Aripiprazole (aripiprazole 10 mg) Dailymed
Generic: aripiprazole is used for the treatment of Schizophrenia
IMPRINT: I 94
SHAPE: rectangle
COLOR: blue
All Imprints
aripiprazole 2 mg - i 94 rectangle blue
aripiprazole tablet - i 94 rectangle blue
Boxed Warning
Warning: Increased Mortality In Elderly Patients With Dementia-related Psychosis And Suicidal Thoughts And Behaviors With Antidepressant Drugs
Go PRO for all pill images
Warning: Increased Mortality In Elderly Patients With Dementia-related Psychosis And Suicidal Thoughts And Behaviors With Antidepressant Drugs
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Aripiprazole tablets are not approved for the treatment of patients with dementia-related psychosis [see Warnings and Precautions ( 5.1)].    Antidepressants increased the risk of suicidal thoughts and behavior in children, adolescents, and young adults in short-term studies. These studies did not show an increase in the risk of suicidal thoughts and behavior with antidepressant use in patients over age 24 years; there was a reduction in risk with antidepressant use in patients aged 65 years and older [see Warnings and Precautions ( 5.3)].    In patients of all ages who are started on antidepressant therapy, monitor closely for worsening, and for emergence of suicidal thoughts and behaviors. Advise families and caregivers of the need for close observation and communication with the prescriber [see Warnings and Precautions ( 5.3)].
¬† ¬† ¬† ¬† See full prescribing information for complete boxed warning.¬† ‚ÄĘ Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Aripiprazole tablets are not approved for the treatment of patients with dementia-related psychosis. (5.1 )¬† ‚ÄĘ Increased risk of suicidal thinking and behavior in children, adolescents, and young adults taking antidepressants. Monitor for worsening and emergence of suicidal thoughts and behaviors. (5.3 )
1 Indications And Usage
Aripiprazole oral tablets are indicated for the treatment of:
- Schizophrenia 
- Treatment of Tourette’s Disorder 
Aripiprazole tablets are an atypical antipsychotic. The oral formulations are indicated for:
- Schizophrenia (
14.1 ) - Treatment of Tourette’s disorder (
14.5 )
2 Dosage And Administration
¬† Initial¬†Dose Recommended¬†Dose Maximum¬†Dose Schizophrenia ‚Äď adults (2.1) 10 to 15 mg/day 10 to 15 mg/day 30 mg/day Schizophrenia ‚Äď adolescents (2.1) 2 mg/day 10 mg/day 30 mg/day Tourette‚Äôs disorder ‚Äď (2.5) Patients < 50kg 2 mg/day 5 mg/day 10 mg/day Patients > 50kg 2 mg/day 10 mg/day 20 mg/day
‚Äʬ†Oral formulations: Administer once daily without regard to meals (2 )¬† ‚Äʬ†Known CYP2D6 poor metabolizers: Half of the usual dose (2.7 ) ¬† ¬†
2.1 Schizophrenia
Adults  The recommended starting and target dose for aripiprazole tablets is 10 or 15 mg/day administered on a once-a-day schedule without regard to meals. Aripiprazole tablets have been systematically evaluated and shown to be effective in a dose range of 10 to 30 mg/day, when administered as the tablet formulation; however, doses higher than 10 or 15 mg/day were not more effective than 10 or 15 mg/day. Dosage increases should generally not be made before 2 weeks, the time needed to achieve steady-state [see Clinical Studies ( 14.1)] .   Maintenance Treatment: Maintenance of efficacy in schizophrenia was demonstrated in a trial involving patients with schizophrenia who had been symptomatically stable on other antipsychotic medications for periods of 3 months or longer. These patients were discontinued from those medications and randomized to either aripiprazole tablets 15 mg/day or placebo, and observed for relapse [see Clinical Studies ( 14.1)] . Patients should be periodically reassessed to determine the continued need for maintenance treatment. 
Adolescents The recommended target dose of aripiprazole tablets is 10 mg/day. Aripiprazole was studied in adolescent patients 13 to 17 years of age with schizophrenia at daily doses of 10 mg and   30 mg. The starting daily dose of the tablet formulation in these patients was 2 mg, which was titrated to 5 mg after 2 days and to the target dose of 10 mg after 2 additional days. Subsequent dose increases should be administered in 5 mg increments. The 30 mg/day dose was not shown to be more efficacious than the 10 mg/day dose. Aripiprazole tablets can be administered without regard to meals [see Clinical Studies ( 14.1)] . Patients should be periodically reassessed to determine the need for maintenance treatment.
Switching from Other Antipsychotics  There are no systematically collected data to specifically address switching patients with schizophrenia from other antipsychotics to aripiprazole tablets or concerning concomitant administration with other antipsychotics. While immediate discontinuation of the previous antipsychotic treatment may be acceptable for some patients with schizophrenia, more gradual discontinuation may be most appropriate for others. In all cases, the period of overlapping antipsychotic administration should be minimized. 
2.5 Tourettes Disorder
Pediatric Patients (6 to 18 years) The recommended dosage range for Tourette’s Disorder is 5 to 20 mg/day.  For patients weighing less than 50 kg, dosing should be initiated at 2 mg/day with a target dose of 5 mg/day after 2 days. The dose can be increased to 10 mg/day in patients who do not achieve optimal control of tics. Dosage adjustments should occur gradually at intervals of no less than one week.  For patients weighing 50 kg or more, dosing should be initiated at 2 mg/day for 2 days, and then increased to 5 mg/day for 5 days, with a target dose of 10 mg/day on Day 8. The dose can be increased up to 20 mg/day for patients who do not achieve optimal control of tics. Dosage adjustments should occur gradually in increments of 5 mg/day at intervals of no less than one week [see Clinical Studies (14.5)]. 
 
Patients should be periodically reassessed to determine the continued need for maintenance treatment.
2.7 Dosage Adjustments for Cytochrome P450 Considerations
Dosage adjustments are recommended in patients who are known CYP2D6 poor metabolizers and in patients taking concomitant CYP3A4 inhibitors or CYP2D6 inhibitors or strong CYP3A4 inducers (see Table 2). When the coadministered drug is withdrawn from the combination therapy, aripiprazole tablets dosage should then be adjusted to its original level. When the coadministered CYP3A4 inducer is withdrawn, aripiprazole tablets dosage should be reduced to the original level over 1 to 2 weeks. Patients who may be receiving a combination of strong, moderate, and weak inhibitors of CYP3A4 and CYP2D6 (e.g., a strong CYP3A4 inhibitor and a moderate CYP2D6 inhibitor or a moderate CYP3A4 inhibitor with a moderate CYP2D6 inhibitor), the dosing may be reduced to one-quarter (25%) of the usual dose initially and then adjusted to achieve a favorable clinical response. 
Table 2: Dose Adjustments for Aripiprazole Tablets in Patients who are known CYP2D6 Poor Metabolizers and Patients Taking Concomitant CYP2D6 Inhibitors, 3A4 Inhibitors, and/or CYP3A4 Inducers
Factors Dosage Adjustments for Aripiprazole Tablets Known CYP2D6 Poor Metabolizers Administer half of usual dose Known CYP2D6 Poor Metabolizers taking concomitant strong CYP3A4 inhibitors (e.g., itraconazole, clarithromycin) Administer a quarter of usual dose Strong CYP2D6 (e.g., quinidine, fluoxetine, paroxetine)  or  CYP3A4 inhibitors (e.g., itraconazole, clarithromycin) Administer half of usual dose StrongCYP2D6  and CYP3A4 inhibitors Administer a quarter of usual dose Strong CYP3A4 inducers (e.g., carbamazepine, rifampin) Double usual dose over 1 to 2 weeks   2.8 Dosing of Oral Solution
The oral solution can be substituted for tablets on a mg-per-mg basis up to the 25 mg dose level. Patients receiving 30 mg tablets should receive 25 mg of the solution [see Clinical Pharmacology ( 12.3)] . 
3 Dosage Forms And Strengths
 Aripiprazole tablets, USP are available as described in 3. 
Table 3: Aripiprazole Tablets Presentations
Tablet Strength Tablet Color/Shape Tablet Markings 2 mg Light green to green modified rectangle ‚ÄúI‚ÄĚ and ‚Äú94‚ÄĚ 5 mg Light blue to blue modified rectangle ‚ÄúI‚ÄĚ and ‚Äú95‚ÄĚ 10 mg Light pink to pink modified rectangle ‚ÄúI‚ÄĚ and ‚Äú96‚ÄĚ 15 mg Light yellow to yellow round ‚ÄúI‚ÄĚ and ‚Äú97‚ÄĚ 20 mg White to off white round ‚ÄúI‚ÄĚ and ‚Äú98‚ÄĚ 30 mg Light pink to pink round ‚ÄúI ‚ÄĚ and ‚Äú99‚ÄĚ
- Tablets: 2 mg, 5 mg, 10 mg, 15 mg, 20 mg, and 30 mg (3) 
4 Contraindications
Aripiprazole tablets are contraindicated in patients with a history of a hypersensitivity reaction to aripiprazole. Reactions have ranged from pruritus/urticaria to anaphylaxis [see Adverse Reactions ( 6.2)]. 
- Known hypersensititivity to aripiprazole tablets (4)
5 Warnings And Precautions
- Cerebrovascular Adverse Reactions in Elderly Patients with Dementia-Related Psychosis:Increased incidence of cerebrovascular adverse reactions (e.g., stroke, transient ischemic attack, including fatalities) (
5.2 )- Neuroleptic Malignant Syndrome:Manage with immediate discontinuation and close monitoring (
5.4 )- Tardive Dyskinesia:Discontinue if clinically appropriate (
5.5 )- Metabolic Changes:Atypical antipsychotic drugs have been associated with metabolic changes that include hyperglycemia/diabetes mellitus, dyslipidemia, and body weight gain (
5.6 )- Hyperglycemia/Diabetes Mellitus:Monitor glucose regularly in patients with and at risk for diabetes (
5.6 )- Dyslipidemia:Undesirable alterations in lipid levels have been    observed in patients treated with atypical antipsychotics (
5.6 )- Weight Gain:Weight gain has been observed with atypical antipsychotic use. Monitor weight (
5.6 )- Pathological Gambling and Other Compulsive Behaviors:Consider dose reduction or discontinuation (
5.7 )- Orthostatic Hypotension:Monitor heart rate and blood pressure and warn patients with known cardiovascular or cerebrovascular disease, and risk of dehydration or syncope (
5.8 )- Leukopenia, Neutropenia, and Agranulocytosis:have been reported with antipsychotics including aripiprazole tablets. Patients with a history of a clinically significant low white blood cell count (WBC) or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of aripiprazole tablets should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors (
5.10 )- Seizures/Convulsions: Use cautiously in patients with a history of seizures or with conditions that lower the seizure threshold (
5.11 )- Potential for Cognitive and Motor Impairment:Use caution when operating machinery (
5.12 )- Suicide:The possibility of a suicide attempt is inherent in schizophrenia. Closely supervise high-risk patients (
5.14 )  5.1 Increased Mortality in Elderly Patients with Dementia-Related Psychosis
Increased Mortality  Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Aripiprazole is not approved for the treatment of patients with dementia-related psychosis [ see Boxed Warning].    Safety Experience in Elderly Patients with Psychosis Associated with Alzheimer’s Disease
 
In three, 10 week, placebo-controlled studies of aripiprazole tablets in elderly patients with psychosis associated with Alzheimer‚Äôs disease (n=938; mean age: 82.4 years; range: 56 to 99 years), the adverse reactions that were reported at an incidence of ‚Č•3% and aripiprazole tablets incidence at least twice that for placebo were lethargy [placebo 2%, aripiprazole tablets 5%], somnolence (including sedation) [placebo 3%, aripiprazole tablets 8%], and incontinence (primarily, urinary incontinence) [placebo 1%, aripiprazole tablets 5%], excessive salivation [placebo 0%, aripiprazole tablets 4%], and lightheadedness [placebo 1%, aripiprazole tablets 4%].¬†
The safety and efficacy of aripiprazole in the treatment of patients with psychosis associated with dementia have not been established. If the prescriber elects to treat such patients with aripiprazole, assess for the emergence of difficulty swallowing or excessive somnolence, which could predispose to accidental injury or aspiration [see Boxed Warning].
5.2 Cerebrovascular Adverse Events, Including Stroke
In placebo-controlled clinical studies (two flexible dose and one fixed dose study) of dementia-related psychosis, there was an increased incidence of cerebrovascular adverse events (e.g., stroke, transient ischemic attack), including fatalities, in aripiprazole-treated patients (mean age: 84 years; range: 78 to 88 years). In the fixed-dose study, there was a statistically significant dose response relationship for cerebrovascular adverse events in patients treated with aripiprazole. Aripiprazole is not approved for the treatment of patients with dementia-related psychosis [see Boxed Warning].  
5.3 Suicidal Thoughts and Behaviors in Children, Adolescents and Young Adults
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term, placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18 to 24 years) with MDD and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24 years; there was a reduction with antidepressants compared to placebo in adults aged 65 years and older. The pooled analyses of placebo-controlled trials in children and adolescents with MDD, Obsessive Compulsive Disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs. placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1,000 patients treated) are provided in Table 5. Table 5: 
Age Range Drug-Placebo Difference in Number of Cases of Suicidality per 1000 Patients Treated ¬† Increases Compared to Placebo <18 14 additional cases 18 to 24 5 additional cases ¬† Decreases Compared to Placebo 25 to 64 1 fewer case ‚Č•65 6 fewer cases
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.  It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression. 
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases. 
 
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for MDD as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality. Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient’s presenting symptoms. Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to healthcare providers. Such monitoring should include daily observation by families and caregivers. Prescriptions for aripiprazole should be written for the smallest quantity of tablets consistent with good patient management, in order to reduce the risk of overdose.
 
It should be noted that aripiprazole is not approved for use in treating depression in the pediatric population.
5.4 Neuroleptic Malignant Syndrome (NMS)
A potentially fatal symptom complex sometimes referred to as Neuroleptic Malignant Syndrome (NMS) may occur with administration of antipsychotic drugs, including aripiprazole. Rare cases of NMS occurred during aripiprazole treatment in the worldwide clinical database. Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status, and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmia). Additional signs may include elevated creatine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure.
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to exclude cases where the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever, and primary central nervous system pathology.
The management of NMS should include: 1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy; 2) intensive symptomatic treatment and medical monitoring; and 3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS. If a patient requires antipsychotic drug treatment after recovery from NMS, the potential reintroduction of drug therapy should be carefully considered. The patient should be carefully monitored since recurrences of NMS have been reported. 
5.5 Tardive Dyskinesia
A syndrome of potentially irreversible, involuntary, dyskinetic movements may develop in patients treated with antipsychotic drugs. Although the prevalence of the syndrome appears to be highest among the elderly, especially elderly women, it is impossible to rely upon prevalence estimates to predict, at the inception of antipsychotic treatment, which patients are likely to develop the syndrome. Whether antipsychotic drug products differ in their potential to cause tardive dyskinesia is unknown.  The risk of developing tardive dyskinesia and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses.  Tardive dyskinesia may remit, partially or completely, if antipsychotic treatment is withdrawn. Antipsychotic treatment, itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome and, thereby, may possibly mask the underlying process. The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.  Given these considerations, aripiprazole should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that (1) is known to respond to antipsychotic drugs and (2) for whom alternative, equally effective, but potentially less harmful treatments are not available or appropriate. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.  If signs and symptoms of tarvdive dyskinesia appear in a patient on aripiprazole, drug discontinuation should be considered. However, some patients may require treatment with aripiprazole despite the presence of the syndrome. 
5.6 Metabolic Changes
Atypical antipsychotic drugs have been associated with metabolic changes that include hyperglycemia/diabetes mellitus, dyslipidemia, and body weight gain. While all drugs in the class have been shown to produce some metabolic changes, each drug has its own specific risk profile
Hyperglycemia/Diabetes Mellitus
 
Hyperglycemia, in some cases extreme and associated with ketoacidosis or hyperosmolar coma or death, has been reported in patients treated with atypical antipsychotics. There have been reports of hyperglycemia in patients treated with aripiprazole [see Adverse Reactions ( 6.1, 6.2)]. Assessment of the relationship between atypical antipsychotic use and glucose abnormalities is complicated by the possibility of an increased background risk of diabetes mellitus in patients with schizophrenia and the increasing incidence of diabetes mellitus in the general population. Given these confounders, the relationship between atypical antipsychotic use and hyperglycemia-related adverse events is not completely understood. However, epidemiological studies suggest an increased risk of hyperglycemia-related adverse reactions in patients treated with the atypical antipsychotics. Because aripiprazole was not marketed at the time these studies were performed, it is not known if aripiprazole is associated with this increased risk. Precise risk estimates for hyperglycemia-related adverse reactions in patients treated with atypical antipsychotics are not available.  Patients with an established diagnosis of diabetes mellitus who are started on atypical antipsychotics should be monitored regularly for worsening of glucose control. Patients with risk factors for diabetes mellitus (e.g., obesity, family history of diabetes) who are starting treatment with atypical antipsychotics should undergo fasting blood glucose testing at the beginning of treatment and periodically during treatment. Any patient treated with atypical antipsychotics should be monitored for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia during treatment with atypical antipsychotics should undergo fasting blood glucose testing. In some cases, hyperglycemia has resolved when the atypical antipsychotic was discontinued; however, some patients required continuation of anti-diabetic treatment despite discontinuation of the suspect drug.  Adults  In an analysis of 13 placebo-controlled monotherapy trials in adults, primarily with schizophrenia or another indication, the mean change in fasting glucose in aripiprazole-treated patients (+4.4 mg/dL; median exposure 25 days; N=1,057) was not significantly different than in placebo-treated patients (+2.5 mg/dL; median exposure 22 days; N=799). Table 6 shows the proportion of aripiprazole-treated patients with normal and borderline fasting glucose at baseline (median exposure 25 days) that had treatment-emergent high fasting glucose measurements compared to placebo-treated patients (median exposure 22 days).  Table 6:  Changes in Fasting Glucose from Placebo-Controlled Monotherapy Trials in Adult Patients
¬† Category Change (at least once) from Baseline Treatment Arm n/ N % Fasting Glucose Normal to High (<100 mg/dL to ‚Č•126 mg/dL) Aripiprazole Tablets 31/822 3.8 Placebo 22/605 3.6 Borderline¬†to High (‚Č•100 mg/dL and <126 mg/dL¬†to ‚Č•126 mg/dL) Aripiprazole Tablets 31/176 17. Placebo 13/142 9.2
At 24 weeks, the mean change in fasting glucose in aripiprazole-treated patients was not significantly different than in placebo-treated patients [+2.2 mg/dL (n=42) and +9.6 mg/dL (n=28), respectively].¬† Pediatric Patients and Adolescents In an analysis of two placebo-controlled trials in adolescents with schizophrenia (13 to 17 years) and pediatric patients with another indication (10 to 17 years), the mean change in fasting glucose in aripiprazole-treated patients (+4.8 mg/dL; with a median exposure of 43 days; N=259) was not significantly different than in placebo-treated patients (+1.7 mg/dL; with a median exposure of 42 days; N=123). In an analysis of two placebo-controlled trials in pediatric and adolescent patients with Tourette‚Äôs disorder (6 to 18 years) with median exposure of 57 days, the mean change in fasting glucose in aripiprazole treated patients (0.79 mg/dL; N=90) was not significantly different than in placebo-treated patients (‚Äď1.66 mg/dL; N=58). Table 8 shows the proportion of patients with changes in fasting glucose levels from the pooled adolescent schizophrenia and another indication (median exposure of 42 to 43 days).¬† Table 8: Changes in Fasting Glucose from Placebo-Controlled Trials in Pediatric and Adolescent Patients
Category Change (at least once) from Baseline I ndication T reatment A rm n /N % Fasting Glucose Normal to High (<100 mg/dL to ‚Č•126 mg/dL) Pooled Schizophrenia and another indication Aripiprazole Tablets 2/236 0.8 Placebo 2/110 1.8 ¬† Tourette‚Äôs Disorder Aripiprazole Tablets 3/88 3.4 Placebo 1/58 1.7 Fasting Glucose Borderline to High (‚Č•100 mg/dL and <126 mg/dL to ‚Č•126 mg/dL) Pooled Schizophrenia and another indication Aripiprazole Tablets 1/22 4.5 Placebo 0/12 0 Tourette‚Äôs Disorder Aripiprazole Tablets 0/11 0 ¬† ¬† Placebo 0/4 0
At 12 weeks in the pooled adolescent schizophrenia and another indication trials, the mean change in fasting glucose in aripiprazole-treated patients was not significantly different than in placebo-treated patients [+2.4 mg/dL (n=81) and  +0.1 mg/dL (n=15), respectively].  Dyslipidemia  Undesirable alterations in lipids have been observed in patients treated with atypical antipsychotics.  There were no significant differences between aripiprazole- and placebo-treated patients in the proportion with changes from normal to clinically significant levels for fasting/nonfasting total cholesterol, fasting triglycerides, fasting LDLs, and fasting/nonfasting HDLs. Analyses of patients with at least 12 or 24 weeks of exposure were limited by small numbers of patients.  Adults Table 9 shows the proportion of adult patients, primarily from pooled schizophrenia and another indication monotherapy placebo-controlled trials, with changes in total cholesterol (pooled from 17 trials; median exposure 21 to 25 days), fasting triglycerides (pooled from eight trials; median exposure 42 days), fasting LDL cholesterol (pooled from eight trials; median exposure 39 to 45 days, except for placebo-treated patients with baseline normal fasting LDL measurements, who had median treatment exposure of 24 days) and HDL cholesterol (pooled from nine trials; median exposure 40 to 42 days).  Table 9: Changes in Blood Lipid Parameters from Placebo-Controlled Monotherapy Trials in Adults
¬† Treatment Arm n/N % Total Cholesterol Normal to High (<200 mg/dL to ‚Č•240 mg/dL) Aripiprazole Tablets 34/1,357 2.5 Placebo 27/973 2.8 Fasting Triglycerides Normal to High (<150 mg/dL to ‚Č•200 mg/dL) Aripiprazole Tablets 40/539 7.4 Placebo 30/431 7 Fasting LDL Cholesterol Normal to High (<100 mg/dL to ‚Č•160 mg/dL) Aripiprazole Tablets 2/332 0.6 Placebo 2/268 0.7 HDL Cholesterol Normal to Low (‚Č•40 mg/dL to <40 mg/dL) Aripiprazole Tablets 121/1,066 11.4 Placebo 99/794 12.5
 
In monotherapy trials in adults, the proportion of patients at 12 weeks and 24 weeks with changes from Normal to High in total cholesterol (fasting/nonfasting), fasting triglycerides, and fasting LDL cholesterol were similar between aripiprazole- and placebo-treated patients: at 12 weeks, Total Cholesterol (fasting/nonfasting), 1/71 (1.4%) vs. 3/74 (4.1%); Fasting Triglycerides, 8/62 (12.9%) vs. 5/37 (13.5%); Fasting LDL Cholesterol, 0/34 (0%) vs. 1/25  (4 %), respectively; and at 24 weeks, Total Cholesterol (fasting/nonfasting), 1/42 (2.4%) vs. 3/37 (8.1%); Fasting Triglycerides, 5/34 (14.7%) vs. 5/20 (25%); Fasting LDL Cholesterol, 0/22 (0%) vs. 1/18 (5.6%), respectively. 
Pediatric Patients and Adolescents  Table 11 shows the proportion of adolescents with schizophrenia (13 to 17 years) and pediatric patients with other indication (10 to 17 years) with changes in total cholesterol and HDL cholesterol (pooled from two placebo-controlled trials; median exposure 42 to 43 days) and fasting triglycerides (pooled from two placebo-controlled trials; median exposure 42 to 44 days). 
Table 11:  Changes in Blood Lipid Parameters from Placebo-Controlled Monotherapy Trials in Pediatric and Adolescent Patients in Schizophrenia and Another Indication
Total Cholesterol Normal to High (<170 mg/dL to ‚Č•200 mg/dL) Treatment Arm n/N % Aripiprazole Tablets 3/220 1.4 Placebo 0/116 0 Fasting Triglycerides Normal to High (<150 mg/dL to ‚Č•200 mg/dL) Aripiprazole Tablets 7/187 3.7 Placebo 4/85 4.7 HDL Cholesterol Normal to Low (‚Č•40 mg/dL to <40 mg/dL) Aripiprazole Tablets 27/236 11.4 Placebo 22/109 20.2
In monotherapy trials of adolescents with schizophrenia and pediatric patients with another indication, the proportion of patients at 12 weeks and 24 weeks with changes from Normal to High in total cholesterol (fasting/nonfasting), fasting triglycerides, and fasting LDL cholesterol were similar between aripiprazole- and placebo-treated patients: at 12 weeks, Total Cholesterol (fasting/nonfasting), 0/57 (0%) vs. 0/15 (0%); Fasting Triglycerides, 2/72 (2.8%) vs. 1/14 (7.1%), respectively; and at 24 weeks, Total Cholesterol (fasting/nonfasting), 0/36 (0%) vs. 0/12 (0%); Fasting Triglycerides, 1/47 (2.1%) vs. 1/10 (10 %), respectively. Table 13 shows the proportion of patients with changes in total cholesterol (fasting/nonfasting) and fasting triglycerides (median exposure 57 days) and HDL cholesterol (median exposure 57 days) from two placebo-controlled trials in pediatric patients (6 to 18 years) with Tourette’s Disorder.
Table 13:  Changes in Blood Lipid Parameters from Placebo-Controlled Trials in Pediatric Patients with Tourette’s Disorder
Total Cholesterol Normal to High (<170 mg/dL to ‚Č•200 mg/dL) Treatment Arm n/N % Aripiprazole Tablets 1/85 1.2 Placebo 0/46 0 Fasting Triglycerides Normal to High (<150 mg/dL to ‚Č•200 mg/dL) Aripiprazole Tablets 5/94 5.3 Placebo 2/55 3.6 HDL Cholesterol Normal to Low (‚Č•40 mg/dL to <40 mg/dL) Aripiprazole Tablets 4/108 3.7 Placebo 2/67 3.0
Weight Gain¬† Weight gain has been observed with atypical antipsychotic use. Clinical monitoring of weight is recommended.¬† Adults¬† In an analysis of 13 placebo-controlled monotherapy trials, primarily from pooled schizophrenia and another indication, with a median exposure of 21 to 25 days, the mean change in body weight in aripiprazole-treated patients was +0.3 kg (N=1673) compared to¬† ¬† ¬†‚Äď0.1 kg (N=1100) in placebo- controlled patients. At 24 weeks, the mean change from baseline in body weight in aripiprazole-treated patients was ‚Äď1.5 kg (n=73) compared to ‚Äď0.2 kg (n=46) in placebo-treated patients.¬†
Table 14 shows the percentage of adult patients with weight gain ‚Č•7% of body weight by indication.
Table 14: Percentage of Patients from Placebo-Controlled Trials in Adult Patients with Weight Gain ‚Č•7% of Body Weight¬†
¬† Weight gain¬† ‚Č• 7% of body weight ¬†¬† Indication Treatment Arm¬† N¬† Patients n (%)¬† ¬† Schizophrenia* ¬†Aripiprazole Tablets¬† ¬† 852¬† 69 (8.1) ¬† ¬† Placebo¬† ¬†379 12 (3.2) ¬† ¬†other indication‚Ć ¬†Aripiprazole¬†Tablets ¬†719 ¬†16 (2.2) ¬† ¬† ¬†Placebo¬† ¬†598 ¬†16 (2.7) ¬†¬†*¬†4 to 6 weeks duration.¬†¬†‚Ƭ†3 weeks duration.¬†¬† ¬† ¬† ¬† ¬†
Pediatric Patients and Adolescents  In an analysis of two placebo-controlled trials in adolescents with schizophrenia (13 to 17 years) and pediatric patients with another indication (10 to 17 years) with median exposure of 42 to 43 days, the mean change in body weight in aripiprazole-treated patients was +1.6 kg (N=381) compared to +0.3 kg (N=187) in placebo-treated patients. At 24 weeks, the mean change from baseline in body weight in aripiprazole-treated patients was +5.8 kg (n=62) compared to +1.4 kg (n=13) in placebo-treated patients. 
In two short-term, placebo-controlled trials in patients (6 to 18 years) with Tourette’s Disorder with median exposure of 57 days, the mean change in body weight in aripiprazole-treated patients was +1.5 kg (n=105) compared to +0.4 kg (n=66) in placebo-treated patients.
Table 15 shows the percentage of pediatric and adolescent patients with weight gain ‚Č•7% of body weight by indication.¬†
Table 15: Percentage of Patients from Placebo-Controlled Monotherapy Trials in Pediatric and Adolescent Patients with Weight Gain ‚Č•7% of Body Weight
¬† Indication Treatment Arm N Patients n (%) ¬† Weight gain ‚Č•7% of body weight Pooled Schizophrenia¬†and another indication* Aripiprazole Tablets 381 20 (5.2) Placebo 187 3 (1.6) Tourette‚Äôs Disorder‚Ä° Aripiprazole Tablets 105 21 (20.0) Placebo 66 5 (7.6) *¬†4 to 6 weeks duration¬† ‚Ä°¬†8 to 10 weeks duration.¬†
In an open-label trial that enrolled patients from the two placebo-controlled trials of adolescents with schizophrenia (13 to 17 years) and pediatric patients with another indication (10 to 17 years), 73.2% of patients (238/325) completed 26 weeks of therapy with aripiprazole. After 26 weeks, 32.8% of patients gained ‚Č•7% of their body weight, not adjusted for normal growth. To adjust for normal growth, z-scores were derived (measured in standard deviations [SD]), which normalize for the natural growth of pediatric patients and adolescents by comparisons to age- and gender-matched population standards. A z-score change <0.5 SD is considered not clinically significant. After 26 weeks, the mean change in z-score was 0.09 SD.¬† When treating pediatric patients for any indication, weight gain should be monitored and assessed against that expected for normal growth.
5.7 Pathological Gambling and Other Compulsive Behaviours
Post-marketing case reports suggest that patients can experience intense urges, particularly for gambling, and the inability to control these urges while taking aripiprazole. Other compulsive urges, reported less frequently, include sexual urges, shopping, eating or binge eating, and other impulsive or compulsive behaviors. Because patients may not recognize these behaviors as abnormal, it is important for prescribers to ask patients or their caregivers specifically about the development of new or intense gambling urges, compulsive sexual urges, compulsive shopping, binge or compulsive eating, or other urges while being treated with aripiprazole. It should be noted that impulse-control symptoms can be associated with the underlying disorder. In some cases, although not all, urges were reported to have stopped when the dose was reduced, or the medication was discontinued. Compulsive behaviors may result in harm to the patient and others if not recognized. Consider dose reduction or stopping the medication if a patient develops such urges.
5.8 Orthostatic Hypotension
Aripiprazole may cause orthostatic hypotension, perhaps due to its őĪ 1-adrenergic receptor antagonism. The incidence of orthostatic hypotension-associated events from short-term, placebo-controlled trials of adult patients on oral aripiprazole (n=2,467) included (aripiprazole incidence, placebo incidence) orthostatic hypotension (1%, 0.3%), postural dizziness (0.5%, 0.3%), and syncope (0.5%, 0.4%); of pediatric patients 6 to 18 years of age (n=732) on oral aripiprazole included orthostatic hypotension (0.5%, 0%), postural dizziness (0.4%, 0%), and syncope (0.2%, 0%) [see Adverse Reactions ( 6.1)]. The incidence of a significant orthostatic change in blood pressure (defined as a decrease in systolic blood pressure ‚Č•20 mmHg accompanied by an increase in heart rate ‚Č•25 bpm when comparing standing to supine values) for aripiprazole was not meaningfully different from placebo (aripiprazole incidence, placebo incidence): in adult oral aripiprazole-treated patients (4%, 2%), in pediatric oral aripiprazole-treated patients aged 6 to 18 years (0.4%, 1%).¬† Aripiprazole should be used with caution in patients with known cardiovascular disease (history of myocardial infarction or ischemic heart disease, heart failure, or conduction abnormalities), cerebrovascular disease, or conditions which would predispose patients to hypotension (dehydration, hypovolemia, and treatment with antihypertensive medications) [see Drug Interactions ( 7.1)] .
5.9 Falls
Antipsychotics, including aripiprazole, may cause somnolence, postural hypotension, motor and sensory instability, which may lead to falls and, consequently, fractures or other injuries. For patients with diseases, conditions, or medications that could exacerbate these effects, complete fall risk assessments when initiating antipsychotic treatment and recurrently for patients on long-term antipsychotic therapy.
5.10 Leukopenia, Neutropenia, and Agranulocytosis
In clinical trials and/or postmarketing experience, events of leukopenia and neutropenia have been reported temporally related to antipsychotic agents, including aripiprazole. Agranulocytosis has also been reported.  Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC)/absolute neutrophil count (ANC) and history of drug-induced leukopenia/neutropenia. In patients with a history of a clinically significant low WBC/ANC or drug-induced leukopenia/neutropenia, perform a complete blood count (CBC) frequently during the first few months of therapy. In such patients, consider discontinuation of aripiprazole at the first sign of a clinically significant decline in WBC in the absence of other causative factors.  Monitor patients with clinically significant neutropenia for fever or other symptoms or signs of infection and treat promptly if such symptoms or signs occur. Discontinue aripiprazole in patients with severe neutropenia (absolute neutrophil count <1,000/mm 3) and follow their WBC counts until recovery.
5.11 Seizures/Convulsions
In short-term, placebo-controlled trials, patients with a history of seizures excluded seizures/convulsions occurred in 0.1% (3/2,467) of undiagnosed adult patients treated with oral aripiprazole, in 0.1% (1/732) of pediatric patients (6 to 18 years). As with other antipsychotic drugs, aripiprazole should be used cautiously in patients with a history of seizures or with conditions that lower the seizure threshold. Conditions that lower the seizure threshold may be more prevalent in a population of 65 years or older.
5.12 Potential for Cognitive and Motor Impairment
Aripiprazole, like other antipsychotics, may have the potential to impair judgment, thinking, or motor skills. For example, in short-term, placebo-controlled trials, somnolence (including sedation) was reported as follows (aripiprazole incidence, placebo incidence): in adult patients ((n=2,467) treated with oral aripiprazole (11%, 6%), in pediatric patients ages 6 to 17 years (n=611 ; 24%, 6%). Somnolence (including sedation) led to discontinuation in 0.3% (8/2,467) of adult patients and 3% (20/732) of pediatric patients (6 to 18 years) on oral aripiprazole in short-term, placebo-controlled trials. Despite the relatively modest increased incidence of these events compared to placebo, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that therapy with aripiprazole does not affect them adversely.     
5.13 Body Temperature Regulation
Disruption of the body’s ability to reduce core body temperature has been attributed to antipsychotic agents. Appropriate care is advised when prescribing aripiprazole for patients who will be experiencing conditions which may contribute to an elevation in core body temperature, (e.g., exercising strenuously, exposure to extreme heat, receiving concomitant medication with anticholinergic activity, or being subject to dehydration) [see Adverse Reactions ( 6.2)].
5.14 Suicide
The possibility of a suicide attempt is inherent in psychotic illnesses and close supervision of high-risk patients should accompany drug therapy. Prescriptions for aripiprazole should be written for the smallest quantity consistent with good patient management in order to reduce the risk of overdose [see Adverse Reactions ( 6.1, 6.2)] .  
5.15 Dysphagia
Esophageal dysmotility and aspiration have been associated with antipsychotic drug use, including aripiprazole. Aspiration pneumonia is a common cause of morbidity and mortality in elderly patients, in particular those with advanced Alzheimer’s dementia. Aripiprazole and other antipsychotic drugs should be used cautiously in patients at risk for aspiration pneumonia [see Warnings and Precautions (5.1) and Adverse Reactions ( 6.2)] .
6 Adverse Reactions
¬† Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The following adverse reactions are discussed in more detail in other sections of the labeling:¬†¬† ‚Äʬ†Increased Mortality in Elderly Patients with Dementia-Related Psychosis [see Boxed¬† ¬†Warning and Warnings and Precautions ( 5.1)] ¬† ‚Äʬ†Cerebrovascular Adverse Events, Including Stroke [see Warnings and Precautions ( 5.2)]¬† ‚Äʬ†Suicidal Thoughts and Behaviors in Children, Adolescents, and Young Adults [see Boxed Warning and Warnings Precautions ( 5.3)] ¬† ‚Äʬ†Neuroleptic Malignant Syndrome (NMS) [see Warnings and Precautions ( 5.4)]¬† ‚Äʬ†Tardive Dyskinesia [see Warnings and Precautions ( 5.5)] ¬† ‚Äʬ†Metabolic Changes [see Warnings and Precautions ( 5.6)]¬† ‚Äʬ†Pathological Gambling and Other Compulsive Behaviors [see Warnings and Precautions ( 5.7)] ‚Äʬ†Orthostatic Hypotension [see Warnings and Precautions ( 5.8)]¬† ‚Äʬ†Falls [see Warnings and Precautions ( 5.9)] ‚Äʬ†Leukopenia, Neutropenia, and Agranulocytosis [see Warnings and Precautions ( 5.10)]¬† ‚Äʬ†Seizures/Convulsions [see Warnings and Precautions ( 5.11)]¬† ‚Äʬ†Potential for Cognitive and Motor Impairment [see Warnings and Precautions ( 5.12)] ‚Äʬ†Body Temperature Regulation [see Warnings and Precautions ( 5.13)]¬† ‚Äʬ†Suicide [see Warnings and Precautions ( 5.14)]¬† ‚Äʬ†Dysphagia [see Warnings and Precautions ( 5.15)]¬† The most common adverse reactions in adult patients in clinical trials (‚Č•10%) were nausea, vomiting, constipation, headache, dizziness, akathisia, anxiety, insomnia, and restlessness. The most common adverse reactions in the pediatric clinical trials (‚Č•10%) were somnolence, headache, vomiting, extrapyramidal disorder, fatigue, increased appetite, insomnia, nausea, nasopharyngitis, and weight increased.¬† Aripiprazole has been evaluated for safety in 13,543 adult patients who participated in multiple-dose, clinical trials in schizophrenia, other indications,¬† Dementia of the Alzheimer‚Äôs type, Parkinson‚Äôs disease, and alcoholism, and who had approximately 7,619 patient-years of exposure to oral aripiprazole. A total of 3,390 patients were treated with oral aripiprazole for at least 180 days and 1,933 patients treated with oral aripiprazole had at least one year of exposure.¬† Aripiprazole has been evaluated for safety in 1,686 patients (6 to 18 years) who participated in multiple-dose, clinical trials in schizophrenia, other indications or Tourette‚Äôs disorder and who had approximately 1,342 patient-years of exposure to oral aripiprazole. A total of 959 pediatric patients were treated with oral aripiprazole for at least 180 days and 556 pediatric patients treated with oral aripiprazole had at least one year of exposure.¬† The conditions and duration of treatment with aripiprazole included (in overlapping categories) double-blind, comparative and noncomparative open-label studies, inpatient and outpatient studies, fixed- and flexible-dose studies, and short- and longer-term exposure.
Commonly observed adverse reactions (incidence ‚Č•5% and at least twice that for placebo) were (6.1 ):¬†
- Adult patients with schizophrenia: akathisia 
- Pediatric patients (13 to 17 years) with schizophrenia: extrapyramidal   disorder, somnolence, and tremor 
- Pediatric patients (6 to 18 years) with Tourette’s disorder: sedation, somnolence, nausea, headache, nasopharyngitis, fatigue, increased appetite
To report SUSPECTED ADVERSE REACTIONS, contact Hetero Labs Limited at 1-866-495-1995 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
 
6.1 Clinical Trials Experience
Adult Patients with Schizophrenia The following findings are based on a pool of five placebo-controlled trials (four 4 week and one 6 week) in which oral aripiprazole was administered in doses ranging from 2 to 30 mg/day.¬† Commonly Observed Adverse Reactions¬† The only commonly observed adverse reaction associated with the use of aripiprazole in patients with schizophrenia (incidence of 5% or greater and aripiprazole incidence at least twice that for placebo) was akathisia (aripiprazole tablets 8%; placebo 4%).¬† Less Common Adverse Reactions in Adults¬† Table 17 enumerates the pooled incidence, rounded to the nearest percent, of adverse reactions that occurred during acute therapy (up to 6 weeks in schizophrenia and up to 3 weeks in another indication), including only those reactions that occurred in 2% or more of patients treated with aripiprazole (doses ‚Č•2 mg/day) and for which the incidence in patients treated with aripiprazole was greater than the incidence in patients treated with placebo in the combined dataset. Table 17: Adverse Reactions in Short-Term, Placebo-Controlled Trials in Adult Patients Treated with Oral Aripiprazole Tablets
  Percentage of Patients Reporting Reaction * System Organ Class Aripiprazole Tablets Placebo Preferred Term ( n=1,843) (n=1,166) Eye Disorders Blurred Vision 3 1 Gastrointestinal Disorders Nausea 15 11 Constipation 11 7 Vomiting 11 6 Dyspepsia 9 7 Dry Mouth 5 4 Toothache Abdominal Discomfort 4 3 3 2 Stomach Discomfort 3 2 General Disorders and Administration Site Conditions Fatigue 6 4 Pain 3 2 Musculoskeletal and Connective Tissue Disorders Musculoskeletal Stiffness 4 3 Pain in Extremity 4 2 Myalgia 2 1 Muscle Spasms 2 1 Nervous System Disorders Headache 27 23 Dizziness 10 7 Akathisia 10 4 Sedation 7 4 Extrapyramidal Disorder 5 3 Tremor 5 3 Somnolence 5 3 Psychiatric Disorders Agitation 19 17 Insomnia 18 13 Anxiety 17 13 Restlessness 5 3 Respiratory, Thoracic, and Mediastinal Disorders Pharyngolaryngeal Pain 3 2 Cough 3 2 *Adverse reactions reported by at least 2% of patients treated with oral aripiprazole, except adverse reactions which had an incidence equal to or less than placebo.
An examination of population subgroups did not reveal any clear evidence of differential adverse reaction incidence on the basis of age, gender, or race. Pediatric Patients (13 to 17 years) with Schizophrenia   The following findings are based on one 6-week, placebo-controlled trial in which oral aripiprazole was administered in doses ranging from 2 to 30 mg/day.  Adverse Reactions Associated with Discontinuation of Treatment   The incidence of discontinuation due to adverse reactions between aripiprazole-treated and placebo-treated pediatric patients (13 to 17 years) was 5% and 2%, respectively. Commonly Observed Adverse Reactions Commonly observed adverse reactions associated with the use of aripiprazole in adolescent patients with schizophrenia (incidence of 5% or greater and aripiprazole incidence at least twice that for placebo) were extrapyramidal disorder, somnolence, and tremor. Pediatric Patients (6 to 18 years) with Tourette's Disorder  The following findings are based on one 8 week and one 10 week, placebo-controlled trials in which oral aripiprazole was administered in doses of 2 to 20 mg/day.  Adverse Reactions Associated with Discontinuation of Treatment  The incidence of discontinuation due to adverse reactions between aripiprazole-treated and placebo-treated pediatric patients (6 to 18 years) was 7% and 1%, respectively.  Commonly Observed Adverse Reactions  Commonly observed adverse reactions associated with the use of aripiprazole in pediatric patients with Tourette's disorder (incidence of 5% or greater and aripiprazole incidence at least twice that for placebo) are shown in Table 21. 
Table 21: Commonly Observed Adverse Reactions in Short-Term, Placebo-Controlled Trials of Pediatric Patients (6 to 18 years) with Tourette's Disorder Treated with Oral Aripiprazole
    Preferred Term Percentage of Patients Reporting Reaction * Aripiprazole Tablets (n=121) Placebo (n=72) Sedation 13 6 Somnolence 13 1 Nausea 11 4 Headache 10 3 Nasopharyngitis 9 0 Fatigue 8 0 Increased Appetite 7 1
Less Common Adverse Reactions in Pediatric Patients (6 to 18 years) with Schizophrenia, or Other Indications Table 22 enumerates the pooled incidence, rounded to the nearest percent, of adverse reactions that occurred during acute therapy (up to 6 weeks in schizophrenia, up to 4 weeks in one indication, up to 8 weeks in another indication, and up to 10 weeks in Tourette‚Äôs discorder), including only those reactions that occurred in 2% or more of pediatric patients treated with aripiprazole (doses ‚Č•2 mg/day) and for which the incidence in patients treated with aripiprazole was greater than the incidence in patients treated with placebo.
Table 22: Adverse Reactions in Short-Term, Placebo-Controlled Trials of Pediatric Patients (6 to 18 years) Treated with Oral Aripiprazole Tablets
  Percentage of Patients Reporting Reaction * System Organ Class Aripiprazole Tablets Placebo Preferred Term (n=732) (n=370) Eye Disorders Blurred Vision 3 0 Gastrointestinal Disorders                                            Abdominal Discomfort                                                  2                                               1 Vomiting 8 7 Nausea 8 4 Diarrhea 4 3 Salivary Hypersecretion 4 1 Abdominal Pain Upper 3 2 Constipation 2 2 General Disorders and Administration Site Conditions Fatigue 10 2 Pyrexia 4 1 Irritability 2 1 Asthenia 2 1 Infections and Infestations Nasopharyngitis 6 3 Investigations Weight Increased 3 1 Metabolism and Nutrition Disorders Increased Appetite 7 3 Decreased Appetite 5 4 Musculoskeletal and Connective Tissue Disorders Musculoskeletal Stiffness 2 1 Muscle Rigidity 2 1 Nervous System Disorders Somnolence 16 4 Headache 12 10 Sedation 9 2 Tremor 9 1 Extrapyramidal Disorder 6 1 Akathisia 6 4 Drooling 3 0 Lethargy 3 0 Dizziness 3 2 Dystonia 2 1 Respiratory, Thoracic, and Mediastinal Disorders Epistaxis 2 1 Skin and Subcutaneous Tissue Disorders Rash 2 1 *Adverse reactions reported by at least 2% of pediatric patients treated with oral aripiprazole, except adverse reactions which had an incidence equal to or less than placebo.
Dose-Related Adverse Reactions¬† Schizophrenia¬† Dose response relationships for the incidence of treatment-emergent adverse events were evaluated from four trials in adult patients with schizophrenia comparing various fixed doses (2, 5, 10, 15, 20, and 30 mg/day) of oral aripiprazole to placebo. This analysis, stratified by study, indicated that the only adverse reaction to have a possible dose response relationship, and then most prominent only with 30 mg, was somnolence [including sedation]; (incidences were placebo, 7.1%; 10 mg, 8.5%; 15 mg, 8.7%; 20 mg, 7.5%; 30 mg, 12.6%).¬† In the study of pediatric patients (13 to 17 years of age) with schizophrenia, three common adverse reactions appeared to have a possible dose response relationship: extrapyramidal disorder (incidences were placebo, 5%; 10 mg, 13%; 30 mg, 21.6%); somnolence (incidences were placebo, 6%; 10 mg, 11%; 30 mg, 21.6%); and tremor (incidences were placebo, 2%;¬† 10 mg, 2%; 30 mg, 11.8%).¬† Tourette‚Äôs Disorder In a study of pediatric patients (7 to 17 years of age) with Tourette‚Äôs disorder, no common adverse reaction(s) had a dose response relationship. Extrapyramidal Symptoms¬† Schizophrenia¬† In short-term, placebo-controlled trials in schizophrenia in adults, the incidence of reported EPS-related events, excluding events related to akathisia, for aripiprazole-treated patients was 13% vs. 12% for placebo; and the incidence of akathisia-related events for aripiprazole-treated patients was 8% vs. 4% for placebo. In the short-term, placebo-controlled trial of schizophrenia in pediatric patients (13 to 17 years), the incidence of reported EPS-related events, excluding events related to akathisia, for aripiprazole-treated patients was 25% vs. 7% for placebo; and the incidence of akathisia-related events for aripiprazole-treated patients was 9% vs. 6% for placebo. Objectively collected data from those trials was collected on the Simpson Angus Rating Scale (for EPS), the Barnes Akathisia Scale (for akathisia), and the Assessments of Involuntary Movement Scales (for dyskinesias). In the adult schizophrenia trials, the objectively collected data did not show a difference between aripiprazole tablets and placebo, with the exception of the Barnes Akathisia Scale (aripiprazole, 0.08; placebo, ‚Äď0.05). In the pediatric (13 to 17 years) schizophrenia trial, the objectively collected data did not show a difference between aripiprazole tablets and placebo, with the exception of the Simpson Angus Rating Scale (aripiprazole tablets, 0.24; placebo, ‚Äď0.29).¬† Similarly, in a long-term (26 week), placebo-controlled trial of schizophrenia in adults, objectively collected data on the Simpson Angus Rating Scale (for EPS), the Barnes Akathisia Scale (for akathisia), and the Assessments of Involuntary Movement Scales (for dyskinesias) did not show a difference between aripiprazole tablets and placebo.¬† Tourette‚Äôs Disorder¬† In the short-term, placebo-controlled trials in Tourette‚Äôs disorder in pediatric patients (6 to 18 years), the incidence of reported EPS-related events, excluding events related to akathisia, for aripiprazole-treated patients was 7% vs. 6% for placebo and the incidence of akathisia-related events for aripiprazole-treated patients was 4% vs. 6% for placebo.¬† In the pediatric (6 to 18 years) short-term Tourette‚Äôs disorder trials, changes in the Simpson Angus Rating Scale, Barnes Akathisia Scale and Assessments of Involuntary Movement Scale were not clinically meaningfully different for aripiprazole and placebo. Dystonia¬† Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first few days of treatment. Dystonic symptoms include¬† spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. While these symptoms can occur at low doses, they occur more frequently and with greater severity with high potency and at higher doses of first generation antipsychotic drugs. An elevated risk of acute dystonia is observed in males and younger age groups.¬† Additional Findings Observed in Clinical Trials¬† Adverse Reactions in Long-Term, Double-Blind, Placebo-Controlled Trials¬† The adverse reactions reported in a 26 week, double-blind trial comparing oral aripiprazole tablets and placebo in patients with schizophrenia were generally consistent with those reported in the short-term, placebo-controlled trials, except for a higher incidence of tremor [8% (12/153) for aripiprazole tablets¬† vs. 2% (3/153) for placebo]. In this study, the majority of the cases of tremor were of mild intensity (8/12 mild and 4/12 moderate), occurred early in therapy (9/12 ‚ȧ49 days), and were of limited duration (7/12 ‚ȧ10 days). Tremor infrequently led to discontinuation (<1%) of aripiprazole. In addition, in a long-term (52 week), active-controlled study, the incidence of tremor was 5% (40/859) for aripiprazole.¬† Other Adverse Reactions Observed During Clinical Trial Evaluation of Aripiprazole¬† The following uling does not include reactions: 1) already uled in previous tables or elsewhere in labeling, 2) for which a drug cause was remote, 3) which were so general as to be uninformative, 4) which were not considered to have significant clinical implications, or 5) which occurred at a rate equal to or less than placebo.¬† Reactions are categorized by body system according to the following definitions: frequentadverse reactions are those occurring in at least 1/100 patients; infrequentadverse reactions are those occurring in 1/100 to 1/1,000 patients; rarereactions are those occurring in fewer than 1/1,000 patients: Adults - Oral Administration¬† ‚Äʬ† Blood and Lymphatic System Disorders:¬† rare- thrombocytopenia¬† ‚Äʬ† Cardiac Disorders:¬† infrequent‚Äď bradycardia, palpitations, rare‚Äď atrial flutter, cardio-respiratory arrest, atrioventricular block, atrial fibrillation, angina pectoris, myocardial ischemia, myocardial infarction, cardiopulmonary failure¬† ‚Äʬ† Eye Disorders:¬† infrequent‚Äď photophobia; rare- diplopia¬† ¬†¬†¬†¬† ‚Äʬ† Gastrointestinal Disorders: infrequent- gastroesophageal reflux disease ‚Äʬ† General Disorders and Administration Site Conditions:¬†frequent- asthenia; infrequent‚Äď peripheral edema, chest pain; rare ‚Äď face edema¬† ‚Äʬ† Hepatobiliary Disorders:rare- hepatitis, jaundice¬† ‚Äʬ† Immune System Disorders:¬† rare- hypersensitivity¬† ‚Äʬ† Injury, Poisoning, and Procedural Complications: Infrequent‚Äď fall; rare‚Äď heat stroke¬† ‚Äʬ† Investigations: frequent- blood prolactin decreased, weight decreased, infrequent- hepatic enzyme increased, blood glucose increased, blood lactate dehydrogenase increased, gamma glutamyl transferase increased; rare‚Äď
blood
prolactin increased, blood urea increased, blood creatinine increased, blood bilirubin increased, electrocardiogram QT prolonged, glycosylated hemoglobin increased ‚Äʬ† Metabolism and Nutrition Disorders: frequent‚Äď anorexia; rare -¬†hypokalemia, hyponatremia, hypoglycemia ‚Äʬ† Musculoskeletal and Connective Tissue Disorders: infrequent- muscular weakness, muscle tightness; rare‚Äď rhabdomyolysis, mobility decreased¬† ‚Äʬ† Nervous System Disorders: infrequent- parkinsonism, memory impairment, cogwheel rigidity, hypokinesia, bradykinesia; rare‚Äď akinesia, myoclonus, coordination abnormal, speech disorder, Grand Mal convulsion; < 1/10,000 patients -choreoathetosis¬† ‚Äʬ† Psychiatric Disorders: infrequent‚Äď aggression, loss of libido, delirium; rare‚Äď libido increased, anorgasmia, tic, homicidal ideation, catatonia, sleep walking ‚Äʬ† Renal and Urinary Disorders: rare- urinary retention, nocturia¬† ‚Äʬ† Reproductive System and Breast Disorders:infrequent- erectile dysfunction; rare‚Äď gynaecomastia, menstruation irregular, amenorrhea, breast pain, priapism¬† ‚Äʬ† Respiratory, Thoracic, and Mediastinal Disorders: infrequent -nasal congestion, dyspnea¬† ‚Äʬ† Skin and Subcutaneous Tissue Disorders:infrequent- rash, hyperhidrosis, pruritus, photosensitivity reaction, alopecia; rare-urticaria¬† ‚Äʬ† Vascular Disorders: infrequent‚Äď hypotension, hypertension Pediatric Patients - Oral Administration¬† Most adverse events observed in the pooled database of 1,686 pediatric patients, aged 6 to 18 years, were also observed in the adult population. Additional adverse reactions observed in the pediatric population are uled below.¬† ‚Äʬ† Eye Disorders : infrequent- oculogyric crisis ‚Äʬ† Gastrointestinal Disorders: infrequent- tongue dry, tongue spasm¬† ‚Äʬ† Investigations: frequent- blood insulin increased¬† ‚Äʬ† Nervous System Disorders: infrequent- sleep talking¬† ‚Äʬ† Renal and Urinary Disorders frequent ‚Äďenuresis ‚Äʬ† Skin and Subcutaneous Tissue Disorders: infrequent- hirsutism¬†
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of aripiprazole. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure: occurrences of allergic reaction (anaphylactic reaction, angioedema, laryngospasm, pruritus/urticaria, or oropharyngeal spasm),  blood glucose fluctuation, Drug reaction with Eosinophilia and Systemic Symptoms (DRESS) hiccups, oculogyric crisis, and  pathological gambling.
7 Drug Interactions
Dosage adjustment due to drug interactions (7.1 ) :
Factors Dosage Adjustments for Aripiprazole Tablets Known CYP2D6 Poor Metabolizers Administer half of usual dose Known CYP2D6 Poor Metabolizers and strong CYP3A4 inhibitors Administer a quarter of usual dose Strong CYP2D6 or CYP3A4 inhibitors Administer half of usual dose Strong CYP2D6 and CYP3A4 inhibitors Administer a quarter of usual dose Strong CYP3A4 inducers Double usual dose over 1 to 2 weeks 7.1 Drugs Having Clinically Important Interactions with Aripiprazole Tablets
Table 25: Clinically Important Drug Interactions with Aripiprazole:
Concomitant   Drug Name or   Drug Class Clinical Rationale Clinical Recommendation Strong CYP3A4 Inhibitors (e.g., itraconazole, clarithromycin) or strong CYP2D6 inhibitors (e.g., quinidine, fluoxetine, paroxetine)   The concomitant use of aripiprazole with strong CYP 3A4 or CYP2D6 inhibitors increased the exposure of aripiprazole compared to the use of aripiprazole alone  [see ClinicalPharmacology ( 12.3)].   With concomitant use of aripiprazole with a strong CYP3A4 inhibitor or CYP2D6 inhibitor, reduce the aripiprazole dosage [see Dosageand Administration( 2.7)]. Strong CYP3A4 Inducers (e.g., carbamazepine, rifampin) The concomitant use of aripiprazole and carbamazepine decreased the exposure of aripiprazole compared to the use of aripiprazole alone [see  Clinical Pharmacology ( 12.3)]. With concomitant use of aripiprazole with a strong CYP3A4 inducer, consider increasing the aripiprazole dosage [see Dosage and Administration( 2.7)].   Antihypertensive Drugs Due to its alpha adrenergic antagonism, aripiprazole has the potential to enhance the effect of certain antihypertensive agents. Monitor blood pressure and adjust dose accordingly [seeWarnings and Precautions( 5.8)].       Benzodiazepines (e.g., lorazepam) The intensity of sedation was greater with the combination of oral aripiprazole and lorazepam as compared to that observed with aripiprazole alone. The orthostatic hypotension observed was greater with the combination as compared to that observed with lorazepam alone [seeWarningsandPrecautions ( 5.8)].       Monitor sedation and blood pressure. Adjust dose accordingly. 7.2 Drugs Having No Clinically Important Interactions with Aripiprazole Tablets
Based on pharmacokinetic studies, no dosage adjustment of aripiprazole is required when administered concomitantly with famotidine, valproate, lithium, lorazepam.  In addition, no dosage adjustment is necessary for substrates of CYP2D6 (e.g., dextromethorphan, fluoxetine, paroxetine, or venlafaxine), CYP2C9 (e.g., warfarin), CYP2C19 (e.g., omeprazole, warfarin, escitalopram), or CYP3A4 (e.g., dextromethorphan) when co-administered with aripiprazole. Additionally, no dosage adjustment is necessary for valproate, lithium, lamotrigine, lorazepam, or sertraline when co-administered with aripiprazole [see Clinical Pharmacology (12.3)].
8 Use In Specific Populations
Pregnancy: May cause extrapyramidal and/or withdrawal symptoms in neonates with third trimester exposure (8.1 ) 
8.1 Pregnancy
Pregnancy Exposure Registry   There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to atypical antipsychotics, including aripiprazole, during pregnancy. Healthcare providers are encouraged to register patients by contacting the National Pregnancy Registry for Atypical Antipsychotics at 1-866-961-2388 or visit http://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/. Risk Summary  Neonates exposed to antipsychotic drugs, including aripiprazole, during the third trimester of pregnancy are at risk for extrapyramidal and/or withdrawal symptoms following delivery (see Clinical Considerations). Overall available data from published epidemiologic studies of pregnant women exposed to aripiprazole have not established a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data). There are risks to the mother associated with untreated schizophrenia, and with exposure to antipsychotics, including aripiprazole, during pregnancy (see Clinical Considerations). In animal reproduction studies, oral and intravenous aripiprazole administration during organogenesis in rats and/or rabbits at doses 10 and 19 times, respectively, the maximum recommended human dose (MRHD) of 30 mg/day based on mg/m 2body surface area, produced fetal death, decreased fetal weight, undescended testicles, delayed skeletal ossification, skeletal abnormalities, and diaphragmatic hernia. Oral and intravenous aripiprazole administration during the pre- and post-natal period in rats at doses 10 times the MRHD based on mg/m 2body surface area, produced prolonged gestation, stillbirths, decreased pup weight, and decreased pup survival (see Data). The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively. Clinical Considerations  Disease-associated maternal and/or embryo/fetal risk There is a risk to the mother from untreated schizophrenia including increased risk of relapse, hospitalization, and suicide. Schizophrenia is associated with increased adverse perinatal outcomes, including preterm birth. It is not known if this is a direct result of the illness or other comorbid factors. A prospective, longitudinal study followed 201 pregnant women with a history of major depressive disorder who were euthymic and taking antidepressants at the beginning of pregnancy. The women who discontinued antidepressants during pregnancy were more likely to experience a relapse of major depression than women who continued antidepressants. Consider the risk of untreated depression when discontinuing or changing treatment with antidepressant medication during pregnancy and postpartum. Fetal/Neonatal Adverse Reactions  Extrapyramidal and/or withdrawal symptoms, including agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress, and feeding disorder have been reported in neonates who were exposed to antipsychotic drugs (including aripiprazole) during the third trimester of pregnancy. These symptoms have varied in severity. Monitor neonates for extrapyramidal and/or withdrawal symptoms and manage symptoms appropriately. Some neonates recovered within hours or days without specific treatment; others required prolonged hospitalization. Data Human data Published data from observational studies, birth registries, and case reports on the use of atypical antipsychotics during pregnancy do not report a clear association with antipsychotics and major birth defects. A retrospective study from a Medicaid database of 9258 women exposed to antipsychotics during pregnancy did not indicate an overall increased risk for major birth defects. Animal Data  In animal studies, aripiprazole demonstrated developmental toxicity, including possible teratogenic effects in rats and rabbits.
In pregnant rats treated orally with aripiprazole during organogenesis at doses of 3, 10, and  30 mg/kg/day, which are approximately 1, 3 and 10 times the MRHD of 30 mg/day based on mg/m 2body surface area, a slight prolongation of gestation and delay in fetal development, as evidenced by decreased fetal weight and undescended testes, were observed at 10 times the MRHD. Delayed skeletal ossification was observed at 3 and 10 times the MRHD. Delivered offspring had increased incidences of hepatodiaphragmatic nodules and diaphragmatic hernia were observed at 10 times the MRHD (the other dose groups were not examined for these findings). Postnatally, delayed vaginal opening was seen at 3 and 10 times the MRHD. Impaired reproductive performance (decreased fertility rate, corpora lutea, implants, live fetuses, and increased post-implantation loss, likely mediated through effects on female offspring) were observed at 10 times the MRHD; however, there was no evidence to suggest that these developmental effects were secondary to maternal toxicity. 
In pregnant rabbits treated orally with aripiprazole during organogenesis at doses of 10, 30, and 100 mg/kg/day which are 6, 19, and 65 times the MRHD of 30 mg/day based on mg/m 2body surface area, decreased maternal food consumption, and increased abortions as well as increased fetal mortality were observed at 65 times the MRHD. Decreased fetal weight and increased incidence of fused sternebrae were observed at 19 and 65 times the MRHD.
In rats treated orally with aripiprazole peri- and postnatally from gestation Day 17 through postpartum Day 21 at doses of 3, 10, and 30 mg/kg/day which are 1, 3, and 10 times the MRHD of 30 mg/day based on mg/m 2body surface area slight maternal toxicity and slightly prolonged gestation were observed at 10 times the MRHD. An increase in stillbirths and, decreases in pup weight (persisting into adulthood) and survival were also seen at this dose.
8.2 Lactation
Risk Summary Limited data from published literature report the presence of aripiprazole in human breast milk, at relative infant doses ranging between 0.7% to 8.3% of the maternal weight-adjusted dosage. There are reports of poor weight gain in breastfed infants exposed to aripiprazole and reports of inadequate milk supply in lactating women taking aripiprazole.  The development and health benefits of breastfeeding should be considered along with the mother’s clinical need for aripiprazole and any potential adverse effects on the breastfed infant from aripiprazole or from the underlying maternal condition.
8.4 Pediatric Use
The pharmacokinetics of aripiprazole and dehydro-aripiprazole in pediatric patients, 10 to 17 years of age, were similar to those in adults after correcting for the differences in body weight [see Clinical Pharmacology (12.3)].
Schizophrenia
 
Safety and effectiveness in pediatric patients with schizophrenia were established in a 6 week, placebo-controlled clinical trial in 202 pediatric patients aged 13 to 17 years [see Dosage and Administration (2.1), Adverse Reactions (6.1), and Clinical Studies (14.1)].Although maintenance efficacy in pediatric patients has not been systematically evaluated, maintenance efficacy can be extrapolated from adult data along with comparisons of aripiprazole pharmacokinetic parameters in adult and pediatric patients.  Tourette’s Disorder  Safety and effectiveness of aripiprazole in pediatric patients with Tourette’s Disorder were established in one 8 week (aged 7 to 17 years) and one 10 week trial (aged 6 to 18 years) in 194 pediatric patients [see Dosage and Administration (2.5), Adverse Reactions (6.1), and Clinical Studies (14.5)].Maintenance efficacy in pediatric patients has not been systematically evaluated. Juvenile Animal Studies  Aripiprazole in juvenile rats caused mortality, CNS clinical signs, impaired memory and learning, and delayed sexual maturation when administered at oral doses of 10, 20, 40 mg/kg/day from weaning (21 days old) through maturity (80 days old). At 40 mg/kg/day, mortality, decreased activity, splayed hind limbs, hunched posture, ataxia, tremors and other CNS signs were observed in both genders. In addition, delayed sexual maturation was observed in males. At all doses and in a dose-dependent manner, impaired memory and learning, increased motor activity, and histopathology changes in the pituitary (atrophy), adrenals (adrenocortical hypertrophy), mammary glands (hyperplasia and increased secretion), and female reproductive organs (vaginal mucification, endometrial atrophy, decrease in ovarian corpora lutea) were observed. The changes in female reproductive organs were considered secondary to the increase in prolactin serum levels. A No Observed Adverse Effect Level (NOAEL) could not be determined and, at the lowest tested dose of 10 mg/kg/day, there is no safety margin relative to the systemic exposures (AUC 0 to 24) for aripiprazole or its major active metabolite in adolescents at the maximum recommended pediatric dose of 15 mg/day. All drug-related effects were reversible after a 2 month recovery period, and most of the drug effects in juvenile rats were also observed in adult rats from previously conducted studies. Aripiprazole in juvenile dogs (2 months old) caused CNS clinical signs of tremors, hypoactivity, ataxia, recumbency and limited use of hind limbs when administered orally for 6 months at 3, 10, 30 mg/kg/day. Mean body weight and weight gain were decreased up to 18% in females in all drug groups relative to control values. A NOAEL could not be determined and, at the lowest tested dose of 3 mg/kg/day, there is no safety margin relative to the systemic exposures (AUC 0 to 24) for aripiprazole or its major active metabolite in adolescents at the maximum recommended pediatric dose of 15 mg/day. All drug-related effects were reversible after a 2 month recovery period.
8.5 Geriatric Use
No dosage adjustment is recommended for elderly patients [see Boxed Warning, Warnings and Precautions (5.1), and Clinical Pharmacology ( 12.3)] . Of the 13,543 patients treated with oral aripiprazole in clinical trials, 1,073 (8%) were ‚Č•65 years old and 799 (6%) were ‚Č•75 years old. Placebo-controlled studies of oral aripiprazole in schizophrenia or other indications did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger patients.¬† Aripiprazole is not approved for the treatment of patients with psychosis associated with Alzheimer‚Äôs disease [see Boxed Warning and Warnings and Precautions ( 5.1)].
8.6 CYP2D6 Poor Metabolizers
Dosage adjustment is recommended in known CYP2D6 poor metabolizers due to high aripiprazole concentrations. Approximately 8% of Caucasians and 3 to 8% of Black/African Americans cannot metabolize CYP2D6 substrates and are classified as poor metabolizers (PM) [see Dosage and Administration (2.7) and Clinical Pharmacology ( 12.3)]. 
8.7 Hepatic and Renal Impairment
No dosage adjustment for aripiprazole is required on the basis of a patient’s hepatic function (mild to severe hepatic impairment, Child-Pugh score between 5 and 15), or renal function (mild to severe renal impairment, glomerular filtration rate between 15 and 90 mL/minute) [see Clinical Pharmacology ( 12.3)] .  
8.8 Other Specific Populations
No dosage adjustment for aripiprazole is required on the basis of a patient’s sex, race, or smoking status [see Clinical Pharmacology ( 12.3)] .
9 Drug Abuse And Dependence
9.1 Controlled Substance
Aripiprazole is not a controlled substance. 
9.2 Abuse
Aripiprazole has not been systematically studied in humans for its potential for abuse, tolerance, or physical dependence. Consequently, patients should be evaluated carefully for a history of drug abuse, and such patients should be observed closely for signs of aripiprazole misuse or abuse (e.g., development of tolerance, increases in dose, drug-seeking behavior). 
9.3 Dependence
In physical dependence studies in monkeys, withdrawal symptoms were observed upon abrupt cessation of dosing. While the clinical trials did not reveal any tendency for any drug-seeking behavior, these observations were not systematic and it is not possible to predict on the basis of this limited experience the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed.
10 Overdosage
MedDRA terminology has been used to classify the adverse reactions. 
10.1 Human Experience
In clinical trials and in postmarketing experience, adverse reactions of deliberate or accidental overdosage with oral aripiprazole have been reported worldwide. These include overdoses with oral aripiprazole alone and in combination with other substances. No fatality was reported with aripiprazole alone. The largest known dose with a known outcome involved acute ingestion of 1,260 mg of oral aripiprazole (42 times the maximum recommended daily dose) by a patient who fully recovered. Deliberate or accidental overdosage was also reported in children (age 12 years and younger) involving oral aripiprazole tablet ingestions up to 195 mg with no fatalities.  Common adverse reactions (reported in at least 5% of all overdose cases) reported with oral aripiprazole overdosage (alone or in combination with other substances) include vomiting, somnolence, and tremor. Other clinically important signs and symptoms observed in one or more patients with aripiprazole overdoses (alone or with other substances) include acidosis, aggression, aspartate aminotransferase increased, atrial fibrillation, bradycardia, coma, confusional state, convulsion, blood creatine phosphokinase increased, depressed level of consciousness, hypertension, hypokalemia, hypotension, lethargy, loss of consciousness, QRS complex prolonged, QT prolonged, pneumonia aspiration, respiratory arrest, status epilepticus, and tachycardia. 
10.2 Management of Overdosage
No specific information is available on the treatment of overdose with aripiprazole. An electrocardiogram should be obtained in case of overdosage and if QT interval prolongation is present, cardiac monitoring should be instituted. Otherwise, management of overdose should concentrate on supportive therapy, maintaining an adequate airway, oxygenation and ventilation, and management of symptoms. Close medical supervision and monitoring should continue until the patient recovers.  Charcoal:In the event of an overdose of aripiprazole, an early charcoal administration may be useful in partially preventing the absorption of aripiprazole. Administration of 50 g of activated charcoal, one hour after a single 15 mg oral dose of aripiprazole, decreased the mean AUC and C maxof aripiprazole by 50%.  Hemodialysis:Although there is no information on the effect of hemodialysis in treating an overdose with aripiprazole, hemodialysis is unlikely to be useful in overdose management since aripiprazole is highly bound to plasma proteins. 
11 Description
Aripiprazole is a psychotropic drug that is available as aripiprazole tablets. Aripiprazole tablets, USP are chemically designated as 7-[4-[4-(2,3-Dichlorophenyl)-1-piperazinyl]butoxy]-3,4-dihydro-2(1H)-quinolinone. The molecular formula is C 23H 27C l2N 3O 2, and molecular weight is 448.39. The chemical structure is as follows:
Aripiprazole tablets, USP are available in 2 mg, 5 mg, 10 mg, 15 mg, 20 mg, and 30 mg strengths. Inactive ingredients include corn starch, FD&C Blue #2/Indigo Carmine Al, ferric oxide red, ferric oxide yellow, hydroxypropyl cellulose, lactose monohydrate, magnesium stearate and microcrystalline cellulose. FDA approved dissolution test specifications differ from USP
12 Clinical Pharmacology
12.1 Mechanism of Action
The mechanism of action of aripiprazole in schizophrenia is unclear. However, the efficacy of aripiprazole in the uled indications could be mediated through a combination of partial agonist activity at D 2and 5-HT 1Areceptors and antagonist activity at 5-HT 2Areceptors. 
12.2 Pharmacodynamics
Aripiprazole exhibits high affinity for dopamine D 2and D 3, serotonin 5-HT 1Aand 5-HT 2Areceptors (K ivalues of 0.34 nM, 0.8 nM, 1.7 nM, and 3.4 nM, respectively), moderate affinity for dopamine D 4, serotonin 5-HT 2Cand 5-HT 7 ,alpha 1-adrenergic and histamine H 1receptors (K ivalues of 44 nM, 15 nM, 39 nM, 57 nM, and 61 nM, respectively), and moderate affinity for the serotonin reuptake site (K i=98 nM). Aripiprazole has no appreciable affinity for cholinergic muscarinic receptors (IC 50>1000 nM).  
12.3 Pharmacokinetics
Aripiprazole activity is presumably primarily due to the parent drug, aripiprazole, and to a lesser extent, to its major metabolite, dehydro-aripiprazole, which has been shown to have affinities for D 2receptors similar to the parent drug and represents 40% of the parent drug exposure in plasma. The mean elimination half-lives are about 75 hours and 94 hours for aripiprazole and dehydro-aripiprazole, respectively. Steady-state concentrations are attained within 14 days of dosing for both active moieties. Aripiprazole accumulation is predictable from single-dose pharmacokinetics. At steady-state, the pharmacokinetics of aripiprazole is dose-proportional. Elimination of aripiprazole is mainly through hepatic metabolism involving two P450 isozymes, CYP2D6 and CYP3A4. For CYP2D6 poor metabolizers, the mean elimination half-life for aripiprazole is about 146 hours. Oral administration  Absorption  Tablet: Aripiprazole is well absorbed after administration of the tablet, with peak plasma concentrations occurring within 3 hours to 5 hours; the absolute oral bioavailability of the tablet formulation is 87%. Aripiprazole can be administered with or without food. Administration of a 15 mg aripiprazole tablet with a standard high-fat meal did not significantly affect the C maxor AUC of aripiprazole or its active metabolite, dehydro-aripiprazole, but delayed T maxby 3 hours for aripiprazole and 12 hours for dehydro-aripiprazole.  Distribution  The steady-state volume of distribution of aripiprazole following intravenous administration is high (404 L or 4.9 L/kg), indicating extensive extravascular distribution. At therapeutic concentrations, aripiprazole and its major metabolite are greater than 99% bound to serum proteins, primarily to albumin. In healthy human volunteers administered 0.5 to 30 mg/day aripiprazole for 14 days, there was dose-dependent D2 receptor occupancy indicating brain penetration of aripiprazole in humans.  Elimination  Metabolism  Aripiprazole is metabolized primarily by three biotransformation pathways: dehydrogenation, hydroxylation, and N-dealkylation. Based on in vitrostudies, CYP3A4 and CYP2D6 enzymes are responsible for dehydrogenation and hydroxylation of aripiprazole, and N-dealkylation is catalyzed by CYP3A4. Aripiprazole is the predominant drug moiety in the systemic circulation. At steady-state, dehydro-aripiprazole, the active metabolite, represents about 40% of aripiprazole AUC in plasma.  Excretion Following a single oral dose of [ 14C]-labeled aripiprazole, approximately 25% and 55% of the administered radioactivity was recovered in the urine and feces, respectively. Less than 1% of unchanged aripiprazole was excreted in the urine and approximately 18% of the oral dose was recovered unchanged in the feces.  Drug Interaction Studies  Effect of other drugs on the exposures of aripiprazole and dehydro-aripiprazole are summarized in Figure 1 and Figure 2, respectively. Based on simulation, a 4.5fold increase in mean C maxand AUC values at steady-state is expected when extensive metabolizers of CYP2D6 are administered with both strong CYP2D6 and CYP3A4 inhibitors. A 3fold increase in mean C maxand AUC values at steady-state is expected in poor metabolizers of CYP2D6 administered with strong CYP3A4 inhibitors.
Figure 1: The Effect of Other Drugs on Aripiprazole Pharmacokinetics
 
 
Figure 2: The Effect of Other Drugs on Dehydro-Aripiprazole Pharmacokinetics
 
The effect of aripiprazole on the exposures of other drugs are summarized in Figure 3.  Figure 3: The Effect of Aripiprazole on Pharmacokinetics of Other Drugs
Specific Populations  Exposure of aripiprazole and dehydro-aripiprazole in specific populations are summarized in Figure 4 and Figure 5, respectively. In addition, in pediatric patients (10 to 17 years of age) administered with aripiprazole (20 mg to 30 mg), the body weight corrected aripiprazole clearance was similar to the adults. Figure 4: Effect of Intrinsic Factors on Aripiprazole Pharmacokinetics
Figure 5: Effect of Intrinsic Factors on Dehydro-Aripiprazole Pharmacokinetics
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis  Lifetime carcinogenicity studies were conducted in ICR mice, F344 rats, and Sprague-Dawley (SD) rats. Aripiprazole was administered for 2 years in the diet at doses of 1, 3, 10, and  30 mg/kg/day to ICR mice and 1, 3, and 10 mg/kg/day to F344 rats (0.2, 0.5, 2 and 5 times and 0.3, 1 and 3 times the MRHD of 30 mg/day based on mg/m 2body surface area, respectively). In addition, SD rats were dosed orally for 2 years at 10, 20, 40, and 60 mg/kg/day, which are 3, 6, 13 and 19 times the MRHD based on mg/m 2body surface area. Aripiprazole did not induce tumors in male mice or male rats. In female mice, the incidences of pituitary gland adenomas and mammary gland adenocarcinomas and adenoacanthomas were increased at dietary doses of 3 to 30 mg/kg/day (0.5 to 5 times the MRHD). In female rats, the incidence of mammary gland fibroadenomas was increased at a dietary dose of 10 mg/kg/day (3 times the MRHD); and the incidences of adrenocortical carcinomas and combined adrenocortical adenomas/carcinomas were increased at an oral dose of  60 mg/kg/day (19 times the MRHD).  An increase in mammary, pituitary, and endocrine pancreas neoplasms has been found in rodents after chronic administration of other antipsychotic drugs and is considered to be mediated by prolonged dopamine D 2-receptor antagonism and hyperprolactinemia. Serum prolactin was not measured in the aripiprazole carcinogenicity studies. However, increases in serum prolactin levels were observed in female mice in a 13 week dietary study at the doses associated with mammary gland and pituitary tumors. Serum prolactin was not increased in female rats in 4week and 13 week dietary studies at the dose associated with mammary gland tumors. The relevance for human risk of the findings of prolactin-mediated endocrine tumors in rodents is unclear. Mutagenesis  The mutagenic potential of aripiprazole was tested in the in vitrobacterial reverse-mutation assay, the in vitrobacterial DNA repair assay, the in vitroforward gene mutation assay in mouse lymphoma cells, the in vitrochromosomal aberration assay in Chinese hamster lung (CHL) cells, the in vivomicronucleus assay in mice, and the unscheduled DNA synthesis assay in rats. Aripiprazole and a metabolite (2,3-DCPP) were clastogenic in the in vitrochromosomal aberration assay in CHL cells with and without metabolic activation. The metabolite, 2,3-DCPP, increased numerical aberrations in the in vitroassay in CHL cells in the absence of metabolic activation. A positive response was obtained in the in vivo micronucleus assay in mice; however, the response was due to a mechanism not considered relevant to humans.  Impairment of Fertility  Female rats were treated orally with aripiprazole from 2 weeks prior to mating through gestation Day 7 at doses of 2, 6, and 20 mg/kg/day, which are 0.6, 2, and 6 times the MRHD of 30 mg/day based on mg/m 2body surface area. Estrus cycle irregularities and increased corpora lutea were seen at all doses, but no impairment of fertility was seen. Increased  pre-implantation loss was seen at 2 and 6 times the MRHD, and decreased fetal weight was seen at 6 times the MRHD.  Male rats were treated orally with aripiprazole from 9 weeks prior to mating through mating at doses of 20, 40, and 60 mg/kg/day, which are 6, 13, and 19 times the MRHD of 30 mg/day based on mg/m 2body surface area. Disturbances in spermatogenesis were seen at 19 times the MRHD and prostate atrophy was seen at 13 and 19 times the MRHD without impairment of fertility.
13.2 Animal Toxicology and/or Pharmacology
Aripiprazole produced retinal degeneration in albino rats in a 26week chronic toxicity study at a dose of 60 mg/kg/day and in a 2year carcinogenicity study at doses of 40 and 60 mg/kg/day which are 13 and 19 times the MRHD of 30 mg/day based on mg/m 2body surface area. Evaluation of the retinas of albino mice and of monkeys did not reveal evidence of retinal degeneration. Additional studies to further evaluate the mechanism have not been performed. The relevance of this finding to human risk is unknown. 
14 Clinical Studies
Efficacy of the oral formulations of aripiprazole was established in the following adequate and well-controlled trials: ‚Äʬ†Four short-term trials and one maintenance trial in adult patients and one short-term trial in adolescents (ages 13 to 17 years) with schizophrenia [see clinical studies ( 14.1)] ‚Äʬ†Two short-term trials in pediatric patients (ages 6 to 18 years) with Tourette‚Äôs disorder [see Clinical Studies ( 14.5)]¬†
14.1 Schizophrenia
Adults  The efficacy of aripiprazole in the treatment of schizophrenia was evaluated in five short-term (4 week and 6 week), placebo-controlled trials of acutely relapsed inpatients who predominantly met DSM-III/IV criteria for schizophrenia. Four of the five trials were able to distinguish aripiprazole tablets from placebo, but one study, the smallest, did not. Three of these studies also included an active control group consisting of either risperidone (one trial) or haloperidol (two trials), but they were not designed to allow for a comparison of aripiprazole and the active comparators. 
In the four positive trials for aripiprazole, four primary measures were used for assessing psychiatric signs and symptoms. Efficacy was evaluated using the total score on the Positive and Negative Syndrome Scale (PANSS). The PANSS is a 30 li scale that measures positive symptoms of schizophrenia (7 lis), negative symptoms of schizophrenia (7 lis), and general psychopathology (16 lis), each rated on a scale of 1 (absent) to 7 (extreme); total PANSS scores range from 30 to 210. The Clinical Global Impression (CGI) assessment reflects the impression of a skilled observer, fully familiar with the manifestations of schizophrenia, about the overall clinical state of the patient. 
In a 4 week trial (n=414) comparing two fixed doses of aripiprazole (15 or 30 mg/day) to placebo, both doses of aripiprazole were superior to placebo in the PANSS total score (Study 1 in Table 26), PANSS positive subscale, and CGI-severity score. In addition, the 15 mg dose was superior to placebo in the PANSS negative subscale. 
In a 4 week trial (n=404) comparing two fixed doses of aripiprazole (20 or 30 mg/day) to placebo, both doses of aripiprazole were superior to placebo in the PANSS total score (Study 2 in Table 26), PANSS positive subscale, PANSS negative subscale, and CGI-severity score. 
In a 6 week trial (n=420) comparing three fixed doses of aripiprazole (10, 15, or 20 mg/day) to placebo, all three doses of aripiprazole were superior to placebo in the PANSS total score (Study 3 in Table 26), PANSS positive subscale, and the PANSS negative subscale.
In a 6 week trial (n=367) comparing three fixed doses of aripiprazole (2, 5, or 10 mg/day) to placebo, the 10 mg dose of aripiprazole was superior to placebo in the PANSS total score (Study 4 in Table 26), the primary outcome measure of the study. The 2 and 5 mg doses did not demonstrate superiority to placebo on the primary outcome measure. Thus, the efficacy of 10, 15, 20, and 30 mg daily doses was established in two studies for each dose. Among these doses, there was no evidence that the higher dose groups offered any advantage over the lowest dose group of these studies. 
Thus, the efficacy of 10, 15, 20, and 30 mg daily doses was established in two studies for each dose. Among these doses, there was no evidence that the higher dose groups offered any advantage over the lowest dose group of these studies. 
An examination of population subgroups did not reveal any clear evidence of differential responsiveness on the basis of age, gender, or race. 
A longer-term trial enrolled 310 inpatients or outpatients meeting DSM-IV criteria for schizophrenia who were, by history, symptomatically stable on other antipsychotic medications for periods of 3 months or longer. These patients were discontinued from their antipsychotic medications and randomized to aripiprazole 15 mg/day or placebo for up to 26 weeks of observation for relapse. Relapse during the double-blind phase was defined as CGI-Improvement score of ‚Č•5 (minimally worse), scores ‚Č•5 (moderately severe) on the hostility or uncooperativeness lis of the PANSS, or ‚Č•20% increase in the PANSS total score. Patients receiving aripiprazole tablets 15 mg/day experienced a significantly longer time to relapse over the subsequent 26 weeks compared to those receiving placebo (Study 5 in Figure 6).¬†
Pediatric Patients
 
The efficacy of aripiprazole in the treatment of schizophrenia in pediatric patients (13 to 17 years of age) was evaluated in one 6week, placebocontrolled trial of outpatients who met DSM-IV criteria for schizophrenia and had a PANSS score ‚Č•70 at baseline. In this trial (n=302) comparing two fixed doses of aripiprazole (10 or 30 mg/day) to placebo, aripiprazole was titrated starting from 2 mg/day to the target dose in 5 days in the 10 mg/day treatment arm and in 11 days in the 30 mg/day treatment arm. Both doses of aripiprazole were superior to placebo in the PANSS total score (Study 6 in Table 26), the primary outcome measure of the study. The 30 mg/day dosage was not shown to be more efficacious than the 10 mg/day dose. Although maintenance efficacy in pediatric patients has not been systematically evaluated, maintenance efficacy can be extrapolated from adult data along with comparisons of aripiprazole pharmacokinetic parameters in adult and pediatric patients.¬† Table 26: Schizophrenia Studies
S tudy Number Treatment Group P rimary Efficacy Measure: PANNS     Mean Baseline Score (SD) LS M ean Change from Baseline (SE) P lacebo subtracted Difference * (95% CI) Study 1 Aripiprazole Tablets (15 mg/day) † Aripiprazole Tablets (30 mg/day) † Placebo 98.5 (17.2) 99 (19.2) 100.2 (16.5) -15.5(2.40) -11.4 (2.39) -2.9 (2.36) -12.6 (-18.9, -6.2) -8.5 (-14.8, -2.1) -- Study 2 Aripiprazole Tablets (20 mg/day) † Aripiprazole Tablets (30 mg/day) † Placebo 92.6 (19.5) 94.2 (18.5) 94.3 (18.5) -14.5(2.23) -13.9(2.24) -5.0 (2.17) -9.6 (-15.4, -3.8) -9 (-14.8, -3.1) -- Study 3 Aripiprazole Tablets (10 mg/day) † Aripiprazole Tablets (15 mg/day) † Aripiprazole Tablets (20 mg/day) † Placebo 92.7(19.5)   93.2 (21.6)   92.5 (20.9)   92.3 (21.8) -15.0(2.38)   -11.7 (2.38)   -14.4(2.45)   -2.3 (2.35) -12.7 (-19, -6.41)    -9.4 (-15.71, 3.08)    -12.1(-18.53,5.68)  -- Study 4 Aripiprazole Tablets (2 mg/day) Aripiprazole Tablets (5 mg/day) Aripiprazole Tablets (10 mg/day) † Placebo 90.7(14.5) 92.0 (12.6) 90.0 (11.9) 90.8 (13.3) -8.2 (1.90) -10.6(1.93) -11.3 (1.88) -5.3 (1.97) -2.9 (-8.29, 2.47) -5.2 (-10.7, 0.19) -5.9 (-11.3, -0.58) -- Study 6 (Pediatric, 13 to 17 Years) Aripiprazole Tablets (10 mg/day) † Aripiprazole Tablets (30 mg/day) † Placebo 93.6 (15.7) 94.0 (16.1) 94.6 (15.6) -26.7(1.91)   -28.6(1.92)   -21.2(1.93) -5.5 (-10.7, -0.21)   -7.4 (-12.7, -2.13)   --
SD: standard deviation; SE: standard error; LS Mean: least-squares mean; CI: unadjusted confidence interval.  *Difference (drug minus placebo) in least-squares mean change from baseline.  †Doses statistically significantly superior to placebo. Figure 6: Kaplan-Meier Estimation of Cumulative Proportion of Patients with Relapse (Schizophrenia Study 5)
14.2 Bipolar Disorder
Additional pediatric use information is approved for Otsuka America Pharmaceutical, Inc.‚Äôs ABILIFY ¬ģ(aripiprazole) product. However, due to Otsuka America Pharmaceutical, Inc.‚Äôs marketing exclusivity rights, this drug product is not labeled with that information. Maintenance Treatment of Bipolar I Disorder¬† Monotherapy Maintenance Therapy
 
A maintenance trial was conducted in adult patients meeting DSM-IV criteria for bipolar I disorder with a recent manic or mixed episode who had been stabilized on open-label aripiprazole and who had maintained a clinical response for at least 6 weeks. The first phase of this trial was an open-label stabilization period in which inpatients and outpatients were clinically stabilized and then maintained on open-label aripiprazole (15 or 30 mg/day, with a starting dose of 30 mg/day) for at least 6 consecutive weeks. One hundred sixty-one outpatients were then randomized in a double-blind fashion, to either the same dose of aripiprazole they were on at the end of the stabilization and maintenance period or placebo and were then monitored for manic or depressive relapse. During the randomization phase, aripiprazole was superior to placebo on time to the number of combined affective relapses (manic plus depressive), the primary outcome measure for this study (Study 7 in Figure 7). A total of 55 mood events were observed during the double-blind treatment phase. Nineteen were from the aripiprazole group and 36 were from the placebo group. The number of observed manic episodes in the aripiprazole group (6) were fewer than that in the placebo group (19), while the number of depressive episodes in the aripiprazole group (9) was similar to that in the placebo group (11).
An examination of population subgroups did not reveal any clear evidence of differential responsiveness on the basis of age and gender; however, there were insufficient numbers of patients in each of the ethnic groups to adequately assess inter-group differences. Figure 7: Kaplan-Meier Estimation of Cumulative Proportion of Patients with Relapse (Bipolar Study 7)
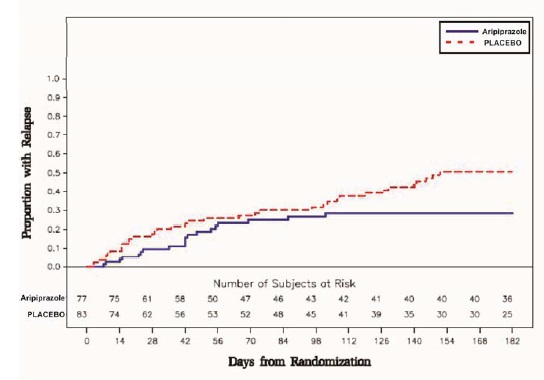
 
Adjunctive Maintenance Therapy¬† An adjunctive maintenance trial was conducted in adult patients meeting DSM-IV criteria for bipolar I disorder with a recent manic or mixed episode. Patients were initiated on open-label lithium (0.6 to 1.0 mEq/L) or valproate (50 to 125 mcg /mL) at therapeutic serum levels, and remained on stable doses for 2 weeks. At the end of 2 weeks, patients demonstrating inadequate response (Y-MRS total score ‚Č•16 and ‚ȧ35% improvement on the Y-MRS total score) to lithium or valproate received aripiprazole with a starting dose of 15 mg/day with the option to increase to 30 mg or reduce to 10 mg as early as Day 4, as adjunctive therapy with open-label lithium or valproate. Prior to randomization, patients on the combination of single-blind aripiprazole and lithium or valproate were required to maintain stability (Y-MRS and MADRS total scores ‚ȧ12) for 12 consecutive weeks. Three hundred thirty-seven patients were then randomized in a double-blind fashion, to either the same dose of aripiprazole they were on at the end of the stabilization period or placebo plus lithium or valproate and were then monitored for manic, mixed, or depressive relapse for a maximum of 52 weeks. Aripiprazole was superior to placebo on the primary endpoint, time from randomization to relapse to any mood event (Study 8 in Figure 8). A mood event was defined as hospitalization for a manic, mixed, or depressive episode, study discontinuation due to lack of efficacy accompanied by Y-MRS score >16 and/or a MADRS >16, or an SAE of worsening disease accompanied by Y-MRS score >16 and/or a MADRS >16. A total of 68 mood events were observed during the double-blind treatment phase. Twenty-five were from the aripiprazole group and 43 were from the placebo group. The number of observed manic episodes in the aripiprazole group (7) were fewer than that in the placebo group (19), while the number of depressive episodes in the aripiprazole group (14) was similar to that in the placebo group (18). The Kaplan-Meier curves of the time from randomization to relapse to any mood event during the 52week, double-blind treatment phase for aripiprazole and placebo groups are shown in Figure 8. An examination of population subgroups did not reveal any clear evidence of differential responsiveness on the basis of age and gender; however, there were insufficient numbers of patients in each of the ethnic groups to adequately assess inter-group differences.
Figure 8: Kaplan-Meier Estimation of Cumulative Proportion of Patients with Relapse to Any Mood Event (Bipolar Study 8)
14.5 Tourettes Disorder
Pediatric Patients¬† The efficacy of aripiprazole in the treatment of Tourette‚Äôs disorder was established in one 8 week (7 to 17 years of age) and one 10 week (6 to 18 years of age), placebo-controlled trials in pediatric patients (6 to 18 years of age) who met the DSM-IV criteria for Tourette‚Äôs disorder and had a Total Tic score (TTS) ‚Č•20 to 22 on the Yale Global Tic Severity Scale (YGTSS). The YGTSS is a fully validated scale designed to measure current tic severity. Efficacy was evaluated using two assessment scales: 1) the Total Tic score (TTS) of the YGTSS and 2) the Clinical Global Impressions Scale for Tourette‚Äôs Syndrome (CGI-TS), a clinician-determined summary measure that takes into account all available patient information.¬† Over 65% of these patients were under 13 years of age.¬† The primary outcome measure in both trials was the change from baseline to endpoint in the TTS of the YGTSS. Ratings for the TTS are made along 5 different dimensions on a scale of 0 to 5 for motor and vocal tics each. Summation of these 10 scores provides a TTS (i.e., 0 to 50).¬† The results of these trials are as follows:¬† In the 8 week, placebo-controlled, fixed-dose trial, children and adolescents with Tourette‚Äôs disorder (n=133), aged 7 to 17 years, were randomized 1:1:1 to low dose aripiprazole, high dose aripiprazole, or placebo. The target doses for the low and high dose aripiprazole groups were based on weight. Patients <50 kg in the low dose aripiprazole group started at 2 mg per day with a target dose of 5 mg per day after 2 days. Patients ‚Č•50 kg in the low dose aripiprazole group, started at 2 mg per day increased to 5 mg per day after 2 days, with a subsequent increase to a target dose of 10 mg per day at Day 7. Patients <50 kg in the high dose aripiprazole group started at 2 mg per day increased to 5 mg per day after 2 days, with a subsequent increase to a target dose of 10 mg per day at Day 7. Patients ‚Č•50 kg in the high dose aripiprazole group, started at 2 mg per day increased to 5 mg per day after 2 days, with a subsequent increase to a dose of 10 mg per day at Day 7 and were allowed weekly increases of 5 mg per day up to a target dose 20 mg per day at Day 21. Aripiprazole (both high and low dose groups) demonstrated statistically significantly improved scores on the YGTSS TTS (Study 1 in Table 30) and on the CGI-TS scale compared with placebo. The estimated improvements on the YGTSS TTS over the course of the study are displayed in Figure 9. Figure 9: Least Square Means of Change from Baseline in YGTSS TTS by Week (Tourette‚Äôs Disorder Study 1)
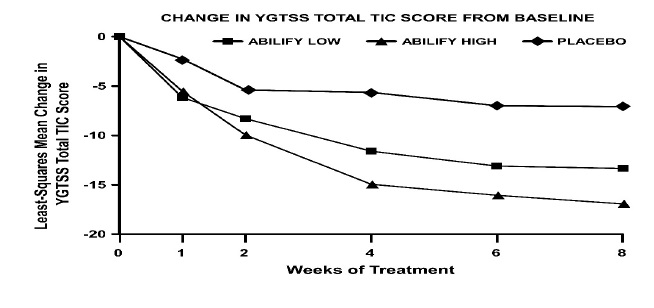
In the 10 week, placebo-controlled, flexible-dose trial in children and adolescents with Tourette’s disorder (n=61), aged 6 to 18 years, patients received daily doses of placebo or aripiprazole, starting at 2 mg/day with increases allowed up to 20 mg/day based on clinical response. Aripiprazole demonstrated statistically significantly improved scores on the YGTSS TTS scale compared with placebo (Study 2 in Table 30). The mean daily dose of aripiprazole at the end of 10 week treatment was 6.54 mg/day.
. Table 30: Tourette’s Disorder Studies (Pediatric)
S tudy Number Treatment Group  P rimary Efficacy Measure: YGTSS TTS     Mean Baseline Score (SD) LS M ean Change from Baseline (SE) P lacebo subtracted Difference * (95% CI) Study 1 Aripiprazole Tablets (low dose) † Aripiprazole Tablets (high dose) † Placebo 29.2 (5.63) 31.2 (6.40) 30.7 (5.95) -13.4 (1.59) -16.9 (1.61) -7.1 (1.55) -6.3 (-10.2, -2.3) -9.9 (-13.8, -5.9) -- Study 2 Aripiprazole Tablets (2 to 20 mg/day) † Placebo 28.3 (5.51)   29.5 (5.60) -15.0 (1.51)   -9.6 (1.64) -5.3 (-9.8, -0.9)   --
SD: standard deviation; SE: standard error; LS Mean: least-squares mean; CI: unadjusted confidence interval. *Difference (drug minus placebo) in least-squares mean change from baseline. ‚ĆDoses statistically significantly superior to placebo. Additional pediatric use information is approved for Otsuka America Pharmaceutical, Inc.‚Äôs ABILIFY¬ģ (aripiprazole) product. However, due to Otsuka America Pharmaceutical, Inc.‚Äôs marketing exclusivity rights, this drug product is not labeled with that information.
16 How Supplied/storage And Handling
16.1 How Supplied
Aripiprazole tablets, USP 2 mg are light green to green, modified rectangular, bevel edged biconvex plain to mottled tablets debossed with 'I' on one side and '94' on other side. Bottles of 30 Tablets                                                     NDC 31722-819-30 Bottles of 100 Tablets                                                   NDC 31722-819-01 Bottles of 500 Tablets                                                  NDC 31722-819-05 Buler card of 10 Unit dose tablets                              NDC 31722-819-31 Buler pack of 250 (25 x 10) Unit dose tablets            NDC 31722-819-32 Aripiprazole tablets, USP 5 mg are light blue to blue, modified rectangular, bevel edged biconvex tablets debossed with 'I' on one side and '95' on other side. Bottles of 30 Tablets                                                     NDC 31722-820-30 Bottles of 100 Tablets                                                   NDC 31722-820-01 Bottles of 500 Tablets                                                  NDC 31722-820-05 Buler card of 10 Unit dose tablets                              NDC 31722-820-31 Buler pack of 250 (25 x 10) Unit dose tablets            NDC 31722-820-32 Aripiprazole tablets, USP 10 mg are light pink to pink, modified rectangular, bevel edged biconvex plain to mottled tablets debossed with 'I' on one side and '96' on other side. Bottles of 30 Tablets                                                     NDC 31722-827-30 Bottles of 100 Tablets                                                   NDC 31722-827-01 Bottles of 500 Tablets                                                   NDC 31722-827-05 Buler card of 10 Unit dose tablets                               NDC 31722-827-31 Buler pack of 250 (25 x 10) Unit dose tablets             NDC 31722-827-32 Aripiprazole tablets, USP 15 mg are light yellow to yellow, round, bevel edged biconvex  plain to mottled tablets debossed with 'I' on one side and '97' on other side. Bottles of 30 Tablets                                                      NDC 31722-828-30 Bottles of 100 Tablets                                                    NDC 31722-828-01 Bottles of 500 Tablets                                                     NDC 31722-828-05 Buler card of 10 Unit dose tablets                                NDC 31722-828-31 Buler pack of 250 (25 x 10) Unit dose tablets              NDC 31722-828-32 Aripiprazole tablets, USP 20 mg are white to off-white, round, bevel edged biconvex tablets debossed with 'I' on one side and '98' on other side. Bottles of 30 Tablets                                                       NDC 31722-829-30 Bottles of 100 Tablets                                                     NDC 31722-829-01 Bottles of 500 Tablets                                                     NDC 31722-829-05 Buler card of 10 Unit dose tablets                                 NDC 31722-829-31 Buler pack of 250 (25 x 10) Unit dose tablets               NDC 31722-829-32 Aripiprazole tablets, USP 30 mg are light pink to pink, round, bevel edged biconvex plain to mottled tablets debossed with 'I' on one side and '99' on other side. Bottles of 30 Tablets                                                         NDC 31722-830-30 Bottles of 100 Tablets                                                       NDC 31722-830-01 Bottles of 500 Tablets                                                       NDC 31722-830-05 Buler card of 10 Unit dose tablets                                  NDC 31722-830-31 Buler pack of 250 (25 x 10) Unit dose tablets                NDC 31722-830-32
16.2 Storage
Store at 20¬ļ to 25¬ļ C (68¬ļ to 77¬ļF) [see USP Controlled Room Temperature].
17 Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling ( Medication Guide).  Discuss the following issues with patients prescribed aripiprazole tablets: Clinical Worsening of Depression and Suicide Risk Patients, their families, and their caregivers should be encouraged to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, worsening of depression, and suicidal ideation, especially early during antidepressant treatment and when the dose is adjusted up or down. Families and caregivers of patients should be advised to look for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient’s prescriber or health professional, especially if they are severe, abrupt in onset, or were not part of the patient’s presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior and indicate a need for very close monitoring and possibly changes in the medication [see Warnings and Precautions (5.3)] .
Prescribers or other health professionals should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with aripiprazole tablets and should counsel them in its appropriate use. A patient Medication Guide including information about ‚ÄúAntidepressant Medicines, Depression and other Serious Mental Illness, and Suicidal Thoughts or Actions‚ÄĚ is available for aripiprazole tablets. The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. It should be noted that aripiprazole tablets are not approved as a single agent for treatment of depression and has not been evaluated in pediatric major depressive disorder. Pathological Gambling and Other Compulsive Behaviors¬† Advise patients and their caregivers of the possibility that they may experience compulsive urges to shop, intense urges to gamble, compulsive sexual urges, binge eating and/or other compulsive urges and the inability to control these urges while taking aripiprazole. In some cases, but not all, the urges were reported to have stopped when the dose was reduced or stopped [see Warnings and Precautions (5.7)]. Interference with Cognitive and Motor Performance¬† Because aripiprazole tablets may have the potential to impair judgment, thinking, or motor skills, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that aripiprazole therapy does not affect them adversely [see Warnings and Precautions (5.12)] .¬† Concomitant Medication¬† Patients should be advised to inform their physicians if they are taking, or plan to take, any prescription or over-the-counter drugs, since there is a potential for interactions [see Drug Interactions (7)] .¬† Heat Exposure and Dehydration¬† Patients should be advised regarding appropriate care in avoiding overheating and dehydration [see Warnings and Precautions (5.13)] .¬† Pregnancy¬† Advise patients to notify their healthcare provider if they become pregnant or intend to become pregnant during treatment with aripiprazole. Advise patients that aripiprazole may cause extrapyramidal and/or withdrawal symptoms (agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress, and feeding disorder) in a neonate. Advise patients that there is a pregnancy registry that monitors pregnancy outcomes in women exposed to Aripiprazole during pregnancy [see Use in Specific Populations (8.1)]. Manufactured by:¬†

Manufactured for: Camber Pharmaceuticals, Inc., Piscataway, NJ 08854 By: HETERO TM Hetero Labs Limited, Unit V, Polepally, Jadcherla, Mahabubnagar - 509 301, India. Revised: 05/2023
Medication Guide
Aripiprazole Tablets USP (ar'' i pip' ra zole) ¬† ¬†What is the most important information I should know about aripiprazole tablets?¬† (For other side effects, also see ‚ÄúWhat are the possible side effects of aripiprazole tablets?‚ÄĚ)¬† Serious side effects may happen when you take aripiprazole tablets, including:¬† ‚ÄĘ Increased risk of death in elderly patients with dementia-related psychosis:Medicines like aripiprazole tablets can raise the risk of death in elderly people who have lost touch with reality (psychosis) due to confusion and memory loss (dementia). Aripiprazole tablets are not approved for the treatment of patients with dementia-related psychosis.¬† ‚ÄĘ Risk of suicidal thoughts or actions:Antidepressant medicines, depression and other serious mental illnesses, and suicidal thoughts or actions:¬† ‚Äʬ† Antidepressant medicines may increase suicidal thoughts or actions in some children, teenagers, and young adults within the first few months of treatment.¬† ‚Äʬ†Depression and other serious mental illnesses are the most important causes of suicidal thoughts and actions. Some people may have a particularly high risk of having suicidal thoughts or actions. These include people who have (or have a family history of) suicidal thoughts or actions. ‚Äʬ† How can I watch for and try to prevent suicidal thoughts and actions in myself or a¬† family member?¬† ‚Äʬ†Pay close attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings. This is very important when an antidepressant medicine is started or when the dose is changed.¬† ¬†Call the healthcare provider right away to report new or sudden changes in mood, behavior, thoughts, or feelings.¬† ‚Äʬ†Keep all follow-up visits with the healthcare provider as scheduled. Call the healthcare provider between visits as needed, especially if you have concerns about symptoms.¬† Call a healthcare provider right away if you or your family member has any of the following symptoms, especially if they are new, worse, or worry you: ‚Äʬ†thoughts about suicide or dying¬† ‚Äʬ†attempts to commit suicide¬† ‚Äʬ†new or worse depression¬† ‚Äʬ†new or worse anxiety¬† ‚Äʬ†feeling very agitated or restless¬† ‚Äʬ†panic attacks¬† ‚Äʬ†trouble sleeping (insomnia)¬† ‚Äʬ†new or worse irritability¬† ‚Äʬ†acting aggressive, being angry, or violent¬† ‚Äʬ†acting on dangerous impulses¬† ‚Äʬ†an extreme increase in activity and talking (mania)¬† ‚Äʬ†other unusual changes in behavior or mood¬† What else do I need to know about antidepressant medicines? ‚Äʬ† Never stop an antidepressant medicine without first talking to a healthcare provider.Stopping an antidepressant medicine suddenly can cause other symptoms.¬† ‚Äʬ† Antidepressants are medicines used to treat depression and other illnesses.It is important to discuss all the risks of treating depression and also the risks of not treating it. Patients and their families or other caregivers should discuss all treatment choices with the healthcare provider, not just the use of antidepressants.¬† ‚Äʬ† Antidepressant medicines have other side effects.Talk to the healthcare provider about the side effects of the medicine prescribed for you or your family member.¬† ‚Äʬ† Antidepressant medicines can interact with other medicines.Know all of the medicines that you or your family member takes. Keep a ul of all medicines to show the healthcare provider. Do not start new medicines without first checking with your healthcare provider.¬† ‚Äʬ† Not all antidepressant medicines prescribed for children are FDA approved for use in children.Talk to your child‚Äôs healthcare provider for more information.¬† ¬†What are aripiprazole tablets? ‚Äʬ†Aripiprazole tablets are prescription medicine used to treat:¬† ‚Äʬ†Schizophrenia¬† ‚Äʬ†Tourette‚Äôs disorder It is not known if aripiprazole tablets are safe or effective in children: ‚Äʬ†under 13 years of age with schizophrenia¬†¬† ‚Äʬ†under 6 years of age with Tourette‚Äôs disorder ¬† Do not take aripiprazole tablets if youare allergic to aripiprazole or any of the ingredients in aripiprazole tablets. See the end of this Medication Guide for a complete ul of ingredients in aripiprazole tablets. ¬†Before taking aripiprazole tablets, tell your healthcare provider about all your medical conditations, including if you have or had:¬† ‚Äʬ†diabetes or high blood sugar in you or your family; your healthcare provider should check your blood sugar before you start aripiprazole tablets and also during therapy.¬† ‚Äʬ†seizures (convulsions).¬† ‚Äʬ†low or high blood pressure.¬† ‚Äʬ†heart problems or stroke.¬† ‚Äʬ†pregnancy or plans to become pregnant. It is not known if aripiprazole tablets will harm your unborn baby.¬† ‚Äʬ†If you become pregnant while receiving aripiprazole tablets, talk to your healthcare provider about registering with the National Pregnancy Registry for Atypical Antipsychotics. You can register by calling 1-866-961-2388 or go to http://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/.¬†¬† ‚Äʬ†breast-feeding or plans to breast-feed. Aripiprazole passes into your breast milk. Talk to your healthcare provider about the best way to feed your baby if you receive aripiprazole tablets.¬† ‚Äʬ†low white blood cell count.¬† Tell your healthcare provider about all the medicines that you take,including prescription and over-the-counter medicines, vitamins, and herbal supplements. Aripiprazole tablets and other medicines may affect each other causing possible serious side effects. Aripiprazole tablets may affect the way other medicines work, and other medicines may affect how aripiprazole tablets works.¬† Your healthcare provider can tell you if it is safe to take aripiprazole tablets with your other medicines. Do not start or stop any medicines while taking aripiprazole tablets without talking to your healthcare provider first. Know the medicines you take. Keep a ul of your medicines to show your healthcare provider and pharmacist when you get a new medicine.¬† ¬† How should I take aripiprazole tablets? ‚Äʬ†Take aripiprazole tablets exactly as your healthcare provider tells you to take it. Do not change the dose or stop taking aripiprazole tablets yourself.¬† ‚Äʬ†Aripiprazole tablets can be taken with or without food.¬† ‚Äʬ†Aripiprazole tablets should be swallowed whole.¬† ‚Äʬ†If you miss a dose of aripiprazole tablets, take the missed dose as soon as you remember. If it is almost time for the next dose, just skip the missed dose and take your next dose at the regular time. Do not take two doses of aripiprazole tablets at the same time.¬† ‚Äʬ†If you take too much aripiprazole tablets, call your healthcare provider or poison control center at 1-800-222-1222 right away, or go to the nearest hospital emergency room. ¬†What should I avoid while taking aripiprazole tablets?¬† ‚Äʬ†Do not drive, operate heavy machinery, or do other dangerous activities until you know how aripiprazole tablets affects you. Aripiprazole tablets may make you drowsy.¬† ‚Äʬ†Avoid getting over-heated or dehydrated.¬† ‚Äʬ†Do not over-exercise.¬† ‚Äʬ†In hot weather, stay inside in a cool place if possible.¬† ‚Äʬ†Stay out of the sun. Do not wear too much or heavy clothing.¬† ‚Äʬ†Drink plenty of water.¬† ¬†What are the possible side effects of aripiprazole tablets?¬† Aripiprazole tablets may cause serious side effects, including: ‚Äʬ†See ‚ÄúWhat is the most important information I should know about aripiprazole tablets?‚Ä̬† ‚Äʬ†Stroke in elderly people (cerebrovascular problems) that can lead to death ‚Äʬ† Neuroleptic malignant syndrome (NMS):Tell your healthcare provider right away if you have some or all of the following symptoms: high fever, stiff muscles, confusion, sweating, changes in pulse, heart rate, and blood pressure. These may be symptoms of a rare and serious condition that can lead to death. Call your healthcare provider right away if you have any of these symptoms.¬† ‚Äʬ† Uncontrolled body movements (tardive dyskinesia).Aripiprazole tablets may cause movements that you cannot control in your face, tongue, or other body parts. Tardive dyskinesia may not go away, even if you stop receiving aripiprazole tablets. Tardive dyskinesia may also start after you stop receiving aripiprazole tablets. ‚Äʬ†Problems with your metabolism such as: ‚Äʬ† High blood sugar (hyperglycemia) and diabetes:Increases in blood sugar can happen in some people who take aripiprazole tablets. Extremely high blood sugar can lead to coma or death. If you have diabetes or risk factors for diabetes (such as being overweight or a family history of diabetes), your healthcare provider should check your blood sugar before you start aripiprazole tablets and during your treatment.¬† Call your healthcare provider if you have any of these symptoms of high blood sugar while receiving aripiprazole tablets:¬† ‚Äʬ†feel very thirsty¬† ‚Äʬ†need to urinate more than usual¬† ‚Äʬ†feel very hungry¬† ‚Äʬ†feel weak or tired¬† ‚Äʬ†feel sick to your stomach¬† ‚Äʬ†feel confused, or your breath smells fruity¬† ‚Äʬ†Increased fat levels (cholesterol and triglycerides) in your blood. ‚Äʬ† Weight gain.You and your healthcare provider should check your weight regularly. ‚Äʬ† Unusual urges.Some people taking aripiprazole tablets have had unusual urges, such as gambling, binge eating or eating that you cannot control (compulsive), compulsive shopping and sexual urges.¬† If you or your family members notice that you are having unusual urges or behaviors, talk to your healthcare provider. ‚Äʬ† Orthostatic hypotension (decreased blood pressure):Lightheadedness or fainting may happen when rising too quickly from a sitting or lying position.¬† ‚Äʬ† Falls.Aripiprazole tablets may make you sleepy or dizzy, may cause a decrease in your blood pressure when changing position and can slow your thinking and motor skills which may lead to falls that can cause fractures or other injuries.¬† ‚Äʬ†Low white blood cell count¬† ‚Äʬ†Seizures (convulsions)¬† ‚Äʬ† Problems with control of your body temperature especially when you exercise a lot or are in an area that is very hot. It is important for you to drink water to avoid dehydration.See ‚ÄúWhat should I avoid while receiving aripiprazole tablets?‚ÄĚ The most common side effects of aripiprazole tablets in adults include: ‚ÄĘ nausea ¬†¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬†¬† ‚ÄĘ vomiting ¬†¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ‚ÄĘ constipation¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬†¬† ‚ÄĘ headache¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬†¬† ‚ÄĘ blurred vision ‚ÄĘ upper respiratory illness¬† ‚ÄĘ dizziness ‚Äʬ†anxiety ‚ÄĘ insomnia ‚Äʬ†restlessness¬† ‚ÄĘ inner sense of restlessness/need to move (akathisia) ¬† The most common side effects of aripiprazole tablets in children include:¬† ‚Äʬ†feeling sleepy¬† ¬† ¬† ¬† ¬† ¬†¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬†¬† ‚Äʬ†headache¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬†¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬†¬† ‚Äʬ†vomiting¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬†¬†¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬†¬† ‚Äʬ†fatigue¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬†¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ‚Äʬ†increased or decreased appetite¬† ‚Äʬ†increased saliva or drooling¬† ‚ÄĘ insomnia ¬†‚Äʬ†nausea ‚Äʬ†stuffy nose ‚Äʬ†weight gain¬† ‚Äʬ†uncontrolled movement such as restlessness, tremor¬† ‚Äʬ†muscle stiffness These are not all the possible side effects of aripiprazole tablets.¬† Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.¬† ¬†How should I store aripiprazole tablets?¬† Store aripiprazole tablets at 68¬ļ to 77¬ļF (20¬ļ to 25¬ļ C). Keep aripiprazole tablets and all medicines out of the reach of children. ¬†General information about the safe and effective use of aripiprazole tablets¬† Medicines are sometimes prescribed for purposes other than those uled in a Medication Guide. Do not use aripiprazole tablets for a condition for which it was not prescribed. Do not give aripiprazole tablets to other people, even if they have the same symptoms you have. It may harm them. You can ask your healthcare provider or pharmacist for information about aripiprazole tablets that was written for healthcare professionals.¬† For more information, call 1-866-495-1995 ¬†What are the ingredients in aripiprazole tablets? Active ingredient:aripiprazole USP Inactive ingredients:corn starch, FD&C Blue #2/Indigo Carmine Al, ferric oxide red, ferric oxide yellow, hydroxypropyl cellulose, lactose monohydrate, magnesium stearate and microcrystalline cellulose Additional pediatric use information is approved for Otsuka America Pharmaceutical, Inc.‚Äôs ABILIFY ¬ģ(aripiprazole) product. However, due to Otsuka America Pharmaceutical, Inc.‚Äôs marketing exclusivity rights, this drug product is not labeled with that information. Manufactured for: Camber Pharmaceuticals, Inc., Piscataway, NJ 08854 By: HETERO TM Hetero Labs Limited, Unit V, Polepally, Jadcherla, Mahabubnagar - 509 301, India.
This Medication Guide has been approved by the U.S. Food and Drug Administration Revised: 05/2023
Package Label.principal Display Panel
2 mg 30s count5 mg 30s count
10 mg 30s count15 mg 30s count
20 mg 30s count
30 mg 30s count
2 mg 500s count
5 mg 500s count
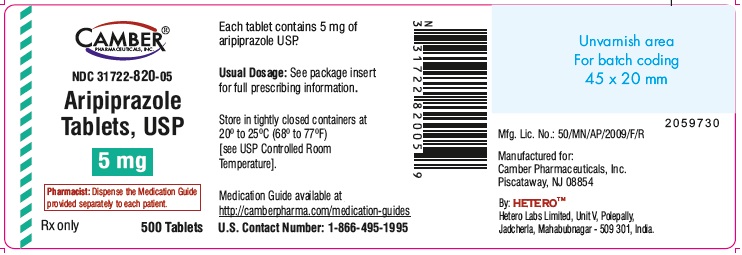
10 mg 500s count
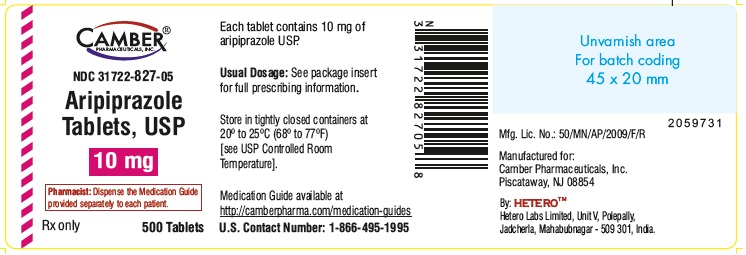
15 mg 500s count
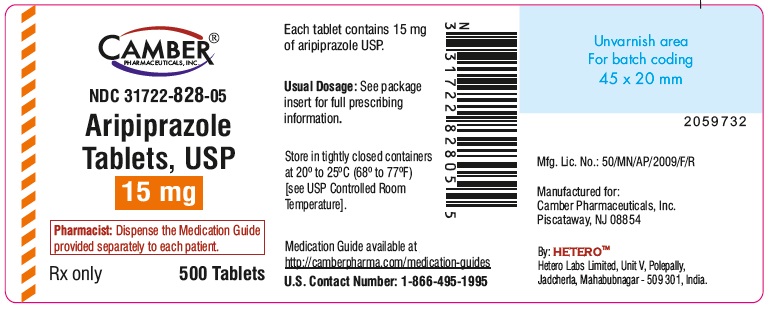
20 mg 500s count
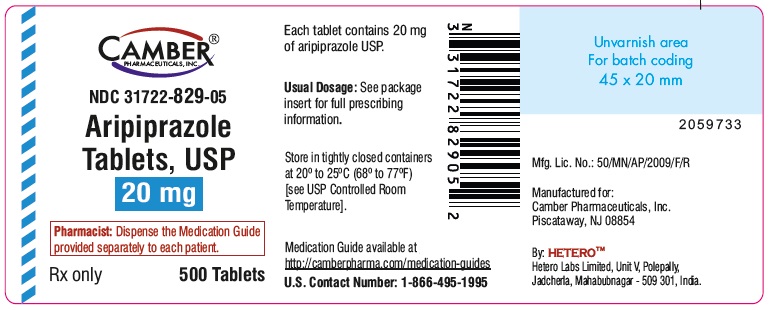
30 mg 500s count
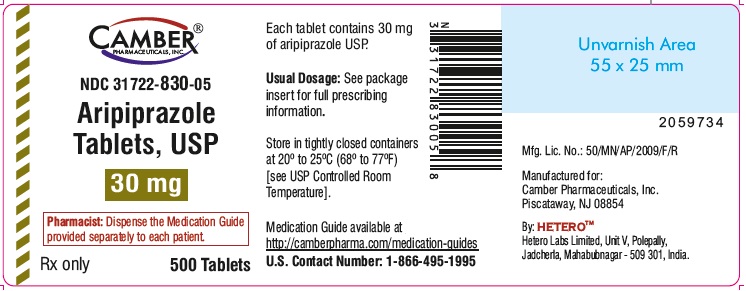
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site