortef 20 round white
oxycodone hydrochloride 5 mgacetaminophen 325 mg - endo 602 round white
atenolol 50 mgchlorthalidone 25 mg - m 63 round white
metoclopramide hydrochloride 5 mg - bl 92 round white
amlodipine besylate 2.5 mg - 2108 v round white
ropinirole hydrochloride 4 mg - 977 hh round brown
phenylephrine hydrochloride 5 mg - fr4 round pink
clonidine hydrochloride 0.2 mgchlorthalidone 15 mg - m 27 round yellow
risperidone 1 mg - m r11 round white
amoxicillin 200 mgclavulanate potassium 28.5 mg - ggn2 round pink
flavoxate hydrochloride 100 mg - e58 round white
aspirin 81 mg - l467 round orange
hydroxyzine hydrochloride 50 mg - pa 309 round white
levonorgestrel 0.15 mgethinyl estradiol 0.03 mg - tv 074 round purple
donepezil hydrochloride 5 mg - 5 aricept round white
carbamazepine 100 mg - t 100 mg round yellow
bupropion hydrochloride 150 mg - g 2444 round yellow
clozapine 25 mg - clozaril 25 round yellow
phenobarbital 64.8 mg - 5013 v round white
benztropine mesylate 2 mg - cor 145 round white
tranylcypromine sulfate 10 mg - 250 k round pink
darifenacin 15 mg - df 15 round orange
olmesartan medoxomil 20 mgamlodipine besylate 5 mghydrochlorothiazide 12.5 mg - c51 round orange
escitalopram oxalate 5 mg - f 53 round white
fenofibrate 50 mg - fh 50 round white
enalapril maleate 2.5 mg - m e15 round white
diclofenac sodium 75 mg - cti 103 round white
amitriptyline hydrochloride 50 mg - gg431 round brown
hydroxyzine hydrochloride 25 mg - m h25 round blue
cyclobenzaprine hydrochloride 5 mg - m 771 round blue
glipizide 5 mg - mylan g1 round white
alendronate sodium 5 mg - a 5 round white
mirtazapine 30 mg - tz 2 round white
glipizide 2.5 mg - gxl 2 5 round blue
oxybutynin chloride 15 mg - ku 272 round white
calcium carbonate 750 mg - as round
dextroamphetamine saccharate 1.25 mgamphetamine aspartate monohydrate 1.25 mgdextroamphetamine sulfate 1.25 mgamphetamine sulfate 1.25 mg - 5 dp round white
finasteride 1 mg - 714 round red
donepezil hydrochloride 10 mg - 10 aricept round yellow
- tolinase 100 round white
nisoldipine 25.5 mg - m ne 25 round orange
desipramine hydrochloride 10 mg - e 29 round white
- 428 round orange
amitriptyline hydrochloride 50 mg - m 36 round brown
metformin hydrochloride 500 mg - e 213 round white
prednisone 5 mg - dan dan 5052 round white
donepezil hydrochloride 10 mg - x 12 round yellow
quetiapine fumarate 100 mg - seroquel 100 round yellow
ciprofloxacin hydrochloride 250 mg - p 250 round white
diclofenac potassium 50 mg - gg977 round white
amiloride hydrochloride anhydrous 5 mg - par 117 round yellow
escitalopram oxalate 20 mg - 251 ig round white
famotidine 20 mg - m f1 round yellow
lamotrigine 150 mg - l123 round white
lorazepam 0.5 mg - 240 0 5 watson round white
timolol maleate 10 mg - m 221 round green
bupropion hydrochloride 300 mg - wpi 3332 round white
fexofenadine hydrochloride 180 mg - 93 7253 round orange
flavoxate hydrochloride 100 mg - g 181 round white
bupropion hydrochloride 100 mg - 736 round white
metoprolol tartrate 25 mg - c 73 round white
naproxen sodium 220 mg - 220 round blue
atenolol 50 mg - 93 752 teva round white
oxybutynin chloride 10 mg - ku 271 round white
tiagabine hydrochloride 4 mg - c 404 round yellow
hydralazine hydrochloride 25 mg - pliva 327 round orange
famotidine 40 mg - cti 122 round white
norethindrone 1 mgethinyl estradiol 0.035 mg - b 342 round white
carbamazepine 200 mg - 109 teva round white
- dan 5552 round white
amantadine hydrochloride 100 mg - 832 amt round orange
lovastatin 40 mg - 40 round orange
clopidogrel bisulfate 75 mg - r 196 round white
glipizide 10 mg - apo glp 10 round white
pioglitazone hydrochloride 30 mg - teva 7272 round white
prochlorperazine maleate 5 mg - gg952 5 round yellow
rifaximin 200 mg - sx round pink
labetalol hydrochloride 300 mg - e118 round white
sertraline hydrochloride 25 mg - s 21 round white
flecainide acetate 100 mg - 54070 round white
chlorothiazide 250 mg - westward 209 round white
atenolol 100 mgchlorthalidone 25 mg - tenoretic 117 round white
diltiazem hydrochloride 30 mg - marion 1771 round green
acamprosate calcium 333 mg - 435 round white
escitalopram oxalate 20 mg - ig 251 round white
bupropion hydrochloride 200 mg - a161 round red
escitalopram oxalate 5 mg - ig 249 round white
prasugrel hydrochloride 5 mg - s77 round pink
bupropion hydrochloride 300 mg - a102 round white
hyoscyamine sulfate 0.125 mg - 644 round white
venlafaxine hydrochloride 37.5 mg - y02 round pink
escitalopram oxalate 10 mg - 5851 10 round white
levothyroxine sodium 0.175 mg - jsp 563 round purple
metoclopramide hydrochloride 5 mg - tv 2204 round white
acetaminophen 500 mg - fr1 round white
hyoscyamine sulfate 0.12 mgsodium phosphate, monobasic, monohydrate 40.8 mgphenyl salicylate 36.2 mgmethenamine 81.6 mgmethylene blue 10.8 mg - 293 round purple
chlorpheniramine maleate 4 mgphenylephrine hydrochloride 10 mg - 44 525 round white
demeclocycline hydrochloride 300 mg - an 55 round red
calcium acetate 667 mg - cyp910 round white
naltrexone hydrochloride 50 mg - b 50 902 round white
hydralazine hydrochloride 50 mg - pliva 328 round orange
promethazine hydrochloride 25 mg - z c 0 2 round white
pioglitazone hydrochloride 30 mgmetformin hydrochloride 1000 mg - 4833x 30 1000 round white
meprobamate 400 mg - 591 a round white
adefovir dipivoxil 10 mg - gilead 10 round white
propranolol hydrochloride 80 mg - pliva 471 round yellow
clonazepam 2 mg - 834 teva round white
fluphenazine hydrochloride 10 mg - gg490 round brown
indapamide 1.25 mg - m 69 round pink
diclofenac sodium 100 mg - gg 904 round pink
metformin hydrochloride 1000 mg - g 45 1000 round white
benztropine mesylate 2 mg - 2327 v round white
eszopiclone 3 mg - s193 round blue
trospium chloride 20 mg - l 1 round yellow
midodrine hydrochloride 10 mg - mh 3 m round white
captopril 25 mg - ww 172 round white
meperidine hydrochloride 50 mg - 381 b round white
nifedipine 30 mg - ku 260 round pink
chloroquine phosphate 500 mg - cn500 round white
venlafaxine hydrochloride 100 mg - y05 round pink
acetaminophen 300 mgcodeine phosphate 60 mg - 4 93 350 round white
risedronate sodium 150 mg - apo ris 150 round blue
lamotrigine 200 mg - lamictal 200 round white
glipizide 5 mg - wpi 844 round orange
olanzapine 5 mg - apo ola 5 round white
cyproheptadine hydrochloride 4 mg - par 043 round white
nifedipine 60 mg - eln 60 round brown
carvedilol 3.125 mg - g round white
ibuprofen 200 1 - ibu 200 round brown
bethanechol chloride 10 mg - an 572 round white
levonorgestrel 0.15 mgethinyl estradiol 0.025 mg - tv 075 round pink
naproxen sodium 275 mg - nps 275 round blue
fosinopril sodium 10 mghydrochlorothiazide 12.5 mg - i 3 round white
levothyroxine sodium 125 ug - synthroid 125 round brown
metoclopramide hydrochloride 5 mg - wpi 2228 round green
sumatriptan succinate 50 mg - sa 50 round white
venlafaxine hydrochloride 25 mg - 9 3 199 round orange
terbinafine hydrochloride 250 mg - c134 round white
acetazolamide 250 mg - lan 1050 round white
exemestane 25 mg - 2858 round white
anastrozole 1 mg - m 34 round white
desloratadine 5 mg - m d17 round red
olmesartan medoxomil 40 mgamlodipine besylate 10 mghydrochlorothiazide 12.5 mg - c55 round red
demeclocycline hydrochloride 150 mg - c 115 round pink
letrozole 2.5 mg - 54 753 round white
sumatriptan succinate 50 mg - m s7 round white
repaglinide 2 mg - 747 c round pink
prochlorperazine maleate 5 mg - 93 9643 round yellow
folic acid 1 mg - 3162 v round yellow
midodrine hydrochloride 10 mg - us 10 213 round purple
felodipine 2.5 mg - mp 771 round green
ropinirole hydrochloride 12 mg - m re12 round green
hydroxyzine hydrochloride 10 mg - 3615 v round orange
labetalol hydrochloride 200 mg - watson 606 round white
- b 143 round white
paroxetine hydrochloride hemihydrate 12.5 mg - m p3 round white
albuterol sulfate 2 mg - mp 47 round white
donepezil hydrochloride 10 mg - zf 15 round white
imipramine hydrochloride 10 mg - mp 4 round yellow
timolol maleate 5 mg - m 55 round green
amlodipine besylate 10 mg - z 5 round white
anastrozole 1 mg - teva a10 round white
morphine sulfate 30 mg - abg 30 round purple
bupropion hydrochloride 100 mg - wpi 858 round white
medroxyprogesterone acetate 5 mg - 555 873 b round white
furosemide 20 mg - 54 840 round white
hydroxyzine hydrochloride 10 mg - a 75 round white
hydroxychloroquine sulfate 200 mg - ww28 round white
hydroxyzine hydrochloride 10 mg - k 10 round white
captopril 100 mg - m c4 round white
morphine sulfate 15 mg - e652 15 round blue
dicyclomine hydrochloride 20 mg - ww 27 round blue
trihexyphenidyl hydrochloride 5 mg - dan dan 5337 round white
nifedipine 90 mg - 90 adalat cc round pink
orphenadrine citrate 100 mg - nl4 round white
desogestrel 0.15 mgethinyl estradiol 0.025 mg - b 335 round pink
amlodipine besylate 10 mgolmesartan medoxomil 40 mg - c77 round red
pilocarpine hydrochloride 7.5 mg - lci 1407 round blue
nifedipine 30 mg - m ne 30 round white
amlodipine besylate 5 mg - 2109 v round white
progesterone 100 mg - ak round pink
oxybutynin chloride 5 mg - 4853 v round blue
amlodipine besylate 2.5 mg - 237 ig round white
lovastatin 60 mg - 60 round orange
pravastatin sodium 40 mg - apo pra 40 round green
promethazine hydrochloride 50 mg - gg 235 round pink
hydrochlorothiazide 25 mg - lci 1413 round orange
diclofenac sodium 50 mg - gg738 round brown
amitriptyline hydrochloride 25 mg - gg44 round green
zafirlukast 10 mg - r 625 round pink
clonidine hydrochloride 0.2 mg - mp 658 round white
acarbose 25 mg - p210 25 round white
- deltasone 2.5 round pink
lisinopril 20 mghydrochlorothiazide 12.5 mg - rx537 round yellow
desipramine hydrochloride 50 mg - norpramin 50 round green
diclofenac sodium 75 mg - r 551 round white
drospirenone 3 mgethinyl estradiol 0.03 mg - do round yellow
nitroglycerin 0.6 mg - n 6 round white
nitroglycerin 0.4 mg - n 4 round white
nitroglycerin 0.3 mg - n 3 round white
Go PRO for all pill images
Patients should be counseled that oral contraceptives do not protect against transmission of HIV (AIDS) and other sexually transmitted diseases (STDs) such as chlamydia, genital herpes, genital warts, gonorrhea, hepatitis B, and syphilis.
Description
21 orange active tablets each containing 0.1 mg of levonorgestrel, d(-)-13ő≤-ethyl-17őĪ-ethinyl-17ő≤-hydroxygon-4-en-3-one, a totally synthetic progestogen, and 0.02 mg of ethinyl estradiol, 17őĪ-ethinyl-1,3,5(10)-estratriene-3,17ő≤-diol. The inactive ingredients present are FD&C Yellow #5 Aluminum Lake, FD&C Yellow #6 Aluminum Lake, FD&C Red #40 Aluminum Lake, titanium dioxide, polyvinyl alchol, talc, macrogol/polyethylene glycol 3350 NF, lecithin (soya), iron oxide black, lactose monohydrate, magnesium stearate and pregelatinized corn starch.
7 white tablets, each containing the following inactive ingredients: titanium dioxide, polydextrose, hypromellose, triacetin, macrogol/polyethylene glycol 8000, lactose monohydrate, magnesium stearate and pregelatinized corn starch.

Clinical Pharmacology
Mode of Action
Combination oral contraceptives act by suppression of gonadotropins. Although the primary mechanism of this action is inhibition of ovulation, other alterations include changes in the cervical mucus (which increase the difficulty of sperm entry into the uterus) and the endometrium (which reduce the likelihood of implantation).
Pharmacokinetics
Absorption
No specific investigation of the absolute bioavailability of FALMINA (Levonorgestrel and Ethinyl Estradiol Tablets, USP) in humans has been conducted. However, literature indicates that levonorgestrel is rapidly and completely absorbed after oral administration (bioavailability about 100%) and is not subject to first-pass metabolism. Ethinyl estradiol is rapidly and almost completely absorbed from the gastrointestinal tract but, due to first-pass metabolism in gut mucosa and liver, the bioavailability of ethinyl estradiol is between 38% and 48%.
After a single dose of levonorgestrel and ethinyl estradiol tablets to 22 women under fasting conditions, maximum serum concentrations of levonorgestrel are 2.8 ¬Ī 0.9 ng/mL (mean ¬Ī SD) at 1.6 ¬Ī 0.9 hours. At steady state, attained from day 19 onwards, maximum levonorgestrel concentrations of 6.0 ¬Ī 2.7 ng/mL are reached at 1.5 ¬Ī 0.5 hours after the daily dose. The minimum serum levels of levonorgestrel at steady state are 1.9 ¬Ī 1.0 ng/mL. Observed levonorgestrel concentrations increased from day 1 (single dose) to days 6 and 21 (multiple doses) by 34% and 96%, respectively (Figure 1).
Unbound levonorgestrel concentrations increased from day 1 to days 6 and 21 by 25% and 83%, respectively. The kinetics of total levonorgestrel are non-linear due to an increase in binding of levonorgestrel to sex hormone binding globulin (SHBG), which is attributed to increased SHBG levels that are induced by the daily administration of ethinyl estradiol.
Following a single dose, maximum serum concentrations of ethinyl estradiol of 62 ¬Ī 21 pg/mL are reached at 1.5 ¬Ī 0.5 hours. At steady state, attained from at least day 6 onwards, maximum concentrations of ethinyl estradiol were 77 ¬Ī 30 pg/mL and were reached at 1.3 ¬Ī 0.7 hours after the daily dose. The minimum serum levels of ethinyl estradiol at steady state are 10.5 ¬Ī 5.1 pg/mL. Ethinyl estradiol concentrations did not increase from days 1 to 6, but did increase by 19% from days 1 to 21 (Figure 1).

FIGURE 1: Mean (SE) levonorgestrel and ethinyl estradiol serum concentrations in 22 subjects receiving 100 mcg levonorgestrel and 20 mcg ethinyl estradiol
Table 1 provides a summary of levonorgestrel and ethinyl estradiol pharmacokinetic parameters.
Distribution
Levonorgestrel in serum is primarily bound to SHBG. Ethinyl estradiol is about 97% bound to plasma albumin. Ethinyl estradiol does not bind to SHBG, but induces SHBG synthesis.
Metabolism
Levonorgestrel: The most important metabolic pathway occurs in the reduction of the őĒ4-3-oxo group and hydroxylation at positions 2őĪ, 1ő≤, and 16ő≤, followed by conjugation. Most of the metabolites that circulate in the blood are sulfates of 3őĪ, 5ő≤-tetrahydro-levonorgestrel, while excretion occurs predominantly in the form of glucuronides. Some of the parent levonorgestrel also circulates as 17ő≤-sulfate. Metabolic clearance rates may differ among individuals by several-fold, and this may account in part for the wide variation observed in levonorgestrel concentrations among users.
Ethinyl estradiol: Cytochrome P450 enzymes (CYP3A4) in the liver are responsible for the 2-hydroxylation that is the major oxidative reaction. The 2-hydroxy metabolite is further transformed by methylation and glucuronidation prior to urinary and fecal excretion. Levels of Cytochrome P450 (CYP3A) vary widely among individuals and can explain the variation in rates of ethinyl estradiol 2-hydroxylation. Ethinyl estradiol is excreted in the urine and feces as glucuronide and sulfate conjugates, and undergoes enterohepatic circulation.
Excretion
The elimination half-life for levonorgestrel is approximately 36 ¬Ī 13 hours at steady state. Levonorgestrel and its metabolites are primarily excreted in the urine (40% to 68%) and about 16% to 48% are excreted in feces. The elimination half-life of ethinyl estradiol is 18 ¬Ī 4.7 hours at steady state.
Special Populations
Race
Based on the pharmacokinetic study with levonorgestrel and ethinyl estradiol tablets, there are no apparent differences in pharmacokinetic parameters among women of different races.
Hepatic insufficiency
No formal studies have evaluated the effect of hepatic disease on the disposition of FALMINA (levonorgestrel and ethinyl estradiol tablets USP). However, steroid hormones may be poorly metabolized in patients with impaired liver function.
Renal insufficiency
No formal studies have evaluated the effect of renal disease on the disposition of FALMINA.
Drug-drug interactions
See PRECAUTIONS section - Drug Interactions
Indications And Usage
FALMINA is indicated for the prevention of pregnancy in women who elect to use oral contraceptives as a method of contraception.
Oral contraceptives are highly effective. Table 2 uls the typical accidental pregnancy rates for users of combination oral contraceptives and other methods of contraception. The efficacy of these contraceptive methods, except sterilization, the IUD, and Norplant¬ģ System, depends upon the reliability with which they are used. Correct and consistent use of methods can result in lower failure rates.

Emergency Contraceptive Pills: The FDA has concluded that certain combined oral contraceptives containing ethinyl estradiol and norgestrel or levonorgestrel are safe and effective for use as postcoital emergency contraception. Treatment initiated within 72 hours after unprotected intercourse reduces the risk of pregnancy by at least 75%.9
Lactation Amenorrhea Method: LAM is a highly effective, temporary method of contraception.10
Source: Trussell J. Contraceptive efficacy. In: Hatcher RA, Trussell J, Stewart F, Cates W, Stewart GK, Kowel D, Guest F. Contraceptive Technology: Seventeenth Revised Edition. New York NY: Irvington Publishers; 1998.
1. Among typical couples who initiate use of a method (not necessarily for the first time), the percentage who experience an accidental pregnancy during the first year if they do not stop use for any other reason.
2. Among couples who initiate use of a method (not necessarily for the first time) and who use it perfectly (both consistently and correctly), the percentage who experience an accidental pregnancy during the first year if they do not stop use for any other reason.
3. Among couples attempting to avoid pregnancy, the percentage who continue to use a method for one year.
4. The proportion of women who become pregnant in columns (2) and (3) are based on data from populations where contraception is not used and from women who cease using contraception in order to become pregnant. Among such populations, about 89% become pregnant within one year. This estimate was lowered slightly (to 85%) to represent the proportion who would become pregnant within one year among women now relying on reversible methods of contraception if they abandoned contraception altogether.
5. Foams, creams, gels, vaginal suppositories, and vaginal film.
6. Cervical mucus (ovulation) method supplemented by calendar in the pre-ovulatory and basal body temperature in the post-ovulatory phases.
7. With spermicidal cream or jelly.
8. Without spermicides.
9. The treatment schedule is one dose within 72 hours after unprotected intercourse, and a second dose 12 hours after the first dose. The FDA has declared the following dosage regimens of oral contraceptives to be safe and effective for emergency contraception: for tablets containing 50 mcg of ethinyl estradiol and 500 mcg of norgestrel 1 dose is 2 tablets; for tablets containing 20 mcg of ethinyl estradiol and 100 mcg of levonorgestrel 1 dose is 5 tablets; for tablets containing 30 mcg of ethinyl estradiol and 150 mcg of levonorgestrel 1 dose is 4 tablets.
10. However, to maintain effective protection against pregnancy, another method of contraception must be used as soon as menstruation resumes, the frequency or duration of breastfeeds is reduced, bottle feeds are introduced, or the baby reaches 6 months of age.
In a clinical trial with levonorgestrel and ethinyl estradiol tablets, 1,477 subjects had 7,720 cycles of use and a total of 5 pregnancies were reported. This represents an overall pregnancy rate of 0.84 per 100 woman-years. This rate includes patients who did not take the drug correctly. One or more pills were missed during 1,479 (18.8%) of the 7,870 cycles; thus all tablets were taken during 6,391 (81.2%) of the 7,870 cycles. Of the total 7,870 cycles, a total of 150 cycles were excluded from the calculation of the Pearl index due to the use of backup contraception and/or missing 3 or more consecutive pills.
Contraindications
Combination oral contraceptives should not be used in women with any of the following conditions:
Thrombophlebitis or thromboembolic disorders
A history of deep-vein thrombophlebitis or thromboembolic disorders
Cerebrovascular or coronary artery disease (current or past history)
Valvular heart disease with thrombogenic complications
Thrombogenic rhythm disorders
Hereditary or acquired thrombophilias
Major surgery with prolonged immobilization
Diabetes with vascular involvement
Headaches with focal neurological symptoms
Uncontrolled hypertension
Current diagnosis of, or history of, breast cancer, which may be hormone-sensitive
Undiagnosed abnormal genital bleeding
Cholestatic jaundice of pregnancy or jaundice with prior pill use
Hepatic adenomas or carcinomas, or active liver disease
Known or suspected pregnancy
Hypersensitivity to any of the components of FALMINA
Women who are receiving Hepatitis C drug combinations containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, due to the potential for alanine aminotransferase (ALT) elevations (see WARNINGS, RISK OF LIVER ENZYME ELEVATIONS WITH CONCOMITANT HEPATITIS C TREATMENT ).
Warnings
Cigarette smoking increases the risk of serious cardiovascular side effects from oral-contraceptive use. This risk increases with age and with the extent of smoking (in epidemiologic studies, 15 or more cigarettes per day was associated with a significantly increased risk ) and is quite marked in women over 35 years of age. Women who use oral contraceptives should be strongly advised not to smoke.
The use of oral contraceptives is associated with increased risks of several serious conditions including venous and arterial thrombotic and thromboembolic events (such as myocardial infarction, thromboembolism, and stroke), hepatic neoplasia, gallbladder disease, and hypertension, although the risk of serious morbidity or mortality is very small in healthy women without underlying risk factors. The risk of morbidity and mortality increases significantly in the presence of other underlying risk factors such as certain inherited or acquired thrombophilias, hypertension, hyperlipidemias, obesity, diabetes, and surgery or trauma with increased risk of thrombosis (see CONTRAINDICATIONS).
Practitioners prescribing oral contraceptives should be familiar with the following information relating to these risks.
The information contained in this package insert is principally based on studies carried out in patients who used oral contraceptives with higher doses of estrogens and progestogens than those in common use today. The effect of long-term use of the oral contraceptives with lower doses of both estrogens and progestogens remains to be determined.
Throughout this labeling, epidemiological studies reported are of two types: retrospective or case control studies and prospective or cohort studies. Case control studies provide a measure of the relative risk of disease, namely, a ratio of the incidence of a disease among oral-contraceptive users to that among nonusers. The relative risk does not provide information on the actual clinical occurrence of a disease. Cohort studies provide a measure of attributable risk, which is the difference in the incidence of disease between oral-contraceptive users and nonusers. The attributable risk does provide information about the actual occurrence of a disease in the population. For further information, the reader is referred to a text on epidemiological methods.
1. Thromboembolic Disorders and Other Vascular Problems
a. Myocardial infarction
An increased risk of myocardial infarction has been attributed to oral-contraceptive use. This risk is primarily in smokers or women with other underlying risk factors for coronary-artery disease such as hypertension, hypercholesterolemia, morbid obesity, and diabetes. The relative risk of heart attack for current oral-contraceptive users has been estimated to be two to six. The risk is very low under the age of 30.
Smoking in combination with oral-contraceptive use has been shown to contribute substantially to the incidence of myocardial infarction in women in their mid-thirties or older with smoking accounting for the majority of excess cases. Mortality rates associated with circulatory disease have been shown to increase substantially in smokers over the age of 35 and nonsmokers over the age of 40 (Figure 2) among women who use oral contraceptives.
Oral contraceptives may compound the effects of well-known risk factors, such as hypertension, diabetes, hyperlipidemias, age and obesity. In particular, some progestogens are known to decrease HDL cholesterol and cause glucose intolerance, while estrogens may create a state of hyperinsulinism. Oral contraceptives have been shown to increase blood pressure among users (see section 10 in WARNINGS ). Similar effects on risk factors have been associated with an increased risk of heart disease. Oral contraceptives must be used with caution in women with cardiovascular disease risk factors.
b. Venous thrombosis and thromboembolism
An increased risk of venous thromboembolic and thrombotic disease associated with the use of oral contraceptives is well established. Case control studies have found the relative risk of users compared to non-users to be 3 for the first episode of superficial venous thrombosis, 4 to 11 for deep-vein thrombosis or pulmonary embolism, and 1.5 to 6 for women with predisposing conditions for venous thromboembolic disease. Cohort studies have shown the relative risk to be somewhat lower, about 3 for new cases and about 4.5 for new cases requiring hospitalization. The approximate incidence of deep-vein thrombosis and pulmonary embolism in users of low dose (<50 mcg ethinyl estradiol) combination oral contraceptives is up to 4 per 10,000 woman years compared to 0.5-3 per 10,000 woman-years for non-users. However, the incidence is less than that associated with pregnancy (6 per 10,000 woman-years). The excess risk is highest during the first year a woman ever uses a combined oral contraceptive. Venous thromboembolism may be fatal. The risk of thromboembolic disease due to oral contraceptives is not related to length of use and gradually disappears after pill use is stopped.
A two- to four-fold increase in relative risk of postoperative thromboembolic complications has been reported with the use of oral contraceptives. The relative risk of venous thrombosis in women who have predisposing conditions is twice that of women without such medical conditions. If feasible, oral contraceptives should be discontinued at least four weeks prior to and for two weeks after elective surgery of a type associated with an increase in risk of thromboembolism and during and following prolonged immobilization. Since the immediate postpartum period is also associated with an increased risk of thromboembolism, oral contraceptives should be started no earlier than four weeks after delivery in women who elect not to breast-feed or after a midtrimester pregnancy termination.
c. Cerebrovascular diseases
Oral contraceptives have been shown to increase both the relative and attributable risks of cerebrovascular events (thrombotic and hemorrhagic strokes), although, in general, the risk is greatest among older (>35 years), hypertensive women who also smoke. Hypertension was found to be a risk factor for both users and nonusers, for both types of strokes, while smoking interacted to increase the risk for hemorrhagic strokes.
In a large study, the relative risk of thrombotic strokes has been shown to range from 3 for normotensive users to 14 for users with severe hypertension. The relative risk of hemorrhagic stroke is reported to be 1.2 for nonsmokers who used oral contraceptives, 2.6 for smokers who did not use oral contraceptives, 7.6 for smokers who used oral contraceptives, 1.8 for normotensive users and 25.7 for users with severe hypertension. The attributable risk is also greater in older women. Oral contraceptives also increase the risk for stroke in women with other underlying risk factors such as certain inherited or acquired thrombophilias. Women with migraine (particularly migraine/headaches with focal neurological symptoms, see CONTRAINDICATIONS ) who take combination oral contraceptives may be at an increased risk of stroke.
d. Dose-related risk of vascular disease from oral contraceptives
A positive association has been observed between the amount of estrogen and progestogen in oral contraceptives and the risk of vascular disease. A decline in serum high-density lipoproteins (HDL) has been reported with many progestational agents. A decline in serum high-density lipoproteins has been associated with an increased incidence of ischemic heart disease. Because estrogens increase HDL cholesterol, the net effect of an oral contraceptive depends on a balance achieved between doses of estrogen and progestogen and the nature and absolute amount of progestogen used in the contraceptive. The amount of both hormones should be considered in the choice of an oral contraceptive.
Minimizing exposure to estrogen and progestogen is in keeping with good principles of therapeutics. For any particular estrogen/progestogen combination, the dosage regimen prescribed should be one which contains the least amount of estrogen and progestogen that is compatible with a low failure rate and the needs of the individual patient. New acceptors of oral-contraceptive agents should be started on preparations containing the lowest estrogen content which is judged appropriate for the individual patient
e. Persistence of risk of vascular disease
There are two studies which have shown persistence of risk of vascular disease for ever-users of oral contraceptives. In a study in the United States, the risk of developing myocardial infarction after discontinuing oral contraceptives persists for at least 9 years for women 40 to 49 years who had used oral contraceptives for five or more years, but this increased risk was not demonstrated in other age groups.
In another study in Great Britain, the risk of developing cerebrovascular disease persisted for at least 6 years after discontinuation of oral contraceptives, although excess risk was very small. However, both studies were performed with oral contraceptive formulations containing 50 mcg or higher of estrogens.
2. Estimates of Mortality from Contraceptive Use
One study gathered data from a variety of sources which have estimated the mortality rate associated with different methods of contraception at different ages (Table 3). These estimates include the combined risk of death associated with contraceptive methods plus the risk attributable to pregnancy in the event of method failure. Each method of contraception has its specific benefits and risks. The study concluded that with the exception of oral-contraceptive users 35 and older who smoke and 40 and older who do not smoke, mortality associated with all methods of birth control is less than that associated with childbirth. The observation of a possible increase in risk of mortality with age for oral-contraceptive users is based on data gathered in the 1970's‚ÄĒbut not reported until 1983. However, current clinical practice involves the use of lower estrogen dose formulations combined with careful restriction of oral contraceptive use to women who do not have the various risk factors uled in this labeling.
Because of these changes in practice and, also, because of some limited new data which suggest that the risk of cardiovascular disease with the use of oral contraceptives may now be less than previously observed, the Fertility and Maternal Health Drugs Advisory Committee was asked to review the topic in 1989. The Committee concluded that although cardiovascular disease risks may be increased with oral-contraceptive use after age 40 in healthy nonsmoking women (even with the newer low-dose formulations), there are greater potential health risks associated with pregnancy in older women and with the alternative surgical and medical procedures which may be necessary if such women do not have access to effective and acceptable means of contraception.
Therefore, the Committee recommended that the benefits of oral-contraceptive use by healthy nonsmoking women over 40 may outweigh the possible risks. Of course, older women, as all women who take oral contraceptives, should take the lowest possible dose formulation that is effective.

3. Malignant Neoplasms
Breast Cancer
FALMINA is contraindicated in females who currently have or have had breast cancer because breast cancer may be hormonally sensitive [see Contraindications (4)]. Epidemiology studies have not found a consistent association between use of combined oral contraceptives (COCs) and breast cancer risk. Studies do not show an association between ever (current or past) use of COCs and risk of breast cancer. However, some studies report a small increase in the risk of breast cancer among current or recent users (<6 months since last use) and current users with longer duration of COC use [see ADVERSE REACTIONS].
Cervical Cancer
Some studies suggest that oral contraceptive use has been associated with an increase in the risk of cervical intraepithelial neoplasia or invasive cervical cancer in some populations of women. However, there continues to be controversy about the extent to which such findings may be due to differences in sexual behavior and other factors.
4. Hepatic Neoplasia
Benign hepatic adenomas are associated with oral-contraceptive use, although the incidence of these benign tumors is rare in the United States. Indirect calculations have estimated the attributable risk to be in the range of 3.3 cases/100,000 for users, a risk that increases after four or more years of use. Rupture of rare, benign, hepatic adenomas may cause death through intra-abdominal hemorrhage.
Studies from Britain have shown an increased risk of developing hepatocellular carcinoma in long-term (>8 years) oral-contraceptive users. However, these cancers are extremely rare in the U.S. and the attributable risk (the excess incidence) of liver cancers in oral-contraceptive users approaches less than one per million users.
5. Risk of Liver Enzyme Elevations with Concomitant Hepatitis C Treatment
During clinical trials with the Hepatitis C combination drug regimen that contains ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, ALT elevations greater than 5 times the upper limit of normal (ULN), including some cases greater than 20 times the ULN, were significantly more frequent in women using ethinyl estradiol-containing medications such as COCs. Discontinue FALMINA prior to starting therapy with the combination drug regimen ombitasvir/paritaprevir/ritonavir, with or without dasabuvir (see CONTRAINDICATIONS). FALMINA can be restarted approximately 2 weeks following completion of treatment with the combination drug regimen.
6. Ocular Lesions
There have been clinical case reports of retinal thrombosis associated with the use of oral contraceptives that may lead to partial or complete loss of vision. Oral contraceptives should be discontinued if there is unexplained partial or complete loss of vision; onset of proptosis or diplopia; papilledema; or retinal vascular lesions. Appropriate diagnostic and therapeutic measures should be undertaken immediately.
7. Oral-Contraceptive Use Before or During Early Pregnancy
Extensive epidemiological studies have revealed no increased risk of birth defects in infants born to women who have used oral contraceptives prior to pregnancy. Studies also do not suggest a teratogenic effect, particularly insofar as cardiac anomalies and limb-reduction defects are concerned, when taken inadvertently during early pregnancy (see CONTRAINDICATIONS section).
The administration of oral contraceptives to induce withdrawal bleeding should not be used as a test for pregnancy. Oral contraceptives should not be used during pregnancy to treat threatened or habitual abortion.
It is recommended that for any patient who has missed two consecutive periods, pregnancy should be ruled out. If the patient has not adhered to the prescribed schedule, the possibility of pregnancy should be considered at the time of the first missed period. Oral-contraceptive use should be discontinued if pregnancy is confirmed.
8. Gallbladder Disease
Combination oral contraceptives may worsen existing gallbladder disease and may accelerate the development of this disease in previously asymptomatic women. Earlier studies have reported an increased lifetime relative risk of gallbladder surgery in users of oral contraceptives and estrogens. More recent studies, however, have shown that the relative risk of developing gallbladder disease among oral-contraceptive users may be minimal. The recent findings of minimal risk may be related to the use of oral-contraceptive formulations containing lower hormonal doses of estrogens and progestogens.
9. Carbohydrate and Lipid Metabolic Effects
Oral contraceptives have been shown to cause glucose intolerance in a significant percentage of users. Oral contraceptives containing greater than 75 mcg of estrogens cause hyper-insulinism, while lower doses of estrogen cause less glucose intolerance. Progestogens increase insulin secretion and create insulin resistance, this effect varying with different progestational agents. However, in the nondiabetic woman, oral contraceptives appear to have no effect on fasting blood glucose. Because of these demonstrated effects, prediabetic and diabetic women should be carefully observed while taking oral contraceptives.
A small proportion of women will have persistent hypertriglyceridemia while on the pill. As discussed earlier (see WARNINGS, 1a. and 1d.; PRECAUTIONS,3 .), changes in serum triglycerides and lipoprotein levels have been reported in oral-contraceptive users.
10. Elevated Blood Pressure
An increase in blood pressure has been reported in women taking oral contraceptives and this increase is more likely in older oral-contraceptive users and with continued use. Data from the Royal College of General Practitioners and subsequent randomized trials have shown that the incidence of hypertension increases with increasing quantities of progestogens.
Women with a history of hypertension or hypertension-related diseases, or renal disease should be encouraged to use another method of contraception. If women with hypertension elect to use oral contraceptives, they should be monitored closely and if significant elevation of blood pressure occurs, oral contraceptives should be discontinued (See CONTRAINDICATIONS section). For most women, elevated blood pressure will return to normal after stopping oral contraceptives, and there is no difference in the occurrence of hypertension among ever- and never-users.
11. Headache
The onset or exacerbation of migraine or development of headache with a new pattern that is recurrent, persistent, or severe requires discontinuation of oral contraceptives and evaluation of the cause. (See WARNINGS, 1c . and CONTRAINDICATIONS .)
12. Bleeding Irregularities
Breakthrough bleeding and spotting are sometimes encountered in patients on oral contraceptives, especially during the first three months of use. The type and dose of progestogen may be important. If bleeding persists or recurs, nonhormonal causes should be considered and adequate diagnostic measures taken to rule out malignancy or pregnancy in the event of breakthrough bleeding, as in the case of any abnormal vaginal bleeding. If pathology has been excluded, time or a change to another formulation may solve the problem. In the event of amenorrhea, pregnancy should be ruled out.
Some women may encounter post-pill amenorrhea or oligomenorrhea (possibly with anovulation), especially when such a condition was preexistent.
13. Ectopic Pregnancy
Ectopic as well as intrauterine pregnancy may occur in contraceptive failures.
Precautions
1. General
Patients should be counseled that oral contraceptives do not protect against transmission of HIV (AIDS) and other sexually transmitted diseases (STDs) such as chlamydia, genital herpes, genital warts, gonorrhea, hepatitis B, and syphilis.
This product contains FD&C Yellow No. 5 (tartrazine) which may cause allergic-type reactions (including bronchial asthma) in certain susceptible persons. Although the overall incidence of FD&C Yellow No. 5 (tartrazine) sensitivity in the general population is low, it is frequently seen in patients who also have aspirin hypersensitivity.
2. Physical Examination and Follow-Up
A periodic personal and family medical history and complete physical examination are appropriate for all women, including women using oral contraceptives. The physical examination, however, may be deferred until after initiation of oral contraceptives if requested by the woman and judged appropriate by the clinician. The physical examination should include special reference to blood pressure, breasts, abdomen and pelvic organs, including cervical cytology, and relevant laboratory tests. In case of undiagnosed, persistent or recurrent abnormal vaginal bleeding, appropriate diagnostic measures should be conducted to rule out malignancy. Women with a strong family history of breast cancer or who have breast nodules should be monitored with particular care.
3. Lipid Disorders
Women who are being treated for hyperlipidemias should be followed closely if they elect to use oral contraceptives. Some progestogens may elevate LDL levels and may render the control of hyperlipidemias more difficult. (See WARNINGS,1a. , 1d. , and 9 .)
A small proportion of women will have adverse lipid changes while taking oral contraceptives. Nonhormonal contraception should be considered in women with uncontrolled dyslipidemias. Persistent hypertriglyceridemia may occur in a small population of combination oral contraceptive users. Elevations of plasma triglycerides may lead to pancreatitis and other complications.
4. Liver Function
If jaundice develops in any woman receiving such drugs, the medication should be discontinued. Steroid hormones may be poorly metabolized in patients with impaired liver function.
5. Fluid Retention
Oral contraceptives may cause some degree of fluid retention. They should be prescribed with caution, and only with careful monitoring, in patients with conditions which might be aggravated by fluid retention.
6. Emotional Disorders
Patients becoming significantly depressed while taking oral contraceptives should stop the medication and use an alternate method of contraception in an attempt to determine whether the symptom is drug related. Women with a history of depression should be carefully observed and the drug discontinued if depression recurs to a serious degree.
7. Contact Lenses
Contact-lens wearers who develop visual changes or changes in lens tolerance should be assessed by an ophthalmologist.
8. Gastrointestinal
Diarrhea and/or vomiting may reduce hormone absorption resulting in decreased serum concentrations.
9. Drug Interactions
Concomitant Use with HCV Combination Therapy-Liver Enzyme Elevation
Do not co-administer Falmina with HCV drug combinations containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, due to potential for ALT elevations (see WARINGS, RISK OF LIVER ENZYME ELEVATIONS WITH CONCOMITANT HEPATITIS C TREATMENT ).
Changes in Contraceptive Effectiveness Associated with Coadministration of Other Products:
Contraceptive effectiveness may be reduced when hormonal contraceptives are coadministered with antibiotics, anticonvulsants, and other drugs that increase the metabolism of contraceptive steroids. This could result in unintended pregnancy or breakthrough bleeding. Examples include rifampin, rifabutin, barbiturates, primidone, phenylbutazone, phenytoin, dexamethasone, carbamazepine, felbamate, oxcarbazepine, topiramate, griseofulvin, and modafinil. In such cases a back-up nonhormonal method of birth control should be considered.
Several cases of contraceptive failure and breakthrough bleeding have been reported in the literature with concomitant administration of antibiotics such as ampicillin and other penicillins, and tetracyclines. However, clinical pharmacology studies investigating drug interactions between combined oral contraceptives and these antibiotics have reported inconsistent results.
Several of the anti-HIV protease inhibitors have been studied with co-administration of oral combination hormonal contraceptives; significant changes (increase and decrease) in the plasma levels of the estrogen and progestin have been noted in some cases. The safety and efficacy of oral contraceptive products may be affected with coadministration of anti-HIV protease inhibitors. Healthcare providers should refer to the label of the individual anti-HIV protease inhibitors for further drug-drug interaction information.
Herbal products containing St. John's Wort (Hypericum perforatum) may induce hepatic enzymes (cytochrome P 450) and p-glycoprotein transporter and may reduce the effectiveness of contraceptive steroids. This may also result in breakthrough bleeding.
Increase in Plasma Levels Associated with Co-Administered Drugs:
Co-administration of atorvastatin and certain oral contraceptives containing ethinyl estradiol increases AUC values for ethinyl estradiol by approximately 20%. Ascorbic acid and acetaminophen increase the bioavailability of ethinyl estradiol since these drugs act as competitive inhibitors for sulfation of ethinyl estradiol in the gastrointestinal wall, a known pathway of elimination for ethinyl estradiol. CYP 3A4 inhibitors such as indinavir, itraconazole, ketoconazole, fluconazole, and troleandomycin may increase plasma hormone levels. Troleandomycin may also increase the risk of intrahepatic cholestasis during coadministration with combination oral contraceptives.
Changes in Plasma Levels of Co-Administered Drugs:
Combination hormonal contraceptives containing some synthetic estrogens (eg, ethinyl estradiol) may inhibit the metabolism of other compounds. Increased plasma concentrations of cyclosporin, prednisolone and other corticosteroids, and theophylline have been reported with concomitant administration of oral contraceptives. Decreased plasma concentrations of acetaminophen and increased clearance of temazepam, salicylic acid, morphine, and clofibric acid, due to induction of conjugation (particularly glucuronidation), have been noted when these drugs were administered with oral contraceptives.
The prescribing information of concomitant medications should be consulted to identify potential interactions.
10. Interactions with Laboratory Tests
Certain endocrine- and liver-function tests and blood components may be affected by oral contraceptives:
a. Increased prothrombin and factors VII, VIII, IX, and X; decreased antithrombin 3; increased norepinephrine-induced platelet aggregability.
b. Increased thyroid-binding globulin (TBG) leading to increased circulating total thyroid hormone, as measured by protein-bound iodine (PBI), T4 by column or by radioimmunoassay. Free T3 resin uptake is decreased, reflecting the elevated TBG; free T4 concentration is unaltered.
c. Other binding proteins may be elevated in serum i.e., corticosteroid binding globulin (CBG), sex hormone-binding globulins (SHBG) leading to increased levels of total circulating corticosteroids and sex steroids respectively. Free or biologically active hormone concentrations are unchanged.
d. Triglycerides may be increased and levels of various other lipids and lipoproteins may be affected.
e. Glucose tolerance may be decreased.
f. Serum folate levels may be depressed by oral-contraceptive therapy. This may be of clinical significance if a woman becomes pregnant shortly after discontinuing oral contraceptives.
11. Carcinogenesis
See WARNINGS section.
12. Pregnancy
See CONTRAINDICATIONS and WARNINGS sections.
13. Nursing Mothers
Small amounts of oral-contraceptive steroids and/or metabolites have been identified in the milk of nursing mothers, and a few adverse effects on the child have been reported, including jaundice and breast enlargement. In addition, combination oral contraceptives given in the postpartum period may interfere with lactation by decreasing the quantity and quality of breast milk. If possible, the nursing mother should be advised not to use combination oral contraceptives but to use other forms of contraception until she has completely weaned her child.
14. Pediatric Use
Safety and efficacy of levonorgestrel and ethinyl estradiol tablets have been established in women of reproductive age. Safety and efficacy are expected to be the same for postpubertal adolescents under the age of 16 and for users 16 years and older. Use of levonorgestrel and ethinyl estradiol tablets before menarche is not indicated.
15. Geriatric Use
Levonorgestrel and ethinyl estradiol tablets have not been studied in women over 65 years of age and is not indicated in this population.
16. Information for the Patient
See Patient Labeling Printed Below.
Adverse Reactions
To report SUSPECTED ADVERSE REACTIONS, contact Northstar Rx LLC at 1-800-206-7821 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch .
An increased risk of the following serious adverse reactions (see WARNINGS section for additional information) has been associated with the use of oral contraceptives:
Thromboembolic and thrombotic disorders and other vascular problems (including thrombophlebitis and venous thrombosis with or without pulmonary embolism, mesenteric thrombosis, arterial thromboembolism, myocardial infarction, cerebral hemorrhage, cerebral thrombosis), carcinoma of the reproductive organs and breasts, hepatic neoplasia (including hepatic adenomas or benign liver tumors), ocular lesions (including retinal vascular thrombosis), gallbladder disease, carbohydrate and lipid effects, elevated blood pressure, and headache including migraine.
Five studies that compared breast cancer risk between ever-users (current or past use) of COCs and never-users of COCs reported no association between ever use of COCs and breast cancer risk, with effect estimates ranging from 0.90 - 1.12 (Figure 3).
Three studies compared breast cancer risk between current or recent COC users (<6 months since last use) and never users of COCs (Figure 3). One of these studies reported no association between breast cancer risk and COC use. The other two studies found an increased relative risk of 1.19 - 1.33 with current or recent use. Both of these studies found an increased risk of breast cancer with current use of longer duration, with relative risks ranging from 1.03 with less than one year of COC use to approximately 1.4 with more than 8-10 years of COC use.
FIGURE 3: Relevant Studies of Risk of Breast Cancer with Combined Oral Contraceptives

RR = relative risk; OR = odds ratio; HR = hazard ratio. ‚Äúever COC‚ÄĚ are females with current or past COC use; ‚Äúnever COC use‚ÄĚ are females that never used COCs.
The following adverse reactions have been reported in patients receiving oral contraceptives and are believed to be drug related (alphabetically uled):
Acne
Amenorrhea
Anaphylactic/anaphylactoid reactions, including urticaria, angioedema, and severe reactions with respiratory and circulatory symptoms
Breast changes: tenderness, pain, enlargement, secretion
Budd-Chiari syndrome
Cervical erosion and secretion, change in
Cholestatic jaundice
Chorea, exacerbation of
Colitis
Contact lenses, intolerance to
Corneal curvature (steepening), change in
Dizziness
Edema/fluid retention
Erythema multiforme
Erythema nodosum
Gastrointestinal symptoms (such as abdominal pain, cramps, and bloating)
Hirsutism
Infertility after discontinuation of treatment, temporary
Lactation, diminution in, when given immediately postpartum
Libido, change in
Melasma/chloasma which may persist
Menstrual flow, change in
Mood changes, including depression
Nausea
Nervousness
Pancreatitis
Porphyria, exacerbation of
Rash (allergic)
Scalp hair, loss of
Serum folate levels, decrease in
Spotting
Systemic lupus erythematosus, exacerbation of
Unscheduled bleeding
Vaginitis, including candidiasis
Varicose veins, aggravation of
Vomiting
Weight or appetite (increase or decrease), change in
The following adverse reactions have been reported in users of oral contraceptives:
Cataracts
Cystitis-like syndrome
Dysmenorrhea
Hemolytic uremic syndrome
Hemorrhagic eruption
Optic neuritis, which may lead to partial or complete loss of vision
Premenstrual syndrome
Renal function, impaired
Overdosage
Symptoms of oral contraceptive overdosage in adults and children may include nausea, vomiting, and drowsiness/fatigue; withdrawal bleeding may occur in females. There is no specific antidote and further treatment of overdose, if necessary, is directed to the symptoms.
NONCONTRACEPTIVE HEALTH BENEFITS
The following non-contraceptive health benefits related to the use of oral contraceptives are supported by epidemiological studies which largely utilized oral-contraceptive formulations containing doses exceeding 0.035 mg of ethinyl estradiol or 0.05 mg of mestranol.
Effects on menses:
Increased menstrual cycle regularity
Decreased blood loss and decreased incidence of iron-deficiency anemia
Decreased incidence of dysmenorrhea
Effects related to inhibition of ovulation:
Decreased incidence of functional ovarian cysts
Decreased incidence of ectopic pregnancies
Effects from long-term use:
Decreased incidence of fibroadenomas and fibrocystic disease of the breast
Decreased incidence of acute pelvic inflammatory disease
Decreased incidence of endometrial cancer
Decreased incidence of ovarian cancer
Dosage And Administration
To achieve maximum contraceptive effectiveness, FALMINA‚ĄĘ (levonorgestrel and ethinyl estradiol tablets USP) must be taken exactly as directed and at intervals not exceeding 24 hours. The dosage of FALMINA is one orange tablet daily for 21 consecutive days, followed by one white inert tablet daily for 7 consecutive days, according to the prescribed schedule.
It is recommended that FALMINA tablets be taken at the same time each day.
During The First Cycle Of Use
The possibility of ovulation and conception prior to initiation of medication should be considered. The patient should be instructed to begin taking FALMINA on either the first Sunday after the onset of menstruation (Sunday Start) or on Day 1 of menstruation (Day 1 Start).
Sunday start:
The patient is instructed to begin taking FALMINA on the first Sunday after the onset of menstruation. If menstruation begins on a Sunday, the first tablet (orange) is taken that day. One orange tablet should be taken daily for 21 consecutive days, followed by one white inert tablet daily for 7 consecutive days. Withdrawal bleeding should usually occur within 3 days following discontinuation of orange tablets and may not have finished before the next pack is started. During the first cycle, contraceptive reliance should not be placed on FALMINA until an orange tablet has been taken daily for 7 consecutive days, and a nonhormonal back-up method of birth control should be used during those 7 days.
Day 1 start:
During the first cycle of medication, the patient is instructed to begin taking FALMINA during the first 24 hours of her period (day one of her menstrual cycle). One orange tablet should be taken daily for 21 consecutive days, followed by one white inert tablet daily for 7 consecutive days. Withdrawal bleeding should usually occur within 3 days following discontinuation of orange tablets and may not have finished before the next pack is started. If medication is begun on day one of the menstrual cycle, no back-up contraception is necessary. If FALMINA tablets are started later than day one of the first menstrual cycle or postpartum, contraceptive reliance should not be placed on FALMINA tablets until after the first 7 consecutive days of administration, and a nonhormonal back-up method of birth control should be used during those 7 days.
After the first cycle of use
The patient begins her next and all subsequent courses of tablets on the day after taking her last white tablet. She should follow the same dosing schedule: 21 days on orange tablets followed by 7 days on white tablets. If in any cycle the patient starts tablets later than the proper day, she should protect herself against pregnancy by using a nonhormonal back-up method of birth control until she has taken an orange tablet daily for 7 consecutive days.
Switching from another hormonal method of contraception
When the patient is switching from a 21-day regimen of tablets, she should wait 7 days after her last tablet before she starts FALMINA. She will probably experience withdrawal bleeding during that week. She should be sure that no more than 7 days pass after her previous 21-day regimen. When the patient is switching from a 28-day regimen of tablets, she should start her first pack of FALMINA on the day after her last tablet. She should not wait any days between packs. The patient may switch any day from a progestin-only pill and should begin FALMINA the next day. If switching from an implant or injection, the patient should start FALMINA on the day of implant removal or, if using an injection, the day the next injection would be due. In switching from a progestin-only pill, injection, or implant, the patient should be advised to use a nonhormonal back-up method of birth control for the first 7 days of tablet-taking.
If spotting or breakthrough bleeding occurs
If spotting or breakthrough bleeding occur, the patient is instructed to continue on the same regimen. This type of bleeding is usually transient and without significance; however, if the bleeding is persistent or prolonged, the patient is advised to consult her physician.
Risk of pregnancy if tablets are missed
While there is little likelihood of ovulation occurring if only one or two orange tablets are missed, the possibility of ovulation increases with each successive day that scheduled orange tablets are missed. Although the occurrence of pregnancy is unlikely if FALMINA is taken according to directions, if withdrawal bleeding does not occur, the possibility of pregnancy must be considered. If the patient has not adhered to the prescribed schedule (missed one or more tablets or started taking them on a day later than she should have), the probability of pregnancy should be considered at the time of the first missed period and appropriate diagnostic measures taken. If the patient has adhered to the prescribed regimen and misses two consecutive periods, pregnancy should be ruled out.
The risk of pregnancy increases with each active (orange) tablet missed. For additional patient instructions regarding missed tablets, see the WHAT TO DO IF YOU MISS PILLS section in the DETAILED PATIENT LABELING below.
Use after pregnancy, abortion or miscarriage
FALMINA may be initiated no earlier than day 28 postpartum in the nonlactating mother or after a second trimester abortion due to the increased risk for thromboembolism (see CONTRAINDICATIONS , WARNINGS , and PRECAUTIONS concerning thromboembolic disease). The patient should be advised to use a non-hormonal back-up method for the first 7 days of tablet taking.
FALMINA may be initiated immediately after a first trimester abortion or miscarriage. If the patient starts FALMINA immediately, back-up contraception is not needed.
How Supplied
FALMINA‚ĄĘ (Levonorgestrel and Ethinyl Estradiol Tablets, USP, 0.1 mg/0.02 mg) is available in a compact buler card (NDC 16714-359-01), containing 28 tablets arranged in 3 rows of 7 active tablets and 1 row of inert tablets, as follows:
21 active tablets: orange, round tablet debossed with "A3" on one side.
7 inert tablets: white, round tablet debossed with "P" on one side and "N" on the other side.
FALMINA Tablets are available in the following configuations:
Carton of 1 NDC 16714-359-02
Carton of 3 NDC 16714-359-03
Carton of 6 NDC 16714-359-04
Store at 20¬į to 25¬įC (68¬į to 77¬įF) [See USP controlled room temperature].

Manufactured for: Northstar Rx LLC
                                 Memphis TN 38141
Manufactured by: Novast Laboratories Ltd.
                                Nantong, China 226009
I 0017
Rev. B
Rev. 12/2023
Brief Summary Patient Package Insert
This product (like all oral contraceptives) is intended to prevent pregnancy. Oral contraceptives do not protect against transmission of HIV (AIDS) and other sexually transmitted diseases (STDs) such as chlamydia, genital herpes, genital warts, gonorrhea, hepatitis B, and syphilis.
Oral contraceptives, also known as "birth-control pills" or "the pill", are taken to prevent pregnancy, and when taken correctly, have a failure rate of approximately 1.0% per year (1 pregnancy per 100 women per year of use) when used without missing any pills. The average failure rate of large numbers of pill users is approximately 5% per year (5 pregnancies per 100 women per year of use) when women who miss pills are included. For most women oral contraceptives are also free of serious or unpleasant side effects. However, forgetting to take pills considerably increases the chances of pregnancy.
For the majority of women, oral contraceptives can be taken safely. But there are some women who are at high risk of developing certain serious diseases that can be life-threatening or may cause temporary or permanent disability or death. The risks associated with taking oral contraceptives increase significantly if you:
- smoke.
- have high blood pressure, diabetes, high cholesterol, or a tendency to form blood clots.
- have or have had clotting disorders, heart attack, stroke, angina pectoris, cancer of the breast or sex organs, jaundice, malignant or benign liver tumors, or major surgery with prolonged immobilization.
- have headaches with neurological symptoms.
You should not take the pill if you take any Hepatitis C drug combination containing ombitasvir/paritaprevir/ ritonavir, with or without dasabuvir. This may increase levels of the liver enzyme "alanine aminotransferase" (ALT) in the blood.
You should not take the pill if you suspect you are pregnant or have unexplained vaginal bleeding.
Although cardiovascular disease risks may be increased with oral-contraceptive use after age 40 in healthy, nonsmoking women, there are also greater potential health risks associated with pregnancy in older women.
Cigarette smoking increases the risk of serious adverse effects on the heart and blood vessels from oral-contraceptive use. This risk increases with age and with the amount of smoking (15 or more cigarettes per day has been associated with a significantly increased risk) and is quite marked in women over 35 years of age. Women who use oral contraceptives should not  smoke.
Most side effects of the pill are not serious. The most common such effects are nausea, vomiting, bleeding between menstrual periods, weight gain, breast tenderness, and difficulty wearing contact lenses. These side effects, especially nausea and vomiting, may subside within the first three months of use.
The serious side effects of the pill occur very infrequently, especially if you are in good health and do not smoke. However, you should know that the following medical conditions have been associated with or made worse by the pill:
1. Blood clots in the legs (thrombophlebitis) and lungs (pulmonary embolism), blockage or rupture of a blood vessel in the brain (stroke), blockage of blood vessels in the heart (heart attack and angina pectoris) or other organs of the body. As mentioned above, smoking increases the risk of heart attacks and strokes and subsequent serious medical consequences. Women with migraine also may be at increased risk of stroke with pill use.
2. Liver tumors, which may rupture and cause severe bleeding. A possible but not definite association has been found with the pill and liver cancer. However, liver cancers are extremely rare. The chance of developing liver cancer from using the pill is thus even rarer.
3. High blood pressure, although blood pressure usually returns to normal when the pill is stopped.
The symptoms associated with these serious side effects are discussed in the detailed leaflet given to you with your supply of pills. Notify your health-care provider if you notice any unusual physical disturbances while taking the pill. In addition, drugs such as rifampin, as well as some anticonvulsants and some antibiotics, herbal preparations containing St. John's Wort (Hypericum perforatum), and HIV/AIDS drugs may decrease oral-contraceptive effectiveness.
There may be slight increases in the risk of breast cancer among current users of hormonal birth control pills with longer duration of use of 8 years or more
Some studies have found an increase in the incidence of cancer of the cervix in women who use oral contraceptives. However, this finding may be related to factors other than the use of oral contraceptives.
Taking the pill provides some important non-contraceptive benefits. These include less painful menstruation, less menstrual blood loss and anemia, fewer pelvic infections, and fewer cancers of the ovary and the lining of the uterus.
Be sure to discuss any medical condition you may have with your health-care provider. Your health-care provider will take a medical and family history before prescribing oral contraceptives and will examine you. The physical examination may be delayed to another time if you request it and the health-care provider believes that it is appropriate to postpone it. You should be reexamined at least once a year while taking oral contraceptives. The detailed patient information leaflet gives you further information which you should read and discuss with your health-care provider.
HOW TO TAKE FALMINA
IMPORTANT POINTS TO REMEMBER
BEFORE YOU START TAKING FALMINA:
1. BE SURE TO READ THESE DIRECTIONS:
Before you start taking FALMINA.
And
Anytime you are not sure what to do.
2. THE RIGHT WAY TO TAKE THE PILL IS TO TAKE ONE PILL EVERY DAY AT THE SAME TIME.
If you miss pills you could get pregnant. This includes starting the pack late. The more pills you miss, the more likely you are to get pregnant. See "WHAT TO DO IF YOU MISS PILLS" below.
3. MANY WOMEN HAVE SPOTTING OR LIGHT BLEEDING, OR MAY FEEL SICK TO THEIR STOMACH DURING THE FIRST 1-3 PACKS OF PILLS.
If you feel sick to your stomach, do not stop taking FALMINA. The problem will usually go away. If it doesn't go away, check with your health-care provider.
4. MISSING PILLS CAN ALSO CAUSE SPOTTING OR LIGHT BLEEDING, even when you make up these missed pills.
On the days you take 2 pills to make up for missed pills, you could also feel a little sick to your stomach.
5. IF YOU HAVE VOMITING (within 4 hours after you take your pill), you should follow the instructions for WHAT TO DO IF YOU MISS PILLS. IF YOU HAVE DIARRHEA or IF YOU TAKE SOME MEDICINES, including some antibiotics, your pills may not work as well.
Use a back-up nonhormonal method (such as condoms or spermicide) until you check with your health-care provider.
6. IF YOU HAVE TROUBLE REMEMBERING TO TAKE THE PILL, talk to your health-care provider about how to make pill-taking easier or about using another method of birth control.
7. IF YOU HAVE ANY QUESTIONS OR ARE UNSURE ABOUT THE INFORMATION IN THIS LEAFLET, call your health-care provider.
BEFORE YOU START TAKING FALMINA
1. DECIDE WHAT TIME OF DAY YOU WANT TO TAKE YOUR PILL. It is important to take it at about the same time every day.
2. LOOK AT YOUR PILL PACK. 
The 28-pill pack has 21 "active" orange pills (with hormones) to take for 3 weeks, followed by 1 week of reminder white pills (without hormones).
3. FIND:
1) where on the pack to start taking pills,
2) in what order to take the pills (follow the arrows), and
3) the week numbers as shown in the picture below.

4. BE SURE YOU HAVE READY AT ALL TIMES:
ANOTHER KIND OF BIRTH CONTROL (such as condoms or spermicide) to use as a back-up in case you miss pills.
AN EXTRA, FULL PILL PACK.
For use of day labels, see WHEN TO START THE FIRST PACK OF PILLS below.
WHEN TO START THE FIRST PACK OF PILLS
You have a choice of which day to start taking your first pack of pills.
Decide with your health-care provider which is the best day for you. Pick a time of day which will be easy to remember.
DAY 1 START
1. Pick the day label sticker that starts with the first day of your period. Place this day label sticker over the area that has the days of the week (starting with Sunday) pre-printed on the tablet dispenser.
Note: if the first day of your period is a Sunday, you can skip step #1.
2. Take the first "active" orange pill of the first pack during the first 24 hours of your period .
3. You will not need to use a back-up nonhormonal method of birth control, since you are starting the pill at the beginning of your period.
SUNDAY START
1. Take the first "active" orange pill of the first pack on the Sunday after your period starts, even if you are still bleeding. If your period begins on Sunday, start the pack that same day.
2. Use a nonhormonal method of birth control (such as condoms or spermicide) as a back-up method if you have sex anytime from the Sunday you start your first pack until the next Sunday (7 days).
WHAT TO DO DURING THE MONTH
1. Take one pill at the same time every day until the pack is empty.
Do not skip pills even if you are spotting or bleeding between monthly periods or feel sick to your stomach (nausea).
Do not skip pills even if you do not have sex very often.
2. When you finish a pack.
Start the next pack on the day after your last "reminder" pill. Do not wait any days between packs.
IF YOU SWITCH FROM ANOTHER BRAND OR COMBINATION PILLS
If your previous brand had 21 pills: Wait 7 days to start taking FALMINA. You will probably have your period during that week. Be sure that no more than 7 days pass between the 21-day pack and taking the first orange FALMINA pill ("active" with hormone).
If your previous brand had 28 pills: Start taking the first orange FALMINA pill ("active" with hormone) on the day after your last reminder pill. Do not wait any days between packs.
WHAT TO DO IF YOU MISS PILLS
FALMINA may not be as effective if you miss orange "active" pills, and particularly if you miss the first few or the last few orange "active" pills in a pack.
If you MISS 1 orange "active" pill:
1. Take it as soon as you remember. Take the next pill at your regular time. This means you may take 2 pills in 1 day.
2. You COULD BECOME PREGNANT if you have sex in the 7 days after you restart your pills. You MUST use a nonhormonal birth-control method (such as condoms or spermicide) as a back-up for those 7 days.
If you MISS 2 orange "active" pills in a row in WEEK 1 OR WEEK 2 of your pack:
1. Take 2 pills on the day you remember and 2 pills the next day.
2. Then take 1 pill a day until you finish the pack.
3. You COULD BECOME PREGNANT if you have sex in the 7 days after you miss pills. You MUST use nonhormonal birth-control method (such as condoms or spermicide) as a back-up for those 7 days.
If you MISS 2 orange "active" pills in a row in THE 3rd WEEK:
1. If you are a Day 1 Starter:
THROW OUT the rest of the pill pack and start a new pack that same day.
If you are a Sunday Starter:
Keep taking 1 pill every day until Sunday.
On Sunday, THROW OUT the rest of the pack and start a new pack of pills that same day.
2. You may not have your period this month but this is expected
However, if you miss your period 2 months in a row, call your health-care provider because you might be pregnant.
3. You COULD BECOME PREGNANT if you have sex in the 7 days after you restart your pills. You MUST use a nonhormonal birth-control method (such as condoms or spermicide) as a back-up for those 7 days.
If you MISS 3 OR MORE orange "active" pills in a row (during the first 3 weeks):
1. If you are a Day 1 Starter:
THROW OUT the rest of the pill pack and start a new pack that same day.
If you are a Sunday Starter:
Keep taking 1 pill every day until Sunday.
On Sunday, THROW OUT the rest of the pack and start a new pack of pills that same day.
2. You may not have your period this month but this is expected.
However, if you miss your period 2 months in a row, call your health-care provider because you might be pregnant.
3. You COULD BECOME PREGNANT if you have sex in the 7 days after you restart your pills. You MUST use a nonhormonal birth-control method (such as condoms or spermicide) as a back-up for those 7 days.
If you forget any of the 7 white "reminder" pills in Week 4:
THROW AWAY the pills you missed.
Keep taking 1 pill each day until the pack is empty.
You do not need a back-up nonhormonal birth-control method if you start your next pack on time.
FINALLY, IF YOU ARE STILL NOT SURE WHAT TO DO ABOUT THE PILLS YOU HAVE MISSED
Use a BACK-UP NONHORMONAL BIRTH-CONTROL METHOD anytime you have sex.
KEEP TAKING ONE PILL EACH DAY until you can reach your health-care provider.
BIRTH CONTROL AFTER STOPPING THE PILL
If you do not wish to become pregnant after stopping the pill, speak to your health-care provider about another method of birth control.
DETAILED PATIENT LABELING
This product (like all oral contraceptives) is intended to prevent pregnancy. Oral contraceptives do not protect against transmission of HIV (AIDS) and other sexually transmitted diseases (STDs) such as chlamydia, genital herpes, genital warts, gonorrhea, hepatitis B, and syphilis.
INTRODUCTION
Any woman who considers using oral contraceptives (the "birth-control pill" or "the pill") should understand the benefits and risks of using this form of birth control. This leaflet will give you much of the information you will need to make this decision and will also help you determine if you are at risk of developing any of the serious side effects of the pill. It will tell you how to use the pill properly so that it will be as effective as possible. However, this leaflet is not a replacement for a careful discussion between you and your health-care provider. You should discuss the information provided in this leaflet with him or her, both when you first start taking the pill and during your revisits. You should also follow your health-care provider's advice with regard to regular check-ups while you are on the pill.
EFFECTIVENESS OF ORAL CONTRACEPTIVES
Oral contraceptives or "birth-control pills" or "the pill" are used to prevent pregnancy and are more effective than most other nonsurgical methods of birth control. When they are taken correctly, without missing any pills, the chance of becoming pregnant is approximately 1% per year (1 pregnancy per 100 women per year of use). Typical failure rates are approximately 5% per year (5 pregnancies per 100 women per year of use) when women who miss pills are included. The chance of becoming pregnant increases with each missed pill during each 28-day cycle of use.
In comparison, average failure rates for other methods of birth control during the first year of use are as follows:
IUD:0.1-2%
Depo-Provera¬ģ (injectable progestogen): 0.3%
Norplant¬ģ System (implants): 0.05%
Diaphragm with spermicides: 20%
Spermicides alone: 26%
Male condom alone: 14%
Female condom alone: 21%
Cervical cap
Nulliparous women: 20%
Parous women: 40%
Periodic abstinence: 25%
No methods: 85%
WHO SHOULD NOT TAKE ORAL CONTRACEPTIVES
Cigarette smoking increases the risk of serious adverse effects on the heart and blood vessels from oral-contraceptive use. This risk increases with age and with the amount of smoking (15 or more cigarettes per day has been associated with a significantly increased risk) and is quite marked in women over 35 years of age. Women who use oral contraceptives should not smoke.
 Some women should not use the pill. For example, you should not take the pill if you have any of the following conditions:
- History of heart attack or stroke.
- Blood clots in the legs (thrombophlebitis), lungs (pulmonary embolism), or eyes.
- A history of blood clots in the deep veins of your legs.
- Chest pain (angina pectoris).
- Known or suspected breast cancer or cancer of the lining of the uterus, cervix or vagina, or certain hormonally-sensitive cancers.
- Unexplained vaginal bleeding (until a diagnosis is reached by your health-care provider).
- Liver tumor (benign or cancerous) or active liver disease.
- Yellowing of the whites of the eyes or of the skin (jaundice) during pregnancy or during previous use of the pill.
- Known or suspected pregnancy.
- A need for surgery with prolonged bedrest.
- Heart valve or heart rhythm disorders that may be associated with formation of blood clots.
- Diabetes affecting your circulation.
- Headaches with neurological symptoms.
- Uncontrolled high blood pressure.
- Allergy or hypersensitivity to any of the components of FALMINA (levonorgestrel and ethinyl estradiol tablets).
Tell your health-care provider if you have had any of these conditions. Your health-care provider can recommend another method of birth control.
You should not take the pills if you take any Hepatitis C drug combination containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir. This may increase levels of the liver enzyme "alanine aminotransferase" (ALT) in the blood.
OTHER CONSIDERATIONS BEFORE TAKING ORAL CONTRACEPTIVES
Tell your health-care provider if you or any family member has ever had:
- Breast nodules, fibrocystic disease of the breast, an abnormal breast X-ray or mammogram.
- Diabetes.
- Elevated cholesterol or triglycerides.
- High blood pressure.
- A tendency to form blood clots.
- Migraine or other headaches or epilepsy.
- Depression.
- Gallbladder, liver, heart, or kidney disease.
- History of scanty or irregular menstrual periods.
Women with any of these conditions should be checked often by their health-care provider if they choose to use oral contraceptives. Also, be sure to inform your health-care provider if you smoke or are on any medications.
Although cardiovascular disease risks may be increased with oral contraceptive use in healthy, non-smoking women over 40 (even with the newer low-dose formulations), there are also greater potential health risks associated with pregnancy in older women.
RISKS OF TAKING ORAL CONTRACEPTIVES
1. Risks of developing blood clots
Blood clots and blockage of blood vessels are the most serious side effects of taking oral contraceptives and can cause death or serious disability. In particular, a clot in the legs can cause thrombophlebitis and a clot that travels to the lungs can cause a sudden blocking of the vessel carrying blood to the lungs. Rarely, clots occur in the blood vessels of the eye and may cause blindness, double vision, or impaired vision.
Users of combination oral contraceptives have a higher risk of developing blood clots compared to non-users. This risk is highest during the first year of combination oral-contraceptive use.
If you take oral contraceptives and need elective surgery, need to stay in bed for a prolonged illness or injury, or have recently delivered a baby, you may be at risk of developing blood clots. You should consult your health-care provider about stopping oral contraceptives three to four weeks before surgery and not taking oral contraceptives for two weeks after surgery or during bed rest. You should also not take oral contraceptives soon after delivery of a baby or after a mid-trimester pregnancy termination. It is advisable to wait for at least four weeks after delivery if you are not breast-feeding. If you are breast-feeding, you should wait until you have weaned your child before using the pill. (See also the section While breast-feeding in GENERAL PRECAUTIONS .)
The risk of blood clots is greater in users of combination oral contraceptives compared to nonusers. This risk may be higher in users of high-dose pills (those containing 50 mcg or more of estrogen) and may also be greater with longer use. In addition, some of these increased risks may continue for a number of years after stopping combination oral contraceptives. The risk of abnormal blood clotting increases with age in both users and nonusers of combination oral contraceptives, but the increased risk from the oral contraceptive appears to be present at all ages.
The excess risk of blood clots is highest during the first year a woman ever uses a combined oral contraceptive. This increased risk is lower than blood clots associated with pregnancy. The use of combination oral contraceptives also increases the risk of other clotting disorders, including heart attack and stroke. Blood clots in veins cause death in 1% to 2% of cases. The risk of clotting is further increased in women with other conditions. Examples include: smoking, high blood pressure, abnormal lipid levels, certain inherited or acquired clotting disorders, obesity, surgery or injury, recent delivery or second trimester abortion, prolonged inactivity or bedrest. If possible, combination oral contraceptives should be stopped before surgery and during prolonged inactivity or bedrest.
Cigarette smoking increases the risk of serious cardiovascular events. This risk increases with age and amount of smoking and is quite pronounced in women over 35. Women who use combination oral contraceptives should be strongly advised not to smoke. If you smoke you should talk to your health care professional before taking combination oral contraceptives.
2. Heart attacks and strokes
Oral contraceptives may increase the tendency to develop strokes or transient ischemic attacks (blockage or rupture of blood vessels in the brain) and angina pectoris and heart attacks (blockage of blood vessels in the heart). Any of these conditions can cause death or serious disability.
Smoking greatly increases the possibility of suffering heart attacks and strokes. Furthermore, smoking and the use of oral contraceptives greatly increase the chances of developing and dying of heart disease.
Women with migraine (especially migraine/headache with neurological symptoms) who take oral contraceptives also may be at higher risk of stroke and must not use combination oral contraceptives (see section WHO SHOULD NOT TAKE ORAL CONTRACEPTIVES ).
3. Gallbladder disease
Oral-contraceptive users probably have a greater risk than nonusers of having gallbladder disease, although this risk may be related to pills containing high doses of estrogens. Oral-contraceptives may worsen existing gallbladder disease or accelerate the development of gallbladder disease in women previously without symptoms.
4. Liver tumors
In rare cases, oral contraceptives can cause benign but dangerous liver tumors. These benign liver tumors can rupture and cause fatal internal bleeding. In addition, a possible but not definite association has been found with the pill and liver cancers in two studies in which a few women who developed these very rare cancers were found to have used oral contraceptives for long periods. However, liver cancers are extremely rare. The chance of developing liver cancer from using the pill is thus even rarer.
5. Risk of Cancer
It is not known if hormonal birth control pills causes breast cancer. Some studies, but not all, suggest that there could be a slight increase in the risk of breast cancer among current users with longer duration of use.
If you have breast cancer now, or have had it in the past, do not use hormonal birth control because some breast cancers are sensitive to hormones.
Some studies have found an increase in the incidence of cancer of the cervix in women who use oral contraceptives. However, this finding may be related to factors other than the use of oral contraceptives.
6. Lipid Metabolism and Pancreatitis
There have been reports of increases of blood cholesterol and triglycerides in users of combination oral contraceptives. Increases in triglycerides have led to inflammation of the pancreas (pancreatitis) in some cases.
ESTIMATED RISK OF DEATH FROM A BIRTH-CONTROL METHOD OR PREGNANCY
All methods of birth control and pregnancy are associated with a risk of developing certain diseases which may lead to disability or death. An estimate of the number of deaths associated with different methods of birth control and pregnancy has been calculated and is shown in the following table.

In the above table, the risk of death from any birth-control method is less than the risk of childbirth, except for oral-contraceptive users over the age of 35 who smoke and pill users over the age of 40 even if they do not smoke. It can be seen in the table that for women aged 15 to 39, the risk of death was highest with pregnancy (7 to 26 deaths per 100,000 women, depending on age). Among pill users who do not smoke, the risk of death was always lower than that associated with pregnancy for any age group, except for those women over the age of 40, when the risk increases to 32 deaths per 100,000 women, compared to 28 associated with pregnancy at that age. However, for pill users who smoke and are over the age of 35, the estimated number of deaths exceeds those for other methods of birth control. If a woman is over the age of 40 and smokes, her estimated risk of death is four times higher (117/100,000 women) than the estimated risk associated with pregnancy (28/100,000 women) in that age group.
The suggestion that women over 40 who do not smoke should not take oral contraceptives is based on information from older high-dose pills. An Advisory Committee of the FDA discussed this issue in 1989 and recommended that the benefits of oral-contraceptive use by healthy, nonsmoking women over 40 years of age may outweigh the possible risks. Older women, as all women, who take oral contraceptives, should take an oral contraceptive which contains the least amount of estrogen and progestogen that is compatible with the individual patient needs.
WARNING SIGNALS
If any of these adverse effects occur while you are taking oral contraceptives, call your healthcare provider immediately:
- Sharp chest pain, coughing of blood, or sudden shortness of breath (indicating a possible clot in the lung).
- Pain in the calf (indicating a possible clot in the leg).
- Crushing chest pain or heaviness in the chest (indicating a possible heart attack).
- Sudden severe headache or vomiting, dizziness or fainting, disturbances of vision or speech, weakness, or numbness in an arm or leg (indicating a possible stroke).
- Sudden partial or complete loss of vision (indicating a possible clot in the eye).
- Breast lumps (indicating possible breast cancer or fibrocystic disease of the breast; ask your health-care provider to show you how to examine your breasts).
- Severe pain or tenderness in the stomach area (indicating a possibly ruptured liver tumor).
- Difficulty in sleeping, weakness, lack of energy, fatigue, or change in mood (possibly indicating severe depression).
- Jaundice or a yellowing of the skin or eyeballs, accompanied frequently by fever, fatigue, loss of appetite, dark-colored urine, or light-colored bowel movements (indicating possible liver problems).
SIDE EFFECTS OF ORAL CONTRACEPTIVES
1. Unscheduled or breakthrough vaginal bleeding or spotting
Unscheduled vaginal bleeding or spotting may occur while you are taking the pills. Unscheduled bleeding may vary from slight staining between menstrual periods to breakthrough bleeding which is a flow much like a regular period. Unscheduled bleeding occurs most often during the first few months of oral-contraceptive use, but may also occur after you have been taking the pill for some time. Such bleeding may be temporary and usually does not indicate any serious problems. It is important to continue taking your pills on schedule. If the bleeding occurs in more than one cycle or lasts for more than a few days, talk to your health-care provider.
2. Contact lenses
If you wear contact lenses and notice a change in vision or an inability to wear your lenses, contact your health-care provider.
3. Fluid retention
Oral contraceptives may cause edema (fluid retention) with swelling of the fingers or ankles and may raise your blood pressure. If you experience fluid retention, contact your health-care provider.
4. Melasma
A spotty darkening of the skin is possible, particularly of the face.
5. Other side effects
Other side effects may include nausea, breast tenderness, change in appetite, headache, nervousness, depression, dizziness, loss of scalp hair, rash, vaginal infections, inflammation of the pancreas, and allergic reactions.
If any of these side effects bother you, call your health-care provider.
GENERAL PRECAUTIONS
1. Missed periods and use of oral contraceptives before or during early pregnancy
There may be times when you may not menstruate regularly after you have completed taking a cycle of pills. If you have taken your pills regularly and miss one menstrual period, continue taking your pills for the next cycle but be sure to inform your health-care provider before doing so. If you have not taken the pills daily as instructed and missed a menstrual period, or if you missed two consecutive menstrual periods, you may be pregnant. Check with your health-care provider immediately to determine whether you are pregnant. Stop taking oral contraceptives if you are pregnant.
There is no conclusive evidence that oral-contraceptive use is associated with an increase in birth defects, when taken inadvertently during early pregnancy. Previously, a few studies had reported that oral contraceptives might be associated with birth defects, but these studies have not been confirmed. Nevertheless, oral contraceptives should not be used during pregnancy. You should check with your health-care provider about risks to your unborn child of any medication taken during pregnancy.
2. While breast-feeding
If you are breast-feeding, consult your health-care provider before starting oral contraceptives. Some of the drug will be passed on to the child in the milk. A few adverse effects on the child have been reported, including yellowing of the skin (jaundice) and breast enlargement. In addition, oral contraceptives may decrease the amount and quality of your milk. If possible, do not use oral contraceptives while breast-feeding. You should use another method of contraception since breast-feeding provides only partial protection from becoming pregnant and this partial protection decreases significantly as you breast-feed for longer periods of time. You should consider starting oral contraceptives only after you have weaned your child completely.
3. Laboratory tests
If you are scheduled for any laboratory tests, tell your doctor you are taking birth-control pills. Certain blood tests may be affected by birth-control pills.
4. Drug interactions
Certain drugs may interact with birth-control pills to make them less effective in preventing pregnancy or cause an increase in breakthrough bleeding. Such drugs include rifampin, drugs used for epilepsy such as barbiturates (for example, phenobarbital) and phenytoin (Dilantin¬ģ is one brand of this drug), primidone (Mysoline¬ģ), topiramate (Topamax¬ģ), carbamazepine (Tegretol¬ģ is one brand of this drug), phenylbutazone (Butazolidin¬ģ is one brand), some drugs used for HIV or AIDS such as ritonavir (Norvir¬ģ), modafinil (Provigil¬ģ) and possibly certain antibiotics (such as ampicillin and other penicillins, and tetracyclines), and herbal products containing St. John's Wort (Hypericum perforatum). You may also need to use a nonhormonal method of contraception during any cycle in which you take drugs that can make oral contraceptives less effective.
You may be at higher risk of a specific type of liver dysfunction if you take troleandomycin and oral contraceptives at the same time.
You should inform your health-care provider about all medicines you are taking, including nonprescription products.
5. Sexually transmitted diseases
This product (like all oral contraceptives) is intended to prevent pregnancy. It does not protect against transmission of HIV (AIDS) and other sexually transmitted diseases such as chlamydia, genital herpes, genital warts, gonorrhea, hepatitis B, and syphilis.
HOW TO TAKE FALMINA
IMPORTANT POINTS TO REMEMBER
BEFORE YOU START TAKING FALMINA:
1. BE SURE TO READ THESE DIRECTIONS:
Before you start taking FALMINA.
And
Anytime you are not sure what to do.
2. THE RIGHT WAY TO TAKE THE PILL IS TO TAKE ONE PILL EVERY DAY AT THE SAME TIME.
If you miss pills you could get pregnant. This includes starting the pack late. The more pills you miss, the more likely you are to get pregnant. See "WHAT TO DO IF YOU MISS PILLS" below.
3. MANY WOMEN HAVE SPOTTING OR LIGHT BLEEDING, OR MAY FEEL SICK TO THEIR STOMACH DURING THE FIRST 1 TO 3 PACKS OF PILLS.
If you feel sick to your stomach, do not stop taking FALMINA. The problem will usually go away. If it doesn't go away, check with your health-care provider.
4. MISSING PILLS CAN ALSO CAUSE SPOTTING OR LIGHT BLEEDING, even when you make up these missed pills.
On the days you take 2 pills to make up for missed pills, you could also feel a little sick to your stomach.
5. IF YOU HAVE VOMITING (within 4 hours after you take your pill), you should follow the instructions for WHAT TO IF YOU MISS PILLS. IF YOU HAVE DIARRHEA or IF YOU TAKE SOME MEDICINES, including some antibiotics, your pills may not work as well.
Use a back-up nonhormonal method (such as condoms or spermicide) until you check with your health-care provider.
6. IF YOU HAVE TROUBLE REMEMBERING TO TAKE THE PILL, talk to your health-care provider about how to make pill-taking easier or about using another method of birth control.
7. IF YOU HAVE ANY QUESTIONS OR ARE UNSURE ABOUT THE INFORMATION IN THIS LEAFLET, contact your health-care provider.
BEFORE YOU START TAKING FALMINA
1. DECIDE WHAT TIME OF DAY YOU WANT TO TAKE YOUR PILL. It is important to take it at about the same time every day.
2. LOOK AT YOUR PILL PACK.
The 28-pill pack has 21 "active" orange pills (with hormones) to take for 3 weeks, followed by 1 week of reminder white pills (without hormones).
3. FIND:
1) where on the pack to start taking pills,
2) in what order to take the pills (follow the arrows), and
3) the week numbers as shown in the picture below.

4. BE SURE YOU HAVE READY AT ALL TIMES:
ANOTHER KIND OF BIRTH CONTROL (such as condoms or spermicide) to use as a back-up in case you miss pills.
AN EXTRA, FULL PILL PACK.
For use of day labels, see WHEN TO START THE FIRST PACK OF PILLS.
WHEN TO START THE PACK OF PILLS
You have a choice of which day to start taking your first pack of pills.
Decide with your health-care provider which is the best day for you. Pick a time of day which will be easy to remember.
DAY 1 START:
1. Pick the day label sticker that starts with the first day of your period. Place this day label sticker over the area that has the days of the week (starting with Sunday) pre-printed on the tablet dispenser.
Note: if the first day of your period is a Sunday, you can skip step #1.
2. Take the first "active" orange pill of the first pack during the first 24 hours of your period .
3. You will not need to use a back-up nonhormonal method of birth control, since you are starting the pill at the beginning of your period.
SUNDAY START:
1. Take the first "active" orange pill of the first pack on the Sunday after your period starts, even if you are still bleeding. If your period begins on Sunday, start the pack that same day.
2. Use a nonhormonal method of birth control (such as condoms or spermicide) as a back-up method if you have sex anytime from the Sunday you start your first pack until the next Sunday (7 days).
WHAT TO DO DURING THE MONTH
1. Take one pill at the same time every day until the pack is empty.
Do not skip pills even if you are spotting or bleeding between monthly periods or feel sick to your stomach (nausea).
Do not skip pills even if you do not have sex very often.
2. When you finish a pack:
Start the next pack on the day after your last "reminder" pill. Do not wait any days between packs.
IF YOU SWITCH FROM ANOTHER BRAND OR COMBINATION PILLS:
If your previous brand had 21 pills: Wait 7 days to start taking FALMINA. You will probably have your period during that week. Be sure that no more than 7 days pass between the 21-day pack and taking the first orange FALMINA pill ("active" with hormone).
If your previous brand had 28 pills: Start taking the first orange FALMINA pill ("active" with hormone) on the day after your last reminder pill. Do not wait any days between packs.
WHAT TO DO IF YOU MISS PILLS
FALMINA may not be as effective if you miss orange "active" pills, and particularly if you miss the first few or the last few orange "active" pills in a pack.
If you MISS 1 orange "active" pill:
1. Take it as soon as you remember. Take the next pill at your regular time. This means you may take 2 pills in 1 day.
2. You COULD BECOME PREGNANT if you have sex in the 7 days after you restart your pills. You MUST use a nonhormonal birth-control method (such as condoms or spermicide) as a back-up for those 7 days.
If you MISS 2 orange "active" pills in a row in WEEK 1 OR WEEK 2 of your pack:
1. Take 2 pills on the day you remember and 2 pills the next day.
2. Then take 1 pill a day until you finish the pack.
3. You COULD BECOME PREGNANT if you have sex in the 7 days after you restart your pills. You MUST use a nonhormonal birth-control method (such as condoms or spermicide) as a back-up for those 7 days.
If you MISS 2 orange "active" pills in a row in THE 3rd WEEK:
1. If you are a Day 1 Starter:
THROW OUT the rest of the pill pack and start a new pack that same day.
If you are a Sunday Starter:
Keep taking 1 pill every day until Sunday.
On Sunday, THROW OUT the rest of the pack and start a new pack of pills that same day.
2. You may not have your period this month but this is expected
However, if you miss your period 2 months in a row, call your health-care provider because you might be pregnant.
3. You COULD BECOME PREGNANT if you have sex in the 7 days after you restart your pills. You MUST use a nonhormonal birth-control method (such as condoms or spermicide) as a back-up for those 7 days.
If you MISS 3 OR MORE orange "active" pills in a row (during the first 3 weeks):
1. If you are a Day 1 Starter:
THROW OUT the rest of the pill pack and start a new pack that same day.
If you are a Sunday Starter:
Keep taking 1 pill every day until Sunday.
On Sunday, THROW OUT the rest of the pack and start a new pack of pills that same day.
2. You may not have your period this month but this is expected.
However, if you miss your period 2 months in a row, call your health-care provider because you might be pregnant.
3. You COULD BECOME PREGNANT if you have sex in the 7 days after you restart your pills. You MUST use a nonhormonal birth-control method (such as condoms or spermicide) as a back-up for those 7 days.
If you forget any of the 7 white "reminder" pills in Week 4:
THROW AWAY the pills you missed.
Keep taking 1 pill each day until the pack is empty.
You do not need a back-up nonhormonal birth-control method if you start your next pack on time.
FINALLY, IF YOU ARE STILL NOT SURE WHAT TO DO ABOUT THE PILLS YOU HAVE MISSED
Use a BACK-UP NONHORMONAL BIRTH-CONTROL METHOD anytime you have sex.
KEEP TAKING ONE PILL EACH DAY until you can reach your health-care provider.
PREGANCY DUE TO PILL FAILURE
The incidence of pill failure resulting in pregnancy is approximately 1 per year (1 pregnancy per 100 women per year of use) if taken every day as directed, but the more typical failure rate is approximately 5% per year (5 pregnancies per 100 women per year of use) including women who do not always take the pill exactly as directed without missing any pills. If you do become pregnant, the risk to the fetus is minimal, but you should stop taking your pills and discuss the pregnancy with your health-care provider
PREGNANCY AFTER STOPPING THE PILL
There may be some delay in becoming pregnant after you stop using oral contraceptives, especially if you had irregular menstrual cycles before you used oral contraceptives. It may be advisable to postpone conception until you begin menstruating regularly once you have stopped taking the pill and desire pregnancy.
There does not appear to be any increase in birth defects in newborn babies when pregnancy occurs soon after stopping the pill.
BIRTH CONTROL AFTER STOPPING THE PILL
If you do not wish to become pregnant after stopping the pill, you should use another method of birth control immediately after stopping FALMINA. Speak to your health-care provider about another method of birth control.
OVERDOSAGE
Overdosage may cause nausea, vomiting, breast tenderness, dizziness, abdominal pain and fatigue/drowsiness. Withdrawal bleeding may occur in females. In case of overdosage, contact your health-care provider or pharmacist.
OTHER INFORMATION
Your health-care provider will take a medical and family history before prescribing oral contraceptives and will examine you. The physical examination may be delayed to another time if you request it and your health-care provider believes that it is appropriate to postpone it. You should be reexamined at least once a year. Be sure to inform your health-care provider if there is a family history of any of the conditions uled previously in this leaflet. Be sure to keep all appointments with your health-care provider, because this is a time to determine if there are early signs of side effects of oral-contraceptive use.
Do not use the drug for any condition other than the one for which it was prescribed. This drug has been prescribed specifically for you; do not give it to others who may want birth-control pills.
HEALTH BENEFITS FROM ORAL CONTRACEPTIVES
In addition to preventing pregnancy, use of oral contraceptives may provide certain benefits. They are:
- Menstrual cycles may become more regular.
- Blood flow during menstruation may be lighter, and less iron may be lost. Therefore, anemia due to iron deficiency is less likely to occur.
- Pain or other symptoms during menstruation may be encountered less frequently.
- Ovarian cysts may occur less frequently.
- Ectopic (tubal) pregnancy may occur less frequently.
- Noncancerous cysts or lumps in the breast may occur less frequently.
- Acute pelvic inflammatory disease may occur less frequently.
- Oral-contraceptive use may provide some protection against developing two forms of cancer: cancer of the ovaries and cancer of the lining of the uterus.
If you want more information about birth-control pills, ask your health-care provider or pharmacist. They have a more technical leaflet called the Professional Labeling which you may wish to read.
To report SUSPECTED ADVERSE REACTIONS, contact Northstar Rx LLC at 1-800-206-7821 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch .

Manufactured for: Northstar Rx LLC
                                 Memphis TN 38141
Manufactured by: Novast Laboratories Ltd.
                                Nantong, China 226009
I 0017
Rev. B
Rev. 12/2023
Package Label.principal Display Panel
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site