Bortezomib Dailymed
Generic: bortezomib is used for the treatment of Multiple Myeloma Pregnancy Lymphoma, Mantle-Cell
Go PRO for all pill images
1 Indications And Usage
Bortezomib for injection is a proteasome inhibitor indicated for:
- treatment of adult patients with multiple myeloma (
1.1 )- treatment of adult patients with mantle cell lymphoma (
1.2 )1.1 Multiple Myeloma
Bortezomib for injection is indicated for the treatment of adult patients with multiple myeloma.
1.2 Mantle Cell Lymphoma
Bortezomib for injection is indicated for the treatment of adult patients with mantle cell lymphoma.
2 Dosage And Administration
- For subcutaneous or intravenous use only. Each route of administration has a different reconstituted concentration. Exercise caution when calculating the volume to be administered. (
2.1 ,2.10 )- The recommended starting dose of bortezomib for injection is 1.3 mg/m 2 administered either as a 3 to 5 second bolus intravenous injection or subcutaneous injection. (
2.2 ,2.4 ,2.6 )- Retreatment for Multiple Myeloma: May retreat starting at the last tolerated dose. (
2.6 )- Hepatic Impairment: Use a lower starting dose for patients with moderate or severe hepatic impairment. (
2.8 )- Dose must be individualized to prevent overdose. (
2.10 )2.1Important Dosing Guidelines
Bortezomib for injection is for intravenous or subcutaneous use only. Do not administer bortezomib for injection by any other route. Because each route of administration has a different reconstituted concentration, use caution when calculating the volume to be administered. The recommended starting dose of Bortezomib for injection is 1.3 mg/m 2. Bortezomib for injection is administered intravenously at a concentration of 1 mg/mL, or subcutaneously at a concentration of 2.5 mg/mL [ see Dosage and Administration (2.10)]. Bortezomib for injection retreatment may be considered for patients with multiple myeloma who had previously responded to treatment with bortezomib for injection and who have relapsed at least six months after completing prior bortezomib for injection treatment. Treatment may be started at the last tolerated dose [see Dosage and Administration (2.6)]. When administered intravenously, administer bortezomib for injection as a 3 to 5 second bolus intravenous injection.
2.2Dosage in Previously Untreated Multiple Myeloma
Bortezomib for injection is administered in combination with oral melphalan and oral prednisone for 9, six week treatment cycles as shown in Table 1.  In Cycles 1to 4, bortezomib for injection is administered twice weekly (Days 1, 4, 8, 11, 22, 25, 29 and 32). In Cycles 5 to 9, bortezomib for injection is administered once weekly (Days 1, 8, 22 and 29). At least 72 hours should elapse between consecutive doses of bortezomib for injection.
Table 1: Dosage Regimen for Patients with Previously Untreated Multiple Myeloma
Twice Weekly Bortezomib for Injection (Cycles 1 to 4)
Week
1
2
3
4
5
6
Bortezomib for Injection (1.3 mg/m 2)
Day 1
--
--
Day 4
Day 8
Day 11
rest period
Day 22
Day 25
Day 29
Day 32
rest period
Melphalan (9 mg/m 2) Prednisone (60 mg/m 2)
Day 1
Day 2
Day 3
Day 4
--
--
rest period
--
--
--
--
rest period
Once Weekly Bortezomib for Injection (Cycles 5 to 9 when used in combination with Melphalan and Prednisone)
Week
1
2
3
4
5
6
Bortezomib for Injection (1.3 mg/m 2)
Day 1
--
--
 
Day 8
 
rest period
Day 22
 
Day 29
 
rest period
Melphalan (9 mg/m 2) Prednisone (60 mg/m 2)
Day 1
Day 2
Day 3
Day 4
--
--
rest period
--
--
--
--
rest period
2.3Dose Modification Guidelines for Bortezomib for Injection When Given in Combination with Melphalan and Prednisone
Prior to initiating any cycle of therapy with bortezomib for injection in combination with melphalan and prednisone:
- Platelet count should be at least 70 x 10 9/L and the absolute neutrophil count (ANC) should be at least 1 x 10 9/L
- Nonhematological toxicities should have resolved to Grade 1 or baseline
Table 2: Dose Modifications During Cycles of Combination Bortezomib for Injection, Melphalan and Prednisone Therapy
Toxicity
Dose Modification or Delay
Hematological toxicity during a cycle: If prolonged Grade 4 neutropenia or thrombocytopenia, or thrombocytopenia with bleeding is observed in the previous cycle
Consider reduction of the melphalan dose by 25% in the next cycle
If platelet count is not above 30 √ó 10 9/L or ANC is not above 0.75 x 10 9/L on a bortezomib for injectiondosing day (other than Day 1)
Withhold bortezomib for injection dose
If several bortezomib for injection doses in consecutive cycles are withheld due to toxicity
Reduce bortezomib for injection dose by one dose level (from 1.3 mg/m 2 to 1 mg/m 2, or from 1 mg/m 2 to 0.7 mg/m 2)
Grade 3 or higher nonhematological toxicities
Withhold bortezomib for injection therapy until symptoms of toxicity have resolved to Grade 1 or baseline. Then, bortezomib for injection may be reinitiated with one dose level reduction (from 1.3 mg/m 2 to 1 mg/m 2, or from 1 mg/m 2 to 0.7 mg/m 2). For bortezomib for injection -related neuropathic pain and/or peripheral neuropathy, hold or modify bortezomib for injection as outlined in Table 5.
For information concerning melphalan and prednisone, see manufacturer's prescribing information. Dose modifications guidelines for peripheral neuropathy are provided [see Dosage and Administration (2.7)].
2.4Dosage in Previously Untreated Mantle Cell Lymphoma
Bortezomib for injection (1.3 mg/m 2) is administered intravenously in combination with intravenous rituximab, cyclophosphamide, doxorubicin and oral prednisone (BR-CAP) for 6, three week treatment cycles as shown in Table 3. Bortezomib for injection is administered first followed by rituximab. Bortezomib for injection is administered twice weekly for two weeks (Days 1, 4, 8, and 11) followed by a ten day rest period on Days 12 to 21. For patients with a response first documented at Cycle 6, two additional BR-CAP cycles are recommended. At least 72 hours should elapse between consecutive doses of bortezomib for injection. Table 3: Dosage Regimen for Patients with Previously Untreated Mantle Cell Lymphoma
Twice Weekly Bortezomib for Injection (6, Three Week Cycles)* 
Week
1
2
3
Bortezomib for Injection (1.3mg/m 2)
Day 1 
--
-- 
Day 4 
--
Day 8  
Day 11 
rest period 
Rituximab (375 mg/m 2) Cyclophosphamide (750 mg/m 2) Doxorubicin (50 mg/m 2)
Day 1
--
--
 
 
-- 
--
rest period 
Prednisone (100 mg/m 2)
Day 1 
Day 2
Day 3
Day 4
Day 5
 --
 --
 rest period
* Dosing may continue for two more cycles (for a total of eight cycles) if response is first seen at Cycle 6.
2.5Dose Modification Guidelines for Bortezomib for Injection When Given in Combination with Rituximab, Cyclophosphamide, Doxorubicin and Prednisone
Prior to the first day of each cycle (other than Cycle 1):
- Platelet count should be at least 100 x 10 9/L and absolute neutrophil count (ANC) should be at least 1.5 x 10 9/L
- Hemoglobin should be at least 8 g/dL (at least 4.96 mmol/L)
- Nonhematologic toxicity should have recovered to Grade 1 or baseline
Interrupt bortezomib for injection treatment at the onset of any Grade 3 hematologic or nonhematological toxicities, excluding neuropathy [see Table 5, Warnings and Precautions (5)]. For dose adjustments, see Table 4 below. Table 4: Dose Modifications on Days 4, 8, and 11 During Cycles of Combination Bortezomib for Injection, Rituximab, Cyclophosphamide, Doxorubicin and Prednisone Therapy
Toxicity  
Dose Modification or Delay  
Hematological Toxicity
 
- Grade 3 or higher neutropenia, or a platelet count not at or above 25 × 10 9/L 
Withhold bortezomib for injection therapy for up to 2 weeks until the patient has an ANC at or above 0.75 √ó 10 9/L and a platelet count at or above 25 √ó 10 9/L.
- If, after bortezomib for injection has been withheld, the toxicity does not resolve, discontinue bortezomib for injection.
- If toxicity resolves such that the patient has an ANC at or above 0.75 × 10 9/L and a platelet count at or above 25 × 10 9/L, bortezomib for injection dose should be reduced by 1 dose level (from 1.3 mg/m 2 to 1 mg/m 2, or from 1 mg/m 2 to 0.7 mg/m 2). 
Grade 3 or higher nonhematological toxicities
Withhold bortezomib for injection therapy until symptoms of the toxicity have resolved to Grade 2 or better. Then, bortezomib for injection may be reinitiated with one dose level reduction (from 1.3 mg/m 2 to 1 mg/m 2, or from 1 mg/m 2 to 0.7 mg/m 2). For bortezomib for injection-related neuropathic pain and/or peripheral neuropathy, hold or modify bortezomib for injection as outlined in Table 5.
For information concerning rituximab, cyclophosphamide, doxorubicin and prednisone, see manufacturer's prescribing information.
2.6 Dosage and Dose Modifications for Relapsed Multiple Myeloma and Relapsed Mantle Cell Lymphoma
Bortezomib for injection (1.3 mg/m 2/dose) is administered twice weekly for two weeks (Days 1, 4, 8, and 11) followed by a ten day rest period (Days 12 to 21). For extended therapy of more than eight cycles, bortezomib for injection may be administered on the standard schedule or, for relapsed multiple myeloma, on a maintenance schedule of once weekly for four weeks (Days 1, 8, 15, and 22) followed by a 13 day rest period (Days 23 to 35) [ see Clinical Studies (14)]. At least 72 hours should elapse between consecutive doses of bortezomib for injection. Patients with multiple myeloma who have previously responded to treatment with bortezomib for injection (either alone or in combination) and who have relapsed at least six months after their prior bortezomib for injection therapy may be started on bortezomib for injection at the last tolerated dose. Retreated patients are administered bortezomib for injection twice weekly (Days 1, 4, 8, and 11) every three weeks for a maximum of eight cycles. At least 72 hours should elapse between consecutive doses of bortezomib for injection. Bortezomib for injection may be administered either as a single agent or in combination with dexamethasone [ see Clinical Studies (14.1)].
Bortezomib for injection therapy should be withheld at the onset of any Grade 3 nonhematological or Grade 4 hematological toxicities excluding neuropathy as discussed below [see Warnings and Precautions (5)]. Once the symptoms of the toxicity have resolved, bortezomib for injection therapy may be reinitiated at a 25% reduced dose (1.3 mg/m 2/dose reduced to 1 mg/m 2/dose; 1 mg/m 2/dose reduced to 0.7 mg/m 2/dose).
For dose modifications guidelines for peripheral neuropathy, see section 2.7.
2.7Dose Modifications for Peripheral Neuropathy
Starting bortezomib for injection subcutaneously may be considered for patients with pre-existing or at high risk of peripheral neuropathy. Patients with pre-existing severe neuropathy should be treated with bortezomib for injection only after careful risk-benefit assessment. Patients experiencing new or worsening peripheral neuropathy during bortezomib for injection therapy may require a decrease in the dose and/or a less dose-intense schedule. For dose or schedule modification guidelines for patients who experience bortezomib for injection-related neuropathic pain and/or peripheral neuropathy, see Table 5.
Table 5: Recommended Dose Modification for Bortezomib for Injection-Related Neuropathic Pain and/or Peripheral Sensory or Motor Neuropathy
Severity of Peripheral Neuropathy Signs and Symptoms*
Modification of Dose and Regimen
Grade 1 (asymptomatic; loss of deep tendon reflexes or paresthesia) without pain or loss of function
No action
Grade 1 with pain or Grade 2 (moderate symptoms; limiting instrumental Activities of Daily Living (ADL) †)
Reduce bortezomib for injection to 1 mg/m 2
Grade 2 with pain or Grade 3 (severe symptoms; limiting self care ADL ‡)
Withhold bortezomib for injection therapy until toxicity resolves. When toxicity resolves reinitiate with a reduced dose of bortezomib for injection at 0.7 mg/m 2 once per week.
Grade 4 (life-threatening consequences; urgent intervention indicated)
Discontinue bortezomib for injection
*Grading based on NCI Common Terminology Criteria CTCAE v4.0
†Instrumental ADL: refers to preparing meals, shopping for groceries or clothes, using telephone, managing money, etc.
‡Self care ADL: refers to bathing, dressing and undressing, feeding self, using the toilet, taking medications, and not bedridden
2.8Dosage in Patients with Hepatic Impairment
Do not adjust the starting dose for patients with mild hepatic impairment. Start patients with moderate or severe hepatic impairment at a reduced dose of 0.7 mg/m 2 per injection during the first cycle, and consider subsequent dose escalation to 1 mg/m 2 or further dose reduction to 0.5 mg/m 2 based on patient tolerance (see Table 6) [ see Use in Specific Populations (8.7),
Clinical Pharmacology (12.3)].
Table 6: Recommended Starting Dose Modification for Bortezomib for Injection in Patients with Hepatic Impairment
 
Bilirubin Level
SGOT (AST) Levels
Modification of Starting Dose
Mild
Less than or equal to 1 x ULN
             More than ULN
None
More than 1x to 1.5x ULN
Any
None
Moderate
More than 1.5x to 3x ULN
Any
Reduce bortezomib for injection to 0.7 mg/m 2 in the first cycle. Consider dose escalation to1 mg/m 2 or further dose reduction to 0.5 mg/m 2 in subsequent cycles based on patient tolerability.
Severe
More than 3x ULN
Any
Abbreviations: SGOT = serum glutamic oxaloacetic transaminase; AST = aspartate aminotransferase;  ULN = upper limit of the normal range.
2.9 Administration Precautions
The drug quantity contained in one vial (3.5 mg) may exceed the usual dose required. Caution should be used in calculating the dose to prevent overdose [see Dosage and Administration (2.10)].
When administered subcutaneously, sites for each injection (thigh or abdomen) should be rotated. New injections should be given at least one inch from an old site and never into areas where the site is tender, bruised, erythematous, or indurated.
If local injection site reactions occur following bortezomib for injection administration subcutaneously, a less concentrated bortezomib for injection solution (1 mg/mL instead of 2.5 mg/mL) may be administered subcutaneously [ see Dosage and Administration (2.10)] . Alternatively, consider use of the intravenous route of administration [ see Dosage and Administration (2.10)]. Bortezomib for injection is a hazardous drug. Follow applicable special handling and disposal procedures. 1
2.10Reconstitution/Preparation for Intravenous and Subcutaneous Administration
Use proper aseptic technique. Reconstitute only with 0.9% sodium chloride. The reconstituted product should be a clear and colorless solution. Different volumes of 0.9% sodium chloride are used to reconstitute the product for the different routes of administration. The reconstituted concentration of bortezomib for subcutaneous administration (2.5 mg/mL) is greater than the reconstituted concentration of bortezomib for intravenous administration (1 mg/mL). Because each route of administration has a different reconstituted concentration, use caution when calculating the volume to be administered [ see Dosage and Administration (2.9)]. For each 3.5 mg single-dose vial of bortezomib, reconstitute with the following volume of 0.9% sodium chloride based on route of administration (Table 7):
Table 7: Reconstitution Volumes and Final Concentration for Intravenous and Subcutaneous Administration
Route of Administration
Bortezomib (mg/vial)
Diluent (0.9% Sodium Chloride)
Final Bortezomib Concentration (mg/mL)
Intravenous
3.5 mg
3.5 mL
1 mg/mL
Subcutaneous
3.5 mg
1.4 mL
2.5 mg/mL
Dose must be individualized to prevent overdosage. After determining patient body surface area (BSA) in square meters, use the following equations to calculate the total volume (mL) of reconstituted bortezomib for injection to be administered:
- Intravenous Administration [1 mg/mL concentration]
Bortezomib for injection dose (mg/m 2) x patient BSA (m 2)
    ______________________________________________   = Total bortezomib for injection volume (mL) to be administered
               1 mg/mL
- Subcutaneous Administration [2.5 mg/mL concentration]
Bortezomib for injection dose (mg/m 2) x patient BSA (m 2)
________________________________________________ = Total bortezomib for injection volume (mL) to be administered
                   2.5 mg/mL
Stickers that indicate the route of administration are provided with each bortezomib for injection vial.¬† These stickers should be placed directly on the syringe of bortezomib for injection once bortezomib for injection is prepared to help alert practitioners of the correct route of administration for bortezomib for injection. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit. If any discoloration or particulate matter is observed, the reconstituted product should not be used. Stability Unopened vials of bortezomib for injection are stable until the date indicated on the package when stored in the original package protected from light. Bortezomib for injection contains no antimicrobial preservative. Administer reconstituted bortezomib for injection within¬† eight hours of preparation.¬† When reconstituted as directed, bortezomib for injection may be stored at 25¬ļC (77¬ļF). The reconstituted material may be stored in the original vial and/or the syringe prior to administration. The product may be stored for up to¬† eight hours in a syringe; however, total storage time for the reconstituted material must not exceed¬† eight hours when exposed to normal indoor lighting.
3 Dosage Forms And Strengths
For injection: Each single-dose vial of bortezomib for injection contains 3.5 mg of bortezomib as a sterile white to off white lyophilized cake or powder for reconstitution and withdrawal of the appropriate individual patient dose [ see Dosage and Administration (2.10)].
For injection: Single-dose vial contains 3.5 mg of bortezomib as lyophilized powder for reconstitution and withdrawal of the appropriate individual patient dose.(3 )
4 Contraindications
Bortezomib is contraindicated in patients with hypersensitivity (not including local reactions) to bortezomib, boron, or mannitol. Reactions have included anaphylactic reactions [see Adverse Reactions (6.1) ].
Bortezomib is contraindicated for intrathecal administration. Fatal events have occurred with intrathecal administration of bortezomib.
- Patients with hypersensitivity (not including local reactions) to bortezomib, boron, or mannitol, including anaphylactic reactions. (
4 )- Contraindicated for intrathecal administration. (
4 )
5 Warnings And Precautions
- Peripheral Neuropathy: Manage with dose modification or discontinuation. ( Error! Hyperlink reference not valid.) Patients with pre-existing severe neuropathy should be treated with bortezomib only after careful risk-benefit assessment. ( Error! Hyperlink reference not valid.,
5.1 )- Hypotension: Use caution when treating patients taking anti‚ÄĎhypertensives, with a history of syncope, or with dehydration. (
5.2 )- Cardiac Toxicity: Worsening of and development of cardiac failure has occurred. Closely monitor patients with existing heart disease or risk factors for heart disease. (
5.3 )- Pulmonary Toxicity: Acute respiratory syndromes have occurred. Monitor closely for new or worsening symptoms and consider interrupting bortezomib therapy. (
5.4 )- Posterior Reversible Encephalopathy Syndrome: Consider MRI imaging for onset of visual or neurological symptoms; discontinue bortezomib if suspected. (
5.5 )- Gastrointestinal Toxicity: Nausea, diarrhea, constipation, and vomiting may require use of antiemetic and antidiarrheal medications or fluid replacement.
(5.6 )- Thrombocytopenia or Neutropenia: Monitor complete blood counts regularly throughout treatment. (
5.7 )- Tumor Lysis Syndrome: Closely monitor patients with high tumor burden. (
5.8 )- Hepatic Toxicity: Monitor hepatic enzymes during treatment. Interrupt bortezomib therapy to assess reversibility. (
5.9 )- Thrombotic Microangiopathy: Monitor for signs and symptoms. Discontinue bortezomib if suspected. (
5.10 )- Embryo-Fetal Toxicity: Bortezomib can cause fetal harm. Advise females of reproductive potential and males with female partners of reproductive potential of the potential risk to a fetus and to use effective contraception. (
5.11 )5.1 Peripheral Neuropathy
Bortezomib treatment causes a peripheral neuropathy that is predominantly sensory; however, cases of severe sensory and motor peripheral neuropathy have been reported. Patients with pre-existing symptoms (numbness, pain or a burning feeling in the feet or hands) and/or signs of peripheral neuropathy may experience worsening peripheral neuropathy (including ‚Č•Grade 3) during treatment with bortezomib. Patients should be monitored for symptoms of neuropathy, such as a burning sensation, hyperesthesia, hypoesthesia, paresthesia, discomfort, neuropathic pain or weakness. In the Phase 3 relapsed multiple myeloma trial comparing bortezomib subcutaneous vs intravenous, the incidence of Grade ‚Č•2 peripheral neuropathy was 24% for subcutaneous and 39% for intravenous. Grade ‚Č•3 peripheral neuropathy occurred in 6% of patients in the subcutaneous treatment group, compared with 15% in the intravenous treatment group [see Adverse Reactions (6.1)]. Starting bortezomib subcutaneously may be considered for patients with pre-existing or at high risk of peripheral neuropathy.
Patients experiencing new or worsening peripheral neuropathy during bortezomib therapy may require a decrease in the dose and/or a less dose-intense schedule [see Dosage and Administration (2.7)]. In the bortezomib vs dexamethasone Phase 3 relapsed multiple myeloma study, improvement in or resolution of peripheral neuropathy was reported in 48% of patients with¬†‚Č•Grade 2 peripheral neuropathy following dose adjustment or interruption. Improvement in or resolution of peripheral neuropathy was reported in 73% of patients who discontinued due to Grade 2 neuropathy or who had ‚Č•Grade 3 peripheral neuropathy in the Phase 2 multiple myeloma studies.¬†The long-term outcome of peripheral neuropathy has not been studied in mantle cell lymphoma.
5.2 Hypotension
The incidence of hypotension (postural, orthostatic, and hypotension NOS) was 8% [see Adverse Reactions (6.1)]. These events are observed throughout therapy. Patients with a history of syncope, patients receiving medications known to be associated with hypotension, and patients who are dehydrated may be at increased risk of hypotension. Management of orthostatic/postural hypotension may include adjustment of antihypertensive medications, hydration, and administration of mineralocorticoids and/or sympathomimetics.
5.3 Cardiac Toxicity
Acute development or exacerbation of congestive heart failure and new onset of decreased left ventricular ejection fraction have occurred during bortezomib therapy, including reports in patients with no risk factors for decreased left ventricular ejection fraction [see Adverse Reactions (6.1)]. Patients with risk factors for, or existing heart disease should be frequently monitored. In the relapsed multiple myeloma study of bortezomib vs dexamethasone, the incidence of any treatment-related cardiac disorder was 8% and 5% in the bortezomib and dexamethasone groups, respectively. The incidence of adverse reactions suggestive of heart failure (acute pulmonary edema, pulmonary edema, cardiac failure, congestive cardiac failure, cardiogenic shock) was ‚ȧ 1% for each individual reaction in the bortezomib group. In the dexamethasone group the incidence was ‚ȧ1% for cardiac failure and congestive cardiac failure; there were no reported reactions of acute pulmonary edema, pulmonary edema, or cardiogenic shock. There have been isolated cases of QT-interval prolongation in clinical studies; causality has not been established.
5.4 Pulmonary Toxicity
Acute Respiratory Distress Syndrome (ARDS) and acute diffuse infiltrative pulmonary disease of unknown etiology such as pneumonitis, interstitial pneumonia, lung infiltration have occurred in patients receiving bortezomib.  Some of these events have been fatal.
In a clinical trial, the first two patients given high-dose cytarabine (2g/m 2 per day) by continuous infusion with daunorubicin and bortezomib for relapsed acute myelogenous leukemia died of ARDS early in the course of therapy.
There have been reports of pulmonary hypertension associated with bortezomib administration in the absence of left heart failure or significant pulmonary disease.
In the event of new or worsening cardiopulmonary symptoms, consider interrupting bortezomib until a prompt and comprehensive diagnostic evaluation is conducted.
5.5 Posterior Reversible Encephalopathy Syndrome (PRES)
Posterior Reversible Encephalopathy Syndrome (PRES; formerly termed Reversible Posterior Leukoencephalopathy Syndrome (RPLS)) has occurred in patients receiving bortezomib. PRES is a rare, reversible, neurological disorder which can present with seizure, hypertension, headache, lethargy, confusion, blindness, and other visual and neurological disturbances. Brain imaging, preferably MRI (Magnetic Resonance Imaging), is used to confirm the diagnosis. In patients developing PRES, discontinue bortezomib. The safety of reinitiating bortezomib therapy in patients previously experiencing PRES is not known.
5.6 Gastrointestinal Toxicity
Bortezomib treatment can cause nausea, diarrhea, constipation, and vomiting [see Adverse Reactions (6.1)] sometimes requiring use of antiemetic and antidiarrheal medications. Ileus can occur. Fluid and electrolyte replacement should be administered to prevent dehydration. Interrupt bortezomib for severe symptoms.
5.7 Thrombocytopenia/Neutropenia
¬†Bortezomib is associated with thrombocytopenia and neutropenia that follow a cyclical pattern with¬†nadirs occurring following the last dose of each cycle and typically recovering prior to initiation of the¬†subsequent cycle. The cyclical pattern of platelet and neutrophil decreases and recovery remain consistent in the studies¬†of multiple myeloma and mantle cell lymphoma, with no evidence of cumulative thrombocytopenia or¬†neutropenia in the treatment regimens¬†studied. ¬†Monitor complete blood counts (CBC) frequently during treatment with bortezomib. Measure platelet¬†counts prior to each dose of bortezomib. Adjust dose/schedule for thrombocytopenia [see Dosage and Administration (2.6)]. Gastrointestinal and intracerebral hemorrhage has occurred¬†during thrombocytopenia in association with bortezomib. Support with transfusions and supportive care, according¬†to published¬†guidelines. In the single agent, relapsed multiple myeloma study of bortezomib vs dexamethasone, the mean¬†platelet count nadir measured was approximately 40% of baseline. The severity of thrombocytopenia related¬†to pretreatment platelet count is shown in Table 8. The incidence of bleeding (‚Č•Grade 3) was 2% on¬†the bortezomib arm and was <1% in the dexamethasone¬†arm.
Table 8: Severity of Thrombocytopenia Related to Pretreatment Platelet Count in the  Relapsed Multiple Myeloma Study of Bortezomib vs Dexamethasone  
Pretreatment Platelet Count*
Number of Patients (N=331) ‡
Number (%) of Patients with Platelet Count <10,000/¬ĶL
Number (%) of Patients with Platelet Count 10,000 to 25,000/¬ĶL¬†
‚Č• 75,000/¬ĶL
309
8 (3%)
36 (12%)
‚Č• 50,000/¬ĶL to <75,000/ ¬ĶL
14
2 (14%)
11 (79%)
‚Č• 10,000/¬ĶL to <50,000/ ¬ĶL
7
1 (14%)
5 (71%)
* A baseline platelet count of 50,000/¬ĶL was required for study¬†eligibility
‡Data were missing at baseline for one patient
In the combination study of bortezomib with rituximab, cyclophosphamide, doxorubicin and prednisone (BR-CAP) in previously untreated mantle cell lymphoma patients, the incidence of thrombocytopenia (‚Č•Grade 4) was 32% vs 1% for the rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) arm as shown in Table 12. The incidence of bleeding events (‚Č•Grade 3) was 1.7% in the BR-CAP arm (four patients) and was 1.2% in the R-CHOP arm (three patients). Platelet transfusions were given to 23% of the patients in the BR-CAP arm and 3% of the patients in the R-CHOP arm. The incidence of neutropenia (‚Č•Grade 4) was 70% in the BR-CAP arm and was 52% in the R-CHOP arm. The incidence of febrile neutropenia (‚Č•Grade 4) was 5% in the BR-CAP arm and was 6% in the R-CHOP arm. Myeloid growth factor support was provided at a rate of 78% in the BR-CAP arm and 61% in the R-CHOP arm.
5.8 Tumor Lysis Syndrome
Tumor lysis syndrome has been reported with bortezomib therapy. Patients at risk of tumor lysis syndrome are those with high tumor burden prior to treatment.  Monitor patients closely and take appropriate precautions.
5.9 Hepatic Toxicity
Cases of acute liver failure have been reported in patients receiving multiple concomitant medications and with serious underlying medical conditions. Other reported hepatic reactions include hepatitis, increases in liver enzymes, and hyperbilirubinemia. Interrupt bortezomib therapy to assess reversibility. There is limited rechallenge information in these patients.
5.10 Thrombotic Microangiopathy
Cases, sometimes fatal, of thrombotic microangiopathy, including thrombotic thrombocytopenic purpura/hemolytic uremic syndrome (TTP/HUS), have been reported in the postmarketing setting in patients who received bortezomib. Monitor for signs and symptoms of TTP/HUS. If the diagnosis is suspected, stop bortezomib  and evaluate. If the diagnosis of TTP/HUS is excluded, consider restarting bortezomib. The safety of reinitiating bortezomib therapy in patients previously experiencing TTP/HUS is not known.
5.11 Embryo-Fetal Toxicity
Based on the mechanism of action and findings in animals, bortezomib can cause fetal harm when administered to a pregnant woman. Bortezomib administered to rabbits during organogenesis at a dose approximately 0.5 times the clinical dose of 1.3 mg/m 2 based on body surface area caused postimplantation loss and a decreased number of live fetuses [ see Use in Specific Populations (8.1)]. Advise females of reproductive potential to use effective contraception during treatment with bortezomib and for  seven months following treatment. Advise males with female partners of reproductive potential to use effective contraception during treatment with bortezomib and for four months following treatment. If bortezomib is used during pregnancy or if the patient becomes pregnant during bortezomib treatment, the patient should be apprised of the potential risk to the fetus [ see Use in Specific Populations (8.1,  8.3), Nonclinical Toxicology (13.1)].
6 Adverse Reactions
The following clinically significant adverse reactions are also discussed in other sections of the labeling:
- Peripheral Neuropathy [see Warnings and Precautions (5.1)]
- Hypotension [see Warnings and Precautions (5.2)]
- Cardiac Toxicity [see Warnings and Precautions (5.3)]
- Pulmonary Toxicity [see Warnings and Precautions (5.4)]
- Posterior Reversible Encephalopathy Syndrome (PRES) [see Warnings and Precautions (5.5)]
- Gastrointestinal Toxicity [see Warnings and Precautions (5.6)]
- Thrombocytopenia/Neutropenia [see Warnings and Precautions (5.7)]
- Tumor Lysis Syndrome [see Warnings and Precautions (5.8)]
- Hepatic Toxicity [see Warnings and Precautions (5.9)]
- Thrombotic Microangiopathy [ see Warnings and Precautions (5.10)]
Most commonly reported adverse reactions (incidence ‚Č• 20%) in clinical studies include nausea, diarrhea, thrombocytopenia, neutropenia, peripheral neuropathy, fatigue, neuralgia, anemia, leukopenia, constipation, vomiting, lymphopenia, rash, pyrexia, and anorexia.(6.1 )
To report SUSPECTED ADVERSE REACTIONS, contact Novadoz Pharmaceuticals LLC at 1-855-668-2369 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice. Summary of Clinical Trial in Patients with Previously Untreated Multiple Myeloma Table 9 describes safety data from 340 patients with previously untreated multiple myeloma who received bortezomib (1.3 mg/m 2) administered intravenously in combination with melphalan  (9 mg/m 2) and prednisone (60 mg/m 2) in a prospective randomized study. The safety profile of bortezomib in combination with melphalan/prednisone is consistent with the known safety profiles of both bortezomib and melphalan/prednisone.
Table 9: Most Commonly Reported Adverse Reactions (‚Č• 10% in the Bortezomib, Melphalan and Prednisone Arm) with Grades 3 and ‚Č• 4 Intensity in the Previously Untreated Multiple Myeloma Study
 
Bortezomib, Melphalan and Prednisone  
Melphalan and Prednisone  
 
(n=340)
(n=337)
  Body System 
Total
Toxicity  Grade , n (%)
Total
Toxicity Grade , n (%)
Adverse Reaction
n (%)
3
‚Č•4
n (%)
3
‚Č•4
Blood and Lymphatic System Disorders  
Thrombocytopenia
164 (48)
60 (18)
57 (17)
140 (42)
48 (14)
39 (12)
Neutropenia
160 (47)
101 (30)
33 (10)
143 (42)
77 (23)
42 (12)
Anemia
109 (32)
41 (12)
4 (1)
156 (46)
61 (18)
18 (5)
Leukopenia
108 (32)
64 (19)
8 (2)
93 (28)
53 (16)
11 (3)
Lymphopenia
78 (23)
46 (14)
17 (5)
51 (15)
26 (8)
7 (2)
Gastrointestinal Disorders  
Nausea
134 (39)
10 (3)
0
70 (21)
1 (< 1)
0
Diarrhea
119 (35)
19 (6)
2 (1)
20 (6)
1 (< 1)
0
Vomiting
87 (26)
13 (4)
0
41 (12)
2 (1)
0
Constipation
77 (23)
2 (1)
0
14 (4)
0
0
Abdominal pain upper
34 (10)
1 (< 1)
0
20 (6)
0
0
Nervous System Disorders  
Peripheral neuropathy*
156 (46)
42 (12)
2 (1)
4 (1)
0
0
Neuralgia
117 (34)
27 (8)
2 (1)
1 (< 1)
0
0
Paresthesia
42 (12)
6 (2)
0
4 (1)
0
0
General Disorders and Administration Site Conditions  
Fatigue
85 (25)
19 (6)
2 (1)
48 (14)
4 (1)
0
Asthenia
54 (16)
18 (5)
0
23 (7)
3 (1)
0
Pyrexia
53 (16)
4 (1)
0
19 (6)
1 (< 1)
1 (< 1)
Infections and Infestations  
Herpes Zoster
39 (11)
11 (3)
0
9 (3)
4 (1)
0
Metabolism and Nutrition Disorders  
Anorexia
64 (19)
6 (2)
0
19 (6)
0
0
Skin and Subcutaneous Tissue Disorders  
Rash
38 (11)
2 (1)
0
7 (2)
0
0
Psychiatric Disorders  
Insomnia
35 (10)
1 (< 1)
0
21 (6)
0
0
  * Represents High Level Term Peripheral Neuropathies NEC
Relapsed Multiple Myeloma Randomized Study of Bortezomib vs Dexamethasone¬† The safety data described below and in Table 10 reflect exposure to either bortezomib (n=331) or dexamethasone (n=332) in a study of patients with relapsed multiple myeloma. Bortezomib was administered intravenously at doses of 1.3 mg/m 2 twice weekly for¬† two out of three weeks (21 day cycle). After eight, 21 day cycles patients continued therapy for three, 35 day cycles on a weekly schedule. Duration of treatment was up to 11 cycles ( nine months) with a median duration of¬† six cycles (4.1 months). For inclusion in the trial, patients must have had measurable disease and one to¬† three prior therapies. There was no upper age limit for entry. Creatinine clearance could be as low as 20 mL/min and bilirubin levels as high as 1.5 times the upper limit of normal. The overall frequency of adverse reactions was similar in men and women, and in patients <65 and ‚Č•65 years of age. Most patients were Caucasian [see Clinical Studies (14.1)]. Among the 331 bortezomib-treated patients, the most commonly reported (>20%) adverse reactions overall were nausea (52%), diarrhea (52%), fatigue (39%), peripheral neuropathies (35%), thrombocytopenia (33%), constipation (30%), vomiting (29%), and anorexia (21%). The most commonly reported (>20%) adverse reaction reported among the 332 patients in the dexamethasone group was fatigue (25%). Eight percent (8%) of patients in the bortezomib-treated arm experienced a Grade 4 adverse reaction; the most common reactions were thrombocytopenia (4%) and neutropenia (2%). Nine percent (9%) of dexamethasone-treated patients experienced a Grade 4 adverse reaction. All individual dexamethasone-related Grade 4 adverse reactions were less than 1%. Serious Adverse Reactions and Adverse Reactions Leading to Treatment Discontinuation in the Relapsed Multiple Myeloma Study of Bortezomib vs Dexamethasone Serious adverse reactions are defined as any reaction that results in death, is life-threatening, requires hospitalization or prolongs a current hospitalization, results in a significant disability, or is deemed to be an important medical event. A total of 80 (24%) patients from the bortezomib treatment arm experienced a serious adverse reaction during the study, as did 83 (25%) dexamethasone-treated patients. The most commonly reported serious adverse reactions in the bortezomib treatment arm were diarrhea (3%), dehydration, herpes zoster, pyrexia, nausea, vomiting, dyspnea, and thrombocytopenia (2% each). In the dexamethasone treatment group, the most commonly reported serious adverse reactions were pneumonia (4%), hyperglycemia (3%), pyrexia, and psychotic disorder (2% each). A total of 145 patients, including 84 (25%) of 331 patients in the bortezomib treatment group and 61 (18%) of 332 patients in the dexamethasone treatment group were discontinued from treatment due to adverse reactions. Among the 331 bortezomib-treated patients, the most commonly reported adverse reaction leading to discontinuation was peripheral neuropathy (8%). Among the 332 patients in the dexamethasone group, the most commonly reported adverse reactions leading to treatment discontinuation were psychotic disorder and hyperglycemia (2% each). Four deaths were considered to be bortezomib-related in this relapsed multiple myeloma study:¬†one case each of cardiogenic shock, respiratory insufficiency, congestive heart failure and cardiac arrest. Four deaths were considered dexamethasone-related:¬†two cases of sepsis,¬†one case of bacterial meningitis, and¬†one case of sudden death at home. Most Commonly Reported Adverse Reactions in the Relapsed Multiple Myeloma Study of Bortezomib vs Dexamethasone The most common adverse reactions from the relapsed multiple myeloma study are shown in Table 10. All adverse reactions with incidence ‚Č• 10% in the bortezomib arm are included.
Table 10: Most Commonly Reported Adverse Reactions (‚Č• 10% in Bortezomib Arm), with Grades 3 and 4 Intensity in the Relapsed Multiple Myeloma Study of Bortezomib¬† vs Dexamethasone N=663)
 
Bortezomib (N=331)
Dexamethasone (N=332)
Adverse Reactions
All
Grade 3
Grade 4
All
Grade 3
Grade 4
Any Adverse Reactions
324 (98)
193 (58)
28 (8)
297 (89)
110 (33)
29 (9)
Nausea
172 (52)
8 (2)
0
31 (9)
0
0
Diarrhea NOS
171 (52)
22 (7)
0
36 (11)
2 (< 1)
0
Fatigue
130 (39)
15 (5)
0
82 (25)
8 (2)
0
Peripheral neuropathies *
115 (35)
23 (7)
2 (< 1)
14 (4)
0
1 (< 1)
Thrombocytopenia
109 (33)
80 (24)
12 (4)
11 (3)
5 (2)
1 (< 1)
Constipation
99 (30)
6 (2)
0
27 (8)
1 (< 1)
0
Vomiting NOS
96 (29)
8 (2)
0
10 (3)
1 (< 1)
0
Anorexia
68 (21)
8 (2)
0
8 (2)
1 (< 1)
0
Pyrexia
66 (20)
2 (< 1)
0
21 (6)
3 (< 1)
1 (< 1)
Paresthesia
64 (19)
5 (2)
0
24 (7)
0
0
Anemia NOS
63 (19)
20 (6)
1 (< 1)
21 (6)
8 (2)
0
Headache NOS
62 (19)
3 (< 1)
0
23 (7)
1 (< 1)
0
Neutropenia
58 (18)
37 (11)
8 (2)
1 (< 1)
1 (< 1)
0
Rash NOS
43 (13)
3 (< 1)
0
7 (2)
0
0
Appetite decreased NOS
36 (11)
0
0
12 (4)
0
0
Dyspnea NOS
35 (11)
11 (3)
1 (< 1)
37 (11)
7 (2)
1 (< 1)
Abdominal pain NOS
35 (11)
5 (2)
0
7 (2)
0
0
Weakness
34 (10)
10 (3)
0
28 (8)
8 (2)
0
* Represents High Level Term Peripheral Neuropathies NEC
Safety Experience from the Phase 2 Open-Label Extension Study in Relapsed Multiple Myeloma In the Phase 2 extension study of 63 patients, no new cumulative or new long-term toxicities were observed with prolonged bortezomib treatment. These patients were treated for a total of 5.3 to 23 months, including time on bortezomib in the prior bortezomib study [see Clinical Studies (14.1)]. Safety Experience from the Phase 3 Open-Label Study of Bortezomib Subcutaneous vs Intravenous in Relapsed Multiple Myeloma The safety and efficacy of bortezomib administered subcutaneously were evaluated in one Phase 3 study at the recommended dose of 1.3 mg/m 2. This was a randomized, comparative study of bortezomib subcutaneous vs intravenous in 222 patients with relapsed multiple myeloma. The safety data described below and in Table 11 reflect exposure to either bortezomib subcutaneous (N=147) or bortezomib intravenous (N=74) [ see Clinical Studies (14.1)]. Table 11: Most Commonly Reported Adverse Reactions (‚Č• 10%), with Grade 3 and ‚Č• 4 Intensity in the Relapsed Multiple Myeloma Study (N=221) of Bortezomib Subcutaneous¬† vs Intravenous
Subcutaneous
Intravenous
(N=147)
(N=74)
 Body System  
Total    
Toxicity Grade ,  n (%)  
Total  
Toxicity Grade ,  n (%)  
Adverse Reaction
n (%)
3
‚Č•4
n (%)
3
‚Č•4
Blood and Lymphatic System Disorders
Anemia
28 (19)
8 (5)
0
17 (23)
3 (4)
0
Leukopenia
26 (18)
8 (5)
0
15 (20)
4 (5)
1 (1)
Neutropenia
34 (23)
15 (10)
4 (3)
20 (27)
10 (14)
3 (4)
Thrombocytopenia
44 (30)
7 (5)
5 (3)
25 (34)
7 (9)
5 (7)
Gastrointestinal Disorders
Diarrhea
28 (19)
1 (1)
0
21 (28)
3 (4)
0
Nausea
24 (16)
0
0
10 (14)
0
0
Vomiting
13 (9)
3 (2)
0
8 (11)
0
0
General Disorders and Administration Site Conditions
Asthenia
10 (7)
1 (1)
0
12 (16)
4 (5)
0
Fatigue
11 (7)
3 (2)
0
11 (15)
3 (4)
0
Pyrexia
18 (12)
0
0
6 (8)
0
0
Nervous System Disorders
Neuralgia
34 (23)
5 (3)
0
17 (23)
7 (9)
0
Peripheral neuropathies *
55 (37)
8 (5)
1 (1)
37 (50)
10 (14)
1 (1)
Note: Safety population: 147 patients in the subcutaneous treatment group and 74 patients in the intravenous treatment group who received at least one dose of study medication *Represents High Level Term Peripheral Neuropathies NEC
In general, safety data were similar for the subcutaneous and intravenous treatment groups. Differences were observed in the rates of some Grade ‚Č•3 adverse reactions. Differences of ‚Č•5% were reported in neuralgia (3% subcutaneous¬† vs 9% intravenous), peripheral neuropathies (6% subcutaneous vs 15% intravenous), neutropenia (13% subcutaneous vs 18% intravenous), and thrombocytopenia (8% subcutaneous vs 16% intravenous). A local reaction was reported in 6% of patients in the subcutaneous group, mostly redness. Only¬† two (1%) patients were reported as having severe reactions,¬† one case of pruritus and¬† one case of redness. Local reactions led to reduction in injection concentration in one patient and drug discontinuation in one patient. Local reactions resolved in a median of six days. Dose reductions occurred due to adverse reactions in 31% of patients in the subcutaneous treatment group compared with 43% of the intravenously-treated patients. The most common adverse reactions leading to a dose reduction included peripheral sensory neuropathy (17% in the subcutaneous treatment group compared with 31% in the intravenous treatment group); and neuralgia (11% in the subcutaneous treatment group compared with 19% in the intravenous treatment group). Serious Adverse Reactions and Adverse Reactions Leading to Treatment Discontinuation in the Relapsed Multiple Myeloma Study of Bortezomib Subcutaneous vs Intravenous The incidence of serious adverse reactions was similar for the subcutaneous treatment group (20%) and the intravenous treatment group (19%). The most commonly reported serious adverse reactions in the subcutaneous treatment arm were pneumonia and pyrexia (2% each). In the intravenous treatment group, the most commonly reported serious adverse reactions were pneumonia, diarrhea, and peripheral sensory neuropathy (3% each). In the subcutaneous treatment group, 27 patients (18%) discontinued study treatment due to an adverse reaction compared with 17 patients (23%) in the intravenous treatment group. Among the 147 subcutaneously-treated patients, the most commonly reported adverse reactions leading to discontinuation were peripheral sensory neuropathy (5%) and neuralgia (5%). Among the 74 patients in the intravenous treatment group, the most commonly reported adverse reactions leading to treatment discontinuation were peripheral sensory neuropathy (9%) and neuralgia (9%). Two patients (1%) in the subcutaneous treatment group and¬†one (1%) patient in the intravenous treatment group died due to an adverse reaction during treatment. In the subcutaneous group the causes of death were one case of pneumonia and one case of sudden death. In the intravenous group the cause of death was coronary artery insufficiency.
Safety Experience from the Clinical Trial in Patients with Previously Untreated Mantle Cell Lymphoma 
Table 12 describes safety data from 240 patients with previously untreated mantle cell lymphoma who received bortezomib (1.3 mg/m 2) administered intravenously in combination with rituximab (375 mg/m 2), cyclophosphamide (750 mg/m 2), doxorubicin (50 mg/m 2), and prednisone (100 mg/m 2) (BR-CAP) in a prospective randomized study.
Infections were reported for 31% of patients in the BR-CAP arm and 23% of the patients in the comparator (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone [R-CHOP]) arm, including the predominant preferred term of pneumonia (BR-CAP 8% vs R-CHOP 5%).
Table 12: Most Commonly Reported Adverse Reactions (‚Č•5%) with Grades 3 and ‚Č•4 Intensity in¬†the¬†Previously Untreated Mantle Cell Lymphoma¬†Study
                                                                                                                                                                                                                                                                                     
    
  BR-CAP   (n=240)  
  R-CHOP   (n=242)  
  Body System   Adverse Reactions  
  All   n (%)  
  Toxicity   Grade 3 n (%)  
¬† Toxicity ¬† Grade ‚Č•4 n (%) ¬†
  All   n (%)     
  Toxicity   Grade 3 n (%)  
¬† Toxicity ¬† Grade ‚Č•4 n (%) ¬†
  Blood and Lymphatic System Disorders  
 Neutropenia  
 209 (87)  
 32 (13)  
 168 (70)  
 172 (71)  
 31 (13)  
 125 (52)  
 Leukopenia  
 116 (48)  
 34 (14)  
 69 (29)  
 87 (36)  
 39 (16)  
 27 (11)  
 Anemia  
 106 (44)  
 27 (11)  
 4 (2)  
 71 (29)  
 23 (10)  
 4 (2)  
 Thrombocytopenia  
 172 (72)  
 59 (25)  
 76 (32)  
 42 (17)  
 9 (4)  
 3 (1)  
 Febrile neutropenia  
 41 (17)  
 24 (10)  
 12 (5)  
 33 (14)  
 17 (7)  
 15 (6)  
 Lymphopenia  
 68 (28)  
 25 (10)  
 36 (15)  
 28 (12)  
 15 (6)  
 2 (1)  
  Nervous System Disorders  
 Peripheral neuropathy*  
 71 (30)  
 17 (7)  
 1 (< 1)  
 65 (27)  
 10 (4)  
 0  
 Hypoesthesia  
 14 (6)  
 3 (1)  
 0  
 13 (5)  
 0  
 0  
 Paresthesia  
 14 (6)  
 2 (1)  
 0  
 11 (5)  
 0  
 0  
 Neuralgia  
 25 (10)  
 9 (4)  
 0  
 1 (< 1)  
 0  
 0  
  General Disorders and Administration Site Conditions  
 Fatigue  
 43 (18)  
 11 (5)  
 1 (< 1)  
 38 (16)  
 5 (2)  
 0  
 Pyrexia  
 48 (20)  
 7 (3)  
 0  
 23 (10)  
 5 (2)  
 0  
 Asthenia  
 29 (12)  
 4 (2)  
 1 (< 1)  
 18 (7)  
 1 (< 1)  
 0  
 Edema peripheral  
 16 (7)  
 1 (< 1)  
 0  
 13 (5)  
 0  
 0  
  Gastrointestinal Disorders  
 Nausea  
 54 (23)  
 1 (< 1)  
 0  
 28 (12)  
 0  
 0  
 Constipation  
 42 (18)  
 1 (< 1)  
 0  
 22 (9)  
 2 (1)  
 0  
 Stomatitis  
 20 (8)  
 2 (1)  
 0  
 19 (8)  
 0  
 1 (< 1)  
 Diarrhea  
 59 (25)  
 11 (5)  
 0  
 11 (5)  
 3 (1)  
 1 (< 1)  
 Vomiting  
 24 (10)  
 1 (< 1)  
 0  
 8 (3)  
 0  
 0  
 Abdominal distension  
 13 (5)  
 0  
 0  
 4 (2)  
 0  
 0  
  Infections and Infestations  
 Pneumonia  
 20 (8)  
 8 (3)  
 5 (2)  
 11 (5)  
 5 (2)  
 3 (1)  
  Skin and Subcutaneous Tissue Disorders  
 Alopecia  
 31 (13)  
 1 (< 1)  
 1 (< 1)  
 33 (14)  
 4 (2)  
 0  
  Metabolism and Nutrition Disorders  
 Hyperglycemia  
 10 (4)  
 1 (< 1)  
 0  
 17 (7)  
 10 (4)  
 0  
 Decreased appetite  
 36 (15)  
 2 (1)  
 0  
 15 (6)  
 1 (< 1)  
 0  
  Vascular Disorders  
 Hypertension  
 15 (6)  
 1 (< 1)  
 0  
 3 (1)  
 0  
 0  
  Psychiatric Disorders  
 Insomnia  
 16 (7)  
 1 (< 1)  
 0  
 8 (3)  
 0  
 0  
Key: R-CHOP = rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone; BR-CAP = bortezomib, rituximab, cyclophosphamide, doxorubicin, and prednisone.
* Represents High Level Term Peripheral Neuropathies NEC
The incidence of herpes zoster reactivation was 4.6% in the BR-CAP arm and 0.8% in the R-CHOP arm. Antiviral prophylaxis was mandated by protocol amendment.
The incidences of Grade ‚Č•3 bleeding events were similar between the two arms (four patients in¬†the BR-CAP arm and three patients in the R-CHOP arm). All of the Grade ‚Č•3 bleeding events ¬†resolved without sequelae in the BR-CAP¬†arm.
Adverse reactions leading to discontinuation occurred in 8% of patients in BR-CAP group and 6% of patients in R-CHOP group. In the BR-CAP group, the most commonly reported adverse reaction leading to discontinuation was peripheral sensory neuropathy (1%; three patients). The most commonly reported adverse reaction leading to discontinuation in the R-CHOP group was febrile neutropenia (<1%; two patients).
Integrated Summary of Safety (Relapsed Multiple Myeloma and Relapsed Mantle Cell Lymphoma) Safety data from Phase 2 and 3 studies of single agent bortezomib 1.3 mg/m 2/dose twice weekly¬† for¬†two weeks followed by a¬† ten day rest period in 1163 patients with previously-treated multiple¬†¬† myeloma (N=1008) and previously-treated mantle cell lymphoma (N=155) were integrated and tabulated. This analysis does not include data from the Phase 3 open-label study of bortezomib subcutaneous¬† vs intravenous in relapsed multiple myeloma. In the integrated studies, the safety profile of bortezomib was similar in patients with multiple myeloma and mantle cell lymphoma. In the integrated analysis, the most commonly reported (>20%) adverse reactions were nausea (49%), diarrhea (46%), asthenic conditions including fatigue (41%) and weakness (11%), peripheral neuropathies (38%), thrombocytopenia (32%), vomiting (28%), constipation (25%), and pyrexia (21%). Eleven percent (11%) of patients experienced at least¬† one episode of ‚Č•Grade 4 toxicity, most commonly thrombocytopenia (4%) and neutropenia (2%). In the Phase 2 relapsed multiple myeloma clinical trials of bortezomib administered intravenously, local skin irritation was reported in 5% of patients, but extravasation of bortezomib was not associated with tissue damage. Serious Adverse Reactions and Adverse Reactions Leading to Treatment Discontinuation in the Integrated Summary of Safety A total of 26% of patients experienced a serious adverse reaction during the studies. The most commonly reported serious adverse reactions included diarrhea, vomiting and pyrexia (3% each), nausea, dehydration, and thrombocytopenia (2% each) and pneumonia, dyspnea, peripheral neuropathies, and herpes zoster (1% each). Adverse reactions leading to discontinuation occurred in 22% of patients. The reasons for discontinuation included peripheral neuropathy (8%), and fatigue, thrombocytopenia, and diarrhea (2% each). In total, 2% of the patients died and the cause of death was considered by the investigator to be possibly related to study drug: including reports of cardiac arrest, congestive heart failure, respiratory failure, renal failure, pneumonia and sepsis. Most Commonly Reported Adverse Reactions in the Integrated Summary of Safety The most common adverse reactions are shown in Table 13. All adverse reactions occurring at ‚Č•10% are included. In the absence of a randomized comparator arm, it is often not possible to distinguish between adverse events that are drug-caused and those that reflect the patient‚Äôs underlying disease. Please see the discussion of specific adverse reactions that follows.
Table 13: ¬†¬†Most Commonly Reported (‚Č•10% Overall) Adverse Reactions in Integrated Analyses of Relapsed Multiple Myeloma and Relapsed Mantle Cell Lymphoma Studies Using the 1.3 mg/m 2 Dose (N=1163)
 
All Patients (N=1163)
Multiple Myeloma (N=1008)
Mantle Cell Lymphoma (N=155)
Adverse Reactions 
All
‚Č•Grade 3
All 
‚Č•Grade 3
All 
‚Č•Grade 3
Nausea
567 (49)
36 (3)
511 (51)
32 (3)
56 (36)
4 (3)
Diarrhea NOS
530 (46)
83 (7)
470 (47)
72 (7)
60 (39)
11 (7)
Fatigue
477 (41)
86 (7)
396 (39)
71 (7)
81 (52)
15 (10)
Peripheral neuropathies *
443 (38)
129 (11)
359 (36)
110 (11)
84 (54)
19 (12)
Thrombocytopenia
369 (32)
295 (25)
344 (34)
283 (28)
25 (16)
12 (8)
Vomiting NOS
321 (28)
44 (4)
286 (28)
40 (4)
35 (23)
4 (3)
Constipation
296 (25)
17 (1)
244 (24)
14 (1)
52 (34)
3 (2)
Pyrexia
249 (21)
16 (1)
233 (23)
15 (1)
16 (10)
1 (< 1)
Anorexia
227 (20)
19 (2)
205 (20)
16 (2)
22 (14)
3 (2)
Anemia NOS
209 (18)
65 (6)
190 (19)
63 (6)
19 (12)
2 (1)
Headache NOS
175 (15)
8 (< 1)
160 (16)
8 (< 1)
15 (10)
0
Neutropenia
172 (15)
121 (10)
164 (16)
117 (12)
8 (5)
4 (3)
Rash NOS
156 (13)
8 (< 1)
120 (12)
4 (< 1)
36 (23)
4 (3)
Paresthesia
147 (13)
9 (< 1)
136 (13)
8 (< 1)
11 (7)
1 (< 1)
Dizziness (excl vertigo)
129 (11)
13 (1)
101 (10)
9 (< 1)
28 (18)
4 (3)
Weakness
124 (11)
31 (3)
106 (11)
28 (3)
18 (12)
3 (2)
  *Represents High Level Term Peripheral Neuropathies NEC
Description of Selected Adverse Reactions from the Integrated Phase 2 and 3 Relapsed Multiple Myeloma and Phase 2 Relapsed Mantle Cell Lymphoma Studies Gastrointestinal Toxicity A total of 75% of patients experienced at least one gastrointestinal disorder. The most common gastrointestinal disorders included nausea, diarrhea, constipation, vomiting, and appetite decreased. Other gastrointestinal disorders included dyspepsia and dysgeusia. Grade 3 adverse reactions occurred in 14% of patients; ‚Č•Grade 4 adverse reactions were ‚ȧ1%. Gastrointestinal adverse reactions were considered serious in 7% of patients. Four percent (4%) of patients discontinued due to a gastrointestinal adverse reaction. Nausea was reported more often in patients with multiple myeloma (51%) compared to patients with mantle cell lymphoma (36%). Thrombocytopenia Across the studies, bortezomib-associated thrombocytopenia was characterized by a decrease in platelet count during the dosing period (Days 1 to 11) and a return toward baseline during the ten day rest period during each treatment cycle. Overall, thrombocytopenia was reported in 32% of patients. Thrombocytopenia was Grade 3 in 22%, ‚Č•Grade 4 in 4%, and serious in 2% of patients, and the reaction resulted in bortezomib discontinuation in 2% of patients [ see Warnings and Precautions (5.7)]. Thrombocytopenia was reported more often in patients with multiple myeloma (34%) compared to patients with mantle cell lymphoma (16%). The incidence of ‚Č•Grade 3 thrombocytopenia also was higher in patients with multiple myeloma (28%) compared to patients with mantle cell lymphoma (8%). Peripheral Neuropathy Overall, peripheral neuropathies occurred in 38% of patients. Peripheral neuropathy was Grade 3 for 11% of patients and ‚Č•Grade 4 for <1% of patients. Eight percent (8%) of patients discontinued bortezomib due to peripheral neuropathy. The incidence of peripheral neuropathy was higher among patients with mantle cell lymphoma (54%) compared to patients with multiple myeloma (36%). In the bortezomib vs dexamethasone Phase 3 relapsed multiple myeloma study, among the 62 bortezomib-treated patients who experienced ‚Č•Grade 2 peripheral neuropathy and had dose adjustments, 48% had improved or resolved with a median of 3.8 months from first onset. In the Phase 2 relapsed multiple myeloma studies, among the 30 patients who experienced Grade 2 peripheral neuropathy resulting in discontinuation or who experienced ‚Č•Grade 3 peripheral neuropathy, 73% reported improvement or resolution with a median time of 47 days to improvement of one grade or more from the last dose of bortezomib. Hypotension The incidence of hypotension (postural, orthostatic and hypotension NOS) was 8% in patients treated with bortezomib. Hypotension was Grade 1 or 2 in the majority of patients and Grade 3 in 2% and ‚Č•Grade 4 in <1%. Two percent (2%) of patients had hypotension reported as a serious adverse reaction, and 1% discontinued due to hypotension. The incidence of hypotension was similar in patients with multiple myeloma (8%) and those with mantle cell lymphoma (9%). In addition, <1% of patients experienced hypotension associated with a syncopal reaction. Neutropenia Neutrophil counts decreased during the bortezomib dosing period (Days 1 to 11) and returned toward baseline during the tenday rest period during each treatment cycle. Overall, neutropenia occurred in 15% of patients and was Grade 3 in 8% of patients and ‚Č•Grade 4 in 2%. Neutropenia was reported as a serious adverse reaction in <1% of patients and < 1% of patients discontinued due to neutropenia. The incidence of neutropenia was higher in patients with multiple myeloma (16%) compared to patients with mantle cell lymphoma (5%). The incidence of ‚Č•Grade 3 neutropenia also was higher in patients with multiple myeloma (12%) compared to patients with mantle cell lymphoma (3%). Asthenic Conditions (Fatigue, Malaise, Weakness, Asthenia) Asthenic conditions were reported in 54% of patients. Fatigue was reported as Grade 3 in 7% and ‚Č•Grade 4 in <1% of patients. Asthenia was reported as Grade 3 in 2% and ‚Č•Grade 4 in <1% of patients. Two percent (2%) of patients discontinued treatment due to fatigue and <1% due to weakness and asthenia. Asthenic conditions were reported in 53% of patients with multiple myeloma and 59% of patients with mantle cell lymphoma. Pyrexia Pyrexia (> 38¬ļC) was reported as an adverse reaction for 21% of patients. The reaction was Grade 3 in 1% and ‚Č•Grade 4 in <1%. Pyrexia was reported as a serious adverse reaction in 3% of patients and led to bortezomib discontinuation in <1% of patients. The incidence of pyrexia was higher among patients with multiple myeloma (23%) compared to patients with mantle cell lymphoma (10%). The incidence of ‚Č•Grade 3 pyrexia was 1% in patients with multiple myeloma and < 1% in patients with mantle cell lymphoma. Herpes Virus Infection Consider using antiviral prophylaxis in subjects being treated with bortezomib. In the randomized studies in previously untreated and relapsed multiple myeloma, herpes zoster reactivation was more common in subjects treated with bortezomib (ranging between 6 to11%) than in the control groups (3 to 4%). Herpes simplex was seen in 1 to 3% in subjects treated with bortezomib and 1 to 3% in the control groups. In the previously untreated multiple myeloma study, herpes zoster virus reactivation in the bortezomib, melphalan and prednisone arm was less common in subjects receiving prophylactic antiviral therapy (3%) than in subjects who did not receive prophylactic antiviral therapy (17%). Retreatment in Relapsed Multiple Myeloma A single-arm trial was conducted in 130 patients with relapsed multiple myeloma to determine the efficacy and safety of retreatment with intravenous bortezomib. The safety profile of patients in this trial is consistent with the known safety profile of bortezomib -treated patients with relapsed multiple myeloma as demonstrated in Tables 10, 11, and 13; no cumulative toxicities were observed upon retreatment. The most common adverse drug reaction was thrombocytopenia which occurred in 52% of the patients. The incidence of ‚Č•Grade 3 thrombocytopenia was 24%.¬† Peripheral neuropathy occurred in 28% of patients, with the incidence of ‚Č•Grade 3 peripheral neuropathy reported at 6%. The incidence of serious adverse reactions was 12.3%. The most commonly reported serious adverse reactions were thrombocytopenia (3.8%), diarrhea (2.3%), and herpes zoster and pneumonia (1.5% each). Adverse reactions leading to discontinuation occurred in 13% of patients. The reasons for discontinuation included peripheral neuropathy (5%) and diarrhea (3%). Two deaths considered to be bortezomib-related occurred within 30 days of the last bortezomib dose; one in a patient with cerebrovascular accident and one in a patient with sepsis. Additional Adverse Reactions from Clinical Studies The following clinically important serious adverse reactions that are not described above have been reported in clinical trials in patients treated with bortezomib administered as monotherapy or in combination with other chemotherapeutics. These studies were conducted in patients with hematological malignancies and in solid tumors. Blood and Lymphatic System Disorders: Anemia, disseminated intravascular coagulation, febrile neutropenia, lymphopenia, leukopenia Cardiac Disorders: Angina pectoris, atrial fibrillation aggravated, atrial flutter, bradycardia, sinus arrest, cardiac amyloidosis, complete atrioventricular block, myocardial ischemia, myocardial infarction, pericarditis, pericardial effusion, Torsades de pointes, ventricular tachycardia Ear and Labyrinth Disorders: Hearing impaired, vertigo Eye Disorders: Diplopia and blurred vision, conjunctival infection, irritation Gastrointestinal Disorders: Abdominal pain, ascites, dysphagia, fecal impaction, gastroenteritis, gastritis hemorrhagic, hematemesis, hemorrhagic duodenitis, ileus paralytic, large intestinal obstruction, paralytic intestinal obstruction, peritonitis, small intestinal obstruction, large intestinal perforation, stomatitis, melena, pancreatitis acute, oral mucosal petechiae, gastroesophageal reflux General Disorders and Administration Site Conditions: Chills, edema, edema peripheral, injection site erythema, neuralgia, injection site pain, irritation, malaise, phlebitis Hepatobiliary Disorders: Cholestasis, hepatic hemorrhage, hyperbilirubinemia, portal vein thrombosis, hepatitis, liver failure Immune System Disorders: Anaphylactic reaction, drug hypersensitivity, immune complex mediated hypersensitivity, angioedema, laryngeal edema Infections and Infestations: Aspergillosis, bacteremia, bronchitis, urinary tract infection, herpes viral infection, uleriosis, nasopharyngitis, pneumonia, respiratory tract infection, septic shock, toxoplasmosis, oral candidiasis, sinusitis, catheter-related infection Injury, Poisoning and Procedural Complications: Catheter-related complication, skeletal fracture, subdural hematoma Investigations: Weight decreased Metabolism and Nutrition Disorders: Dehydration, hypocalcemia, hyperuricemia, hypokalemia, hyperkalemia, hyponatremia, hypernatremia Musculoskeletal and Connective Tissue Disorders: Arthralgia, back pain, bone pain, myalgia, pain in extremity Nervous System Disorders: Ataxia, coma, dizziness, dysarthria, dysesthesia, dysautonomia, encephalopathy, cranial palsy, grand mal convulsion, headache, hemorrhagic stroke, motor dysfunction, neuralgia, spinal cord compression, paralysis, postherpetic neuralgia, transient ischemic attack Psychiatric Disorders: Agitation, anxiety, confusion, insomnia, mental status change, psychotic disorder, suicidal ideation Renal and Urinary Disorders: Calculus renal, bilateral hydronephrosis, bladder spasm, hematuria, hemorrhagic cystitis, urinary incontinence, urinary retention, renal failure (acute and chronic), glomerular nephritis proliferative Respiratory, Thoracic and Mediastinal Disorders: Acute respiratory distress syndrome, aspiration pneumonia, atelectasis, chronic obstructive airways disease exacerbated, cough, dysphagia, dyspnea, dyspnea exertional, epistaxis, hemoptysis, hypoxia, lung infiltration, pleural effusion, pneumonitis, respiratory distress, pulmonary hypertension Skin and Subcutaneous Tissue Disorders: Urticaria, face edema, rash (which may be pruritic), leukocytoclastic vasculitis, pruritus Vascular Disorders: Cerebrovascular accident, cerebral hemorrhage, deep venous thrombosis, hypertension, peripheral embolism, pulmonary embolism, pulmonary hypertension
6.2 Postmarketing Experience
The following adverse reactions have been identified from the worldwide postmarketing experience with bortezomib. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure: Cardiac Disorders: Cardiac tamponade Ear and Labyrinth Disorders: Deafness bilateral Eye Disorders: Optic neuropathy, blindness, chalazion/blepharitis Gastrointestinal Disorders: Ischemic colitis Infections and Infestations: Progressive multifocal leukoencephalopathy (PML), ophthalmic herpes, herpes meningoencephalitis Nervous System Disorders: Posterior reversible encephalopathy syndrome (PRES, formerly RPLS), Guillain-Barré syndrome, demyelinating polyneuropathy   Respiratory, Thoracic and Mediastinal Disorders: Acute diffuse infiltrative pulmonary disease Skin and Subcutaneous Tissue Disorders: Stevens-Johnson syndrome/toxic epidermal necrolysis (SJS/TEN), acute febrile neutrophilic dermatosis (Sweet’s syndrome)
7 Drug Interactions
- Strong CYP3A4 Inhibitors: Closely monitor patients with concomitant use. (
7.1 )- Strong CYP3A4 Inducers: Avoid concomitant use. (7.3)
7.1 Effects of Other Drugs on Bortezomib
Strong CYP3A4 Inducers Coadministration with a strong CYP3A4 inducer decreases the exposure of bortezomib [see Clinical Pharmacology (12.3)]  which may decrease bortezomib efficacy. Avoid coadministration with strong CYP3A4 inducers. Strong CYP3A4 Inhibitors Coadministration with a strong CYP3A4 inhibitor increases the exposure of bortezomib [ see Clinical Pharmacology (12.3)] which may increase the risk of bortezomib toxicities. Monitor patients for signs of bortezomib toxicity and consider a bortezomib dose reduction if bortezomib must be given in combination with strong CYP3A4 inhibitors.
7.2 Drugs Without Clinically Significant Interactions with Bortezomib
No clinically significant drug interactions have been observed when bortezomib was coadministered with dexamethasone, omeprazole, or melphalan in combination with prednisone [ see Clinical Pharmacology (12.3)].
8 Use In Specific Populations
Patients with diabetes may require close monitoring of blood glucose and adjustment of antidiabetic medication.(8.8 )
8.1 Pregnancy
Risk Summary Based on its mechanism of action [see Clinical Pharmacology (12.1)]  and findings in animals, bortezomib can cause fetal harm when administered to a pregnant woman. There are no studies with the use of bortezomib in pregnant women to inform drug-associated risks. Bortezomib caused embryo-fetal lethality in rabbits at doses lower than the clinical dose (see Data). Advise pregnant women of the potential risk to the fetus. Adverse outcomes in pregnancy occur regardless of the health of the mother or the use of medications. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively. Data Animal Data Bortezomib was not teratogenic in nonclinical developmental toxicity studies in rats and rabbits at the highest dose tested (0.075 mg/kg; 0.5 mg/m 2 in the rat and 0.05 mg/kg; 0.6 mg/m 2 in the rabbit) when administered during organogenesis. These dosages are approximately 0.5 times the clinical dose of 1.3 mg/m 2 based on body surface area. Bortezomib caused embryo-fetal lethality in rabbits at doses lower than the clinical dose (approximately 0.5 times the clinical dose of 1.3 mg/m 2 based on body surface area). Pregnant rabbits given bortezomib during organogenesis at a dose of 0.05 mg/kg (0.6 mg/m 2) experienced significant postimplantation loss and decreased number of live fetuses. Live fetuses from these litters also showed significant decreases in fetal weight.
8.2 Lactation
Risk Summary There are no data on the presence of bortezomib or its metabolites in human milk, the effects of the drug on the breastfed child, or the effects of the drug on milk production. Because many drugs are excreted in human milk and because the potential for serious adverse reactions in breastfed child from bortezomib is unknown, advise nursing women not to breastfeed during treatment with bortezomib and for two months after treatment.
8.3 Females and Males of Reproductive Potential
Based on its mechanism of action and findings in animals, bortezomib can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)].   Pregnancy Testing Conduct pregnancy testing in females of reproductive potential prior to initiating bortezomib treatment. Contraception Females Advise females of reproductive potential to use effective contraception during treatment with bortezomib and for seven months after the last dose. Males Males with female partners of reproductive potential should use effective contraception during treatment with bortezomib and for four months after the last dose. Infertility Based on the mechanism of action and findings in animals, bortezomib may have an effect on either male or female fertility [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
Safety and effectiveness have not been established in pediatric patients. The activity and safety of bortezomib in combination with intensive reinduction chemotherapy was evaluated in pediatric and young adult patients with lymphoid malignancies (pre-B cell ALL 77%, 16% with T-cell ALL, and 7% T-cell lymphoblastic lymphoma (LL)), all of whom relapsed within 36 months of initial diagnosis in a single-arm multicenter, nonrandomized cooperative group trial. An effective reinduction multiagent chemotherapy regimen was administered in¬†three blocks. Block 1 included vincristine, prednisone, doxorubicin and pegaspargase; Block 2 included cyclophosphamide, etoposide and methotrexate; Block 3 included high-dose cytosine arabinoside and asparaginase. Bortezomib was administered at a dose of 1.3 mg/m 2 as a bolus intravenous injection on Days 1, 4, 8, and 11 of Block 1 and Days 1, 4, and 8 of Block 2. There were 140 patients with ALL or LL enrolled and evaluated for safety. The median age was ten years (range: 1 to 26), 57% were male, 70% were white, 14% were black, 4% were Asian, 2% were American Indian/Alaska Native, 1% were Pacific Islander. The activity was evaluated in a prespecified subset of the first 60 evaluable patients enrolled on the study with pre-B ALL ‚ȧ 21 years and relapsed <36 months from diagnosis. The complete remission (CR) rate at day 36 was compared to that in a historical control set of patients who had received the identical backbone therapy without bortezomib.¬† There was no evidence that the addition of bortezomib had any impact on the CR rate. No new safety concerns were observed when bortezomib was added to a chemotherapy backbone regimen as compared with a historical control group in which the backbone regimen was given without bortezomib. The BSA-normalized clearance of bortezomib in pediatric patients was similar to that observed in adults.
8.5 Geriatric Use
Of the 669 patients enrolled in the relapsed multiple myeloma study, 245 (37%) were 65 years of age or older: 125 (38%) on the bortezomib arm and 120 (36%) on the dexamethasone arm. Median time to progression and median duration of response for patients ‚Č•65 were longer on bortezomib compared to dexamethasone [5.5 mo vs 4.3 mo, and 8.0 mo¬† vs 4.9 mo, respectively]. On the bortezomib arm, 40% (n=46) of evaluable patients aged ‚Č•65 experienced response (CR + PR)¬† vs 18% (n=21) on the dexamethasone arm. The incidence of Grade 3 and 4 events was 64%, 78% and 75% for bortezomib patients ‚ȧ50, 51 to 64 and ‚Č•65 years old, respectively [see Adverse Reactions (6.1), Clinical Studies (14.1)].
No overall differences in safety or effectiveness were observed between patients ‚Č•age 65 and younger patients receiving bortezomib; but greater sensitivity of some older individuals cannot be ruled out.
8.6 Renal Impairment
 No starting dosage adjustment of bortezomib is recommended for patients with renal impairment. In patients requiring dialysis, bortezomib should be administered after the dialysis procedure [see Clinical Pharmacology (12.3)].
8.7Hepatic Impairment
No starting dosage adjustment of bortezomib is recommended for patients with mild hepatic impairment (total bilirubin ‚ȧ1x ULN and AST >ULN, or total bilirubin >1 to 1.5x ULN and any AST). The exposure of bortezomib is increased in patients with moderate (total bilirubin ‚Č•1.5 to 3x ULN and any AST) and severe (total bilirubin >3x ULN and any AST) hepatic impairment. Reduce the starting dose in patients with moderate or severe hepatic impairment [see Dosage and Administration (2.8), Clinical Pharmacology (12.3)].
8.8 Patients with Diabetes
During clinical trials, hypoglycemia and hyperglycemia were reported in diabetic patients receiving oral hypoglycemics. Patients on oral antidiabetic agents receiving bortezomib treatment may require close monitoring of their blood glucose levels and adjustment of the dose of their antidiabetic medication.
10 Overdosage
There is no known specific antidote for bortezomib overdosage. In humans, fatal outcomes following the administration of more than twice the recommended therapeutic dose have been reported, which were associated with the acute onset of symptomatic hypotension (5.2) and thrombocytopenia ( 5.7). In the event of an overdosage, the patient’s vital signs should be monitored and appropriate supportive care given.
Studies in monkeys and dogs showed that intravenous bortezomib doses as low as two times the recommended clinical dose on a mg/m 2 basis were associated with increases in heart rate, decreases in contractility, hypotension, and death. In dog studies, a slight increase in the corrected QT interval was observed at doses resulting in death. In monkeys, doses of 3.0 mg/m 2 and greater (approximately twice the recommended clinical dose) resulted in hypotension starting at one hour postadministration, with progression to death in 12 to 14 hours following drug administration.
11 Description
Bortezomib for Injection, a proteasome inhibitor, contains bortezomib which is an antineoplastic agent. Bortezomib is a modified dipeptidyl boronic acid. The chemical name for bortezomib, the monomeric boronic acid, is [(1R)-3-methyl-1-[[(2S)-1-oxo-3-phenyl-2-[(pyrazinylcarbonyl) amino]propyl]amino]butyl] boronic acid. Bortezomib has the following chemical structure: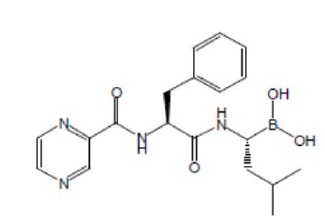
The molecular weight is 384.24. The molecular formula is C 19H 25BN 4O 4. The solubility of bortezomib, is freely soluble in N, N dimethyl fornamide, soluble in methanol and practically insoluble in n-Hexane.
Bortezomib is available for intravenous injection or subcutaneous use. Each single-dose vial contains 3.5 mg of bortezomib as a sterile lyophilized powder. It also contains the inactive ingredient: 35 mg mannitol, USP. The product is provided as a mannitol boronic ester which, in reconstituted form, consists of the mannitol ester in equilibrium with its hydrolysis product, the monomeric boronic acid. The drug substance exists in its cyclic anhydride form as a trimeric boroxine.
12 Clinical Pharmacology
12.1 Mechanism of Action
Bortezomib is a reversible inhibitor of the chymotrypsin-like activity of the 26S proteasome in mammalian cells. The 26S proteasome is a large protein complex that degrades ubiquitinated proteins. The ubiquitin-proteasome pathway plays an essential role in regulating the intracellular concentration of specific proteins, thereby maintaining homeostasis within cells. Inhibition of the 26S proteasome prevents this targeted proteolysis, which can affect multiple signaling cascades within the cell. This disruption of normal homeostatic mechanisms can lead to cell death. Experiments have demonstrated that bortezomib is cytotoxic to a variety of cancer cell types in vitro. Bortezomib causes a delay in tumor growth in vivo in nonclinical tumor models, including multiple myeloma.
12.2 Pharmacodynamics
Following twice weekly administration of 1 mg/m 2 and 1.3 mg/m 2 bortezomib doses, the maximum inhibition of 20S proteasome activity (relative to baseline) in whole blood was observed  five minutes after drug administration. Comparable maximum inhibition of 20S proteasome activity was observed between 1 and 1.3 mg/m 2 doses. Maximal inhibition ranged from 70% to 84% and from 73% to 83% for the 1 mg/m 2 and 1.3 mg/m 2 dose regimens, respectively.
12.3 Pharmacokinetics
Following intravenous administration of 1 mg/m 2 and 1.3 mg/m 2 doses, the mean maximum plasma concentrations of bortezomib (C max) after the first dose (Day 1) were 57 and 112 ng/mL, respectively. When administered twice weekly, the mean maximum observed plasma concentrations ranged from 67 to 106 ng/mL for the 1 mg/m 2 dose and 89 to 120 ng/mL for the 1.3 mg/m 2 dose. Following an intravenous bolus or subcutaneous injection of a 1.3 mg/m 2 dose to patients¬† with multiple myeloma, the total systemic exposure after repeat dose administration (AUC last) was equivalent for subcutaneous and intravenous administration. The AUC last geometric mean ratio (90% confidence interval) was 0.99 (0.80 to 1.23). The C max after subcutaneous administration (20.4 ng/mL) was lower than after intravenous administration (223 ng/mL) with repeat dose administration. Distribution The mean distribution volume of bortezomib ranged from approximately 498 to 1884 L/m 2 following single- or repeat-dose administration of 1 mg/m 2 or 1.3mg/m 2 to patients with multiple myeloma. The binding of bortezomib to human plasma proteins averaged 83% over the concentration range of 100 to 1,000 ng/mL. Elimination The mean elimination half-life of bortezomib upon multiple dosing ranged from 40 to 193 hours after the 1 mg/m 2 dose and 76 to 108 hours after the 1.3 mg/m 2 dose. The mean total body clearances were 102 and 112 L/h following the first dose for doses of 1 mg/m 2 and 1.3 mg/m 2, respectively, and¬† ranged from 15 to 32 L/h following subsequent doses for doses of 1 and 1.3 mg/m 2, respectively. Metabolism Bortezomib is primarily oxidatively metabolized to several inactive metabolites in vitro via cytochrome P450 (CYP) enzymes 3A4, CYP2C19, and CYP1A2, and to a lesser extent by CYP2D6 and CYP2C9. Excretion The pathways of elimination of bortezomib have not been characterized in humans. Specific Populations No clinically significant differences in the pharmacokinetics of bortezomib were observed based on age, sex, or renal impairment (including patients administered bortezomib after dialysis). The effect of race on bortezomib pharmacokinetics is unknown. Patients with Hepatic Impairment Following administration of bortezomib doses ranging from 0.5 to 1.3 mg/m 2, mild (total bilirubin ‚ȧ1x ULN and AST >ULN, or total bilirubin >1 to 1.5x ULN and any AST) hepatic impairment did not alter dose-normalized bortezomib AUC when compared to patients with normal hepatic function. Dose normalized mean bortezomib AUC increased by approximately 60% in patients with moderate (total bilirubin >1.5 to 3x ULN and any AST) or severe (total bilirubin >3x ULN and any AST) hepatic impairment. A lower starting dose is recommended in patients with moderate or severe hepatic impairment. Drug Interaction Studies Clinical Studies No clinically significant differences in bortezomib pharmacokinetics were observed when coadministered with dexamethasone (weak CYP3A4 inducer), omeprazole (strong CYP2C19 inhibitor), or melphalan in combination with prednisone. Strong CYP3A4 inhibitor Coadministration with ketoconazole (strong CYP3A4 inhibitor) increased bortezomib exposure by 35%.
Strong CYP3A4 inducer Coadministration with rifampin (strong CYP3A4 inducer) decreased bortezomib exposure by approximately 45%. In Vitro Studies Bortezomib may inhibit CYP2C19 activity and increase exposure to drugs that are substrates for this enzyme.
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis ,Impairment of Fertility
Carcinogenicity studies have not been conducted with bortezomib.
Bortezomib showed clastogenic activity (structural chromosomal aberrations) in the in vitro chromosomal aberration assay using Chinese hamster ovary cells. Bortezomib was not genotoxic when tested in the in vitro mutagenicity assay (Ames test) and in vivo micronucleus assay in mice.
Fertility studies with bortezomib were not performed but evaluation of reproductive tissues has been performed in the general toxicity studies. In the six month rat toxicity study, degenerative effects in the ovary were observed at doses ‚Č•0.3 mg/m 2 (one-fourth of the recommended clinical dose), and degenerative changes in the testes occurred at 1.2 mg/m 2.
13.2 Animal Toxicology and/or Pharmacology
Cardiovascular Toxicity Studies in monkeys showed that administration of dosages approximately twice the recommended clinical dose resulted in heart rate elevations, followed by profound progressive hypotension, bradycardia, and death 12 to 14 hours postdose. Doses ‚Č• 1.2 mg/m 2 induced dose-proportional changes in cardiac parameters. Bortezomib has been shown to distribute to most tissues in the body, including the myocardium. In a repeated dosing toxicity study in the monkey, myocardial hemorrhage, inflammation, and necrosis were also observed.
Chronic Administration
 In animal studies at a dose and schedule similar to that recommended for patients (twice weekly dosing for two weeks followed by one week rest), toxicities observed included severe anemia and thrombocytopenia, and gastrointestinal, neurological and lymphoid system toxicities. Neurotoxic effects of bortezomib in animal studies included axonal swelling and degeneration in peripheral nerves, dorsal spinal roots, and tracts of the spinal cord. Additionally, multifocal hemorrhage and necrosis in the brain, eye, and heart were observed.
14 Clinical Studies
14.1 Multiple Myeloma
Randomized, Open-Label Clinical Study in Patients with Previously Untreated Multiple Myeloma A prospective, international, randomized (1:1), open-label clinical study (NCT00111319) of 682 patients was conducted to determine whether bortezomib administered intravenously (1.3 mg/m 2) in combination with melphalan (9 mg/m 2) and prednisone (60 mg/m 2) resulted in improvement in time to progression (TTP) when compared to melphalan (9 mg/m 2) and prednisone (60 mg/m 2) in patients with previously untreated multiple myeloma. Treatment was administered for a maximum of  nine cycles (approximately 54 weeks) and was discontinued early for disease progression or unacceptable toxicity. Antiviral prophylaxis was recommended for patients on the bortezomib study arm.
The median age of the patients in the study was 71 years (48;91), 50% were male, 88% were Caucasian and the median Karnofsky performance status score for the patients was 80 (60;100). Patients had IgG/IgA/Light chain myeloma in 63%/25%/8% instances, a median hemoglobin of 105 g/L (64;165), and a median platelet count of 221,500/microliter (33,000; 587,000). Efficacy results for the trial are presented in Table 14. At a prespecified interim analysis (with median follow-up of 16.3 months), the combination of bortezomib, melphalan and prednisone therapy resulted in significantly superior results for time to progression, progression-free survival, overall survival and response rate. Further enrollment was halted, and patients receiving melphalan and prednisone were offered bortezomib in addition. A later, prespecified analysis of overall survival (with median follow-up of 36.7 months with a hazard ratio of 0.65, 95% CI: 0.51, 0.84) resulted in a statistically significant survival benefit for the bortezomib, melphalan and prednisone treatment arm despite subsequent therapies including bortezomib based regimens. In an updated analysis of overall survival based on 387 deaths (median follow-up 60.1 months), the median overall survival for the bortezomib, melphalan and prednisone treatment arm was 56.4 months and for the melphalan and prednisone treatment arm was 43.1 months, with a hazard ratio of 0.695 (95% CI: 0.57, 0.85).
Table 14: Summary of Efficacy Analyses in the Previously Untreated Multiple Myeloma Study
Efficacy Endpoint  
Bortezomib, Melphalan and Prednisone (n=344)
Melphalan and Prednisone (n=338)
Time to Progression
Events n (%)
101 (29)
152 (45)
Median* (months)
20.7
15.0
(95% CI)
(17.6, 24.7)
(14.1, 17.9)
Hazard ratio †
0.54
(95% CI)
(0.42, 0.70)
p-value ‡
0.000002
Progression-Free Survival
Events n (%)
135 (39)
190 (56)
Median * (months)
18.3
14.0
(95% CI)
(16.6, 21.7)
(11.1, 15.0)
Hazard ratio †
0.61
(95% CI)
(0.49, 0.76)
 p-value ‡
0.00001
Response Rate
CR § n (%)
102 (30)
12 (4)
PR § n (%)
136 (40)
103 (30)
nCR n (%)
5 (1)
0
CR + PR § n (%)
238 (69)
115 (34)
p-value ¶
<10 -10
Overall Survival at Median Follow Up of 36.7 Months
Events (deaths) n (%)
109 (32)
148 (44)
Median * (months)
Not Reached
43.1
(95% CI)
(46.2, NR)
(34.8, NR)
Hazard ratio †
0.65
(95% CI)
(0.51, 0.84)
p-value ‡
0.00084
Note: All results are based on the analysis performed at a median follow-up duration of 16.3 months except for the overall survival analysis. *Kaplan-Meier estimate ‚ĆHazard ratio estimate is based on a Cox proportional-hazard model adjusted for stratification factors: beta 2-microglobulin, albumin, and region. A hazard ratio less than¬† one indicates an advantage for bortezomib, melphalan and prednisone ‚Ä°p-value based on the stratified log-rank test adjusted for stratification factors: beta 2-microglobulin, albumin, and region ¬ß EBMT criteria ¬∂ p-value for Response Rate (CR + PR) from the Cochran-Mantel-Haenszel chi-square test adjusted for the stratification factors TTP was statistically significantly longer on the bortezomib, melphalan and prednisone arm (see Figure 1). (median follow-up 16.3 months) Figure 1: Time to Progression Bortezomib, Melphalan and Prednisone vs Melphalan and Prednisone Overall survival was statistically significantly longer on the bortezomib, melphalan and prednisone arm (see Figure 2). (median follow-up 60.1 months) Figure 2: Overall Survival Bortezomib, Melphalan and Prednisone vs Melphalan and Prednisone Randomized, Clinical Study in Relapsed Multiple Myeloma of Bortezomib vs Dexamethasone A prospective Phase 3, international, randomized (1:1), stratified, open-label clinical study (NCT00048230) enrolling 669 patients was designed to determine whether bortezomib resulted in improvement in time to progression (TTP) compared to high-dose dexamethasone in patients with progressive multiple myeloma following 1 to 3 prior therapies. Patients considered to be refractory to prior high-dose dexamethasone were excluded as were those with baseline Grade ‚Č•2 peripheral neuropathy or platelet counts < 50,000/őľL. A total of 627 patients were evaluable for response. Stratification factors were based on the number of lines of prior therapy the patient had previously received (one previous line vs more than one¬† line of therapy), time of progression relative to prior treatment (progression during or within¬† six¬† months of stopping their most recent therapy vs relapse > 6 months after receiving their most recent therapy), and screening beta 2-microglobulin levels¬† (‚ȧ ¬†¬†¬†¬†2.5 mg/L vs >2.5 mg/L). Baseline patient and disease characteristics are summarized in Table 15. Table 15: Summary of Baseline Patient and Disease Characteristics in the Relapsed Multiple Myeloma Study
Patient Characteristics
Bortezomib (N=333)
Dexamethasone  (N=336)
Median age in years (range)
62.0 (33, 84)
61.0 (27, 86)
Gender: Male/female
56% / 44%
60% / 40%
Race: Caucasian/black/other
90% / 6% / 4%
88% / 7% / 5%
Karnofsky performance status score ‚ȧ70
13%
17%
Hemoglobin <100 g/L
32%
28%
Platelet count <75 x 10 9/L
6%
4%
Disease Characteristics
Type of myeloma (%): IgG/IgA/Light chain
60% / 23% / 12%
59% / 24% / 13%
Median beta 2-microglobulin (mg/L)
3.7
3.6
Median albumin (g/L)
39.0
39.0
Creatinine clearance ‚ȧ30 mL/min [n (%)]
17 (5%)
11 (3%)
Median Duration of Multiple Myeloma Since Diagnosis (Years)
  3.5
  3.1
Number of Prior Therapeutic Lines of Treatment
Median
2
2
1 prior line
40%
35%
>1 prior line
60%
65%
Previous Therapy
Any prior steroids, e.g., dexamethasone, VAD
98%
99%
Any prior anthracyclines, e.g., VAD, mitoxantrone
77%
76%
Any prior alkylating agents, e.g., MP, VBMCP
91%
92%
Any prior thalidomide therapy
48%
50%
Vinca alkaloids
74%
72%
Prior stem cell transplant/other high-dose therapy
67%
68%
Prior experimental or other types of therapy
3%
2%
Patients in the bortezomib treatment group were to receive 8, three week treatment cycles followed by 3,¬† five week treatment cycles of bortezomib. Patients achieving a CR were treated for¬† four cycles beyond first evidence of CR. Within each three¬† week treatment cycle, bortezomib 1.3 mg/m 2/dose alone was administered by intravenous bolus twice weekly for two weeks on Days 1, 4, 8, and 11 followed by a ten day rest period (Days 12 to 21). Within each five week treatment cycle, bortezomib 1.3 mg/m 2/dose alone was administered by intravenous bolus once weekly for four weeks on Days 1, 8, 15, and 22 followed by a 13 day rest period (Days 23 to 35) [ see Dosage and Administration (2.2)]. Patients in the dexamethasone treatment group were to receive 4, five week treatment cycles followed by 5,¬† four¬† week treatment cycles. Within each five week treatment cycle, dexamethasone 40 mg/day PO was administered once daily on Days 1 to 4, 9 to 12, and 17 to 20 followed by a 15 day rest period (Days 21 to 35). Within each four week treatment cycle, dexamethasone 40 mg/day PO was administered once daily on Days 1 to 4 followed by a 24 day rest period (Days 5 to 28). Patients with documented progressive disease on dexamethasone were offered bortezomib at a standard dose and schedule on a companion study. Following a preplanned interim analysis of time to progression, the dexamethasone arm was halted and all patients randomized to dexamethasone were offered bortezomib, regardless of disease status. In the bortezomib arm, 34% of patients received at least one bortezomib dose in all¬† eight of the three week cycles of therapy, and 13% received at least one dose in all 11 cycles. The average number of bortezomib doses during the study was 22, with a range of 1 to 44. In the dexamethasone arm, 40% of patients received at least one dose in all¬† four of the five week treatment cycles of therapy, and 6% received at least one dose in all¬†¬† nine cycles. The time to event analyses and response rates from the relapsed multiple myeloma study are presented in Table 16. Response and progression were assessed using the European Group for Blood and Marrow Transplantation (EBMT) criteria. Complete response (CR) required <5% plasma cells in the marrow, 100% reduction in M-protein, and a negative immunofixation test (IF -). Partial response (PR) requires ‚Č•50% reduction in serum myeloma protein and ‚Č•90% reduction of urine myeloma protein on at least two occasions for a minimum of at least¬† six weeks along with stable bone disease and normal calcium. Near complete response (nCR) was defined as meeting all the criteria for complete response including 100% reduction in M-protein by protein electrophoresis; however, M-protein was still detectable by immunofixation (IF +). Table 16: Summary of Efficacy Analyses in the Relapsed Multiple Myeloma Study
Efficacy Endpoint
All Patients
1 Prior Line of Therapy
> 1 Prior Line of Therapy
Bortezomib
Dex
Bortezomib
Dex
Bortezomib
Dex
(n=333)
(n=336)
(n=132)
(n=119)
(n=200)
(n=217)
Time to Progression Events n (%)
147 (44)
196 (58)
55 (42)
64 (54)
92 (46)
132 (61)
Median * (95% CI)
    6.2 mo  (4.9, 6.9)
    3.5 mo (2.9, 4.2)
      7.0 mo (6.2, 8.8)
    5.6 mo (3.4, 6.3)
    4.9 mo (4.2, 6.3)
    2.9 mo (2.8, 3.5)
Hazard ratio †  (95% CI)
0.55 (0.44, 0.69)
0.55 (0.38, 0.81)
0.54 (0.41, 0.72)
p-value ‡
<0.0001
0.0019
<0.0001
Overall Survival  Events (deaths) n (%)
51 (15)
84 (25)
12 (9)
24 (20)
39 (20)
60 (28)
Hazard ratio † (95% CI)
0.57 (0.40, 0.81)
0.39 (0.19, 0.81)
0.65  (0.43, 0.97)
p-value ‡, §
<0.05
<0.05
<0.05
Response Rate Population ¶ n = 627
n=315
n=312
n=128
n=110
n=187
n=202
CR #n (%)
20 (6)
2 (<1)
8 (6)
2 (2)
12 (6)
0 (0)
PR #n(%)
101 (32)
54 (17)
49 (38)
27 (25)
52 (28)
27 (13)
nCR #, ♠  n(%)
21 (7)
3 (<1)
8 (6)
2 (2)
13 (7)
1 (<1)
CR + PR #n (%)
121 (38)
56 (18)
57 (45)
29 (26)
64 (34)
27 (13)
p-value ‚ô•
<0.0001
0.0035
<0.0001
* Kaplan-Meier estimate † Hazard ratio is based on Cox proportional-hazard model with the treatment as single independent variable. A hazard ratio less than one indicates an advantage for bortezomib ‡ p-value based on the stratified log-rank test including randomization stratification factors § Precise p-value cannot be rendered ¶ Response population includes patients who had measurable disease at baseline and received at least one  dose of study drug # EBMT criteria; nCR meets all EBMT criteria for CR but has positive IF. Under EBMT criteria nCR is in the PR category ♠ In two patients, the IF was unknown ♥ p-value for Response Rate (CR + PR) from the Cochran-Mantel-Haenszel chi-square test adjusted for the stratification factors TTP was statistically significantly longer on the bortezomib arm (see Figure 3). Figure 3: Time to Progression Bortezomib vs Dexamethasone (Relapsed Multiple Myeloma Study)
As shown in Figure 4, bortezomib had a significant survival advantage relative to dexamethasone (p < 0.05). The median follow-up was 8.3 months. Figure 4: Overall Survival Bortezomib vs Dexamethasone (Relapsed Multiple Myeloma Study)
For the 121 patients achieving a response (CR or PR) on the bortezomib arm, the median duration was 8.0 months (95% CI: 6.9, 11.5 months) compared to 5.6 months (95% CI: 4.8, 9.2 months) for the 56 responders on the dexamethasone arm. The response rate was significantly higher on the bortezomib arm regardless of beta 2-microglobulin levels at baseline. Randomized, Open-Label Clinical Study of Bortezomib Subcutaneous vs Intravenous in Relapsed Multiple Myeloma An open-label, randomized, Phase 3 noninferiority study (NCT00722566) compared the efficacy and safety of the subcutaneous administration of bortezomib vs the intravenous administration. This study included 222 bortezomib na√Įve patients with relapsed multiple myeloma, who were randomized in a 2:1 ratio to receive 1.3 mg/m 2 of bortezomib by either the subcutaneous (n=148) or intravenous (n=74) route for¬† eight cycles. Patients who did not obtain an optimal response (less than Complete Response (CR)) to therapy with bortezomib alone after four cycles were allowed to receive oral dexamethasone 20 mg daily on the day of and after bortezomib administration (82 patients in subcutaneous treatment group and 39 patients in the intravenous treatment group). Patients with baseline Grade ‚Č•2 peripheral neuropathy or neuropathic pain, or platelet counts <50,000/őľL were excluded. A total of 218 patients were evaluable for response. Stratification factors were based on the number of lines of prior therapy the patient had received ( one previous line vs¬† more than one¬† line of therapy), and international staging system (ISS) stage (incorporating beta 2-microglobulin and albumin levels; Stages I, II, or III). The baseline demographic and other characteristics of the two treatment groups are summarized as follows: the median age of the patient population was approximately 64 years of age (range: 38 to 88 years), primarily male (subcutaneous: 50%, intravenous: 64%); the primary type of myeloma is IgG (subcutaneous: 65% IgG, 26% IgA, 8% light chain; intravenous: 72% IgG, 19% IgA, 8% light chain), ISS staging I/II/III (%) was 27, 41, 32 for both subcutaneous and intravenous, Karnofsky performance status score was ‚ȧ70% in 22% of subcutaneous and 16% of intravenous, creatinine clearance was 67.5 mL/min in subcutaneous and 73 mL/min in intravenous, the median years from diagnosis was 2.68 and 2.93 in subcutaneous and intravenous respectively and the proportion of patients with more than one prior line of therapy was 38% in subcutaneous and 35% in intravenous. This study met its primary (noninferiority) objective that single agent subcutaneous bortezomib retains at least 60% of the overall response rate after four cycles relative to single agent intravenous bortezomib. The results are provided in Table 17. Table 17: Summary of Efficacy Analyses in the Relapsed Multiple Myeloma Study of Bortezomib Subcutaneous vs Intravenous
 
Subcutaneous Bortezomib
Intravenous Bortezomib
Intent to Treat Population
(n=148)
(n=74)
Primary Endpoint
Response Rate at 4 Cycles
ORR (CR + PR) n(%)
63 (43)
31 (42)
Ratio of Response Rates (95% CI)
1.01 (0.73, 1.40)
CR n (%)
11 (7)
6 (8)
PR n (%)
52 (35)
25 (34)
nCR n (%)
9 (6)
4 (5)
Secondary Endpoints
Response Rate at 8 Cycles
ORR (CR + PR)
78 (53)
38 (51)
CR n (%)
17 (11)
9 (12)
PR n (%)
61 (41)
29 (39)
nCR n (%)
14 (9)
7 (9)
Median Time to Progression, months
10.4
9.4
Median Progression-Free Survival, months
10.2
8.0
1 Year Overall Survival (%) *
72.6
76.7
*Median duration of follow-up is 11.8 months A Randomized, Phase 2 Dose-Response Study in Relapsed Multiple Myeloma An open-label, multicenter study randomized 54 patients with multiple myeloma who had progressed or relapsed on or after front-line therapy to receive bortezomib 1 mg/m 2 or 1.3 mg/m 2 intravenous bolus twice weekly for two¬† weeks on Days 1, 4, 8, and 11 followed by a ten day rest period (Days 12 to 21). The median duration of time between diagnosis of multiple myeloma and first dose of bortezomib on this trial was two years, and patients had received a median of¬† one prior line of treatment (median of three prior therapies). A single complete response was seen at each dose. The overall response rates (CR + PR) were 30% (8/27) at 1 mg/m 2 and 38% (10/26) at 1.3 mg/m 2. A Phase 2 Open-Label Extension Study in Relapsed Multiple Myeloma Patients from the two Phase 2 studies, who in the investigators‚Äô opinion would experience additional clinical benefit, continued to receive bortezomib beyond 8 cycles on an extension study. Sixty-three (63) patients from the Phase 2 multiple myeloma studies were enrolled and received a median of¬† seven additional cycles of bortezomib therapy for a total median of 14 cycles (range: 7 to 32). The overall median dosing intensity was the same in both the parent protocol and extension study. Sixty-seven percent (67%) of patients initiated the extension study at the same or higher dose intensity at which they completed the parent protocol, and 89% of patients maintained the standard three week dosing schedule during the extension study. No new cumulative or new long-term toxicities were observed with prolonged bortezomib treatment [ see Adverse Reactions (6.1)]. A Single-Arm Trial of Retreatment in Relapsed Multiple Myeloma A single-arm, open-label trial (NCT00431769) was conducted to determine the efficacy and safety of retreatment with bortezomib. One hundred and thirty patients (‚Č• 18 years of age) with multiple myeloma who previously had at least partial response on a bortezomib-containing regimen (median of two prior lines of therapy [range: 1to 7]) were retreated upon progression with bortezomib administered intravenously. Patients were excluded from trial participation if they had peripheral neuropathy or neuropathic pain of Grade ‚Č•2. At least¬† six months after prior bortezomib therapy, bortezomib was restarted at the last tolerated dose of 1.3 mg/m 2 (n=93) or ‚ȧ 1 mg/m 2 (n=37) and given on Days 1, 4, 8 and 11 every¬† three weeks for maximum of eight cycles either as single agent or in combination with dexamethasone in accordance with the standard of care. Dexamethasone was administered in combination with bortezomib to 83 patients in Cycle 1 with an additional 11 patients receiving dexamethasone during the course of bortezomib retreatment cycles. The primary endpoint was best confirmed response to retreatment as assessed by European Group for Blood and Marrow Transplantation (EBMT) criteria.¬† Fifty of the 130 patients achieved a best confirmed response of Partial Response or better for an overall response rate of 38.5% (95% CI: 30.1, 47.4). One patient achieved a Complete Response and 49 achieved Partial Response. In the 50 responding patients, the median duration of response was 6.5 months and the range was 0.6 to 19.3 months.
14.2 Mantle Cell Lymphoma
A Randomized, Open-Label Clinical Study in Patients with Previously Untreated Mantle Cell Lymphoma A randomized, open-label, Phase 3 study (NCT00722137) was conducted in 487 adult patients with previously untreated mantle cell lymphoma (Stage II, III or IV) who were ineligible or not considered for bone marrow transplantation to determine whether bortezomib administered in combination with rituximab, cyclophosphamide, doxorubicin, and prednisone (BR-CAP) resulted in improvement in progression-free survival (PFS) when compared to the combination of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP). This clinical study utilized independent pathology confirmation and independent radiologic response assessment. Patients in the BR-CAP treatment arm received bortezomib (1.3 mg/m 2) administered intravenously on Days 1, 4, 8, and 11 (rest period Days 12 to 21); rituximab (375 mg/m 2) on Day 1; cyclophosphamide (750 mg/m 2) on Day 1; doxorubicin (50 mg/m 2) on Day 1; and prednisone (100 mg/m 2) on Day 1 through Day 5 of the 21 day treatment cycle. For patients with a response first documented at Cycle 6, two additional treatment cycles were allowed. Median patient age was 66 years, 74% were male, 66% were Caucasian and 32% were Asian. Sixty-nine percent of patients had a positive bone marrow aspirate and/or a positive bone marrow biopsy for MCL, 54% of patients had an International Prognostic Index (IPI) score of three (high‚ÄĎintermediate) or higher and 76% had Stage IV disease. The majority of the patients in both groups received six or more cycles of treatment, 84% in the BR-CAP group and 83% in the R-CHOP group. Median number of cycles received by patients in both treatment arms was six with 17% of patients in the R-CHOP group and 14% of subjects in the BR-CAP group receiving up to two additional cycles. The efficacy results for PFS, CR and ORR with a median follow-up of 40 months are presented in Table 18. The response criteria used to assess efficacy were based on the International Workshop to Standardize Response Criteria for Non-Hodgkin‚Äôs Lymphoma (IWRC). Final overall survival results at a median follow-up of 78.5 months are also presented in Table 18 and Figure 6. The combination of BR-CAP resulted in statistically significant prolongation of PFS compared with R-CHOP (see Table 18, Figure 5). Table 18: Summary of Efficacy Analyses in the Previously Untreated Mantle Cell Lymphoma Study
Efficacy Endpoint n: Intent to Treat patients  
BR-CAP    (n=243)
R-CHOP    (n=244)
Progression-Free Survival (by independent radiographic assessment)
Events n (%)  
133 (55) 
165 (68) 
 Median* (months)  (95% CI) 
 25 (20, 32)
 14 (12, 17)  
 Hazard ratio †  (95% CI) 
 0.63 (0.50, 0.79)
p-value ‡ 
<0.001 
Complete Response Rate (CR) § 
n (%)
108 (44) 
82 (34) 
(95% CI)
(38, 51) 
(28, 40) 
Overall Response Rate (CR + Cru + PR) ¶
n (%)  
214 (88)
208 (85)
    (95% CI)
(83, 92)
(80, 89)
 Overall Survival
 Events n(%)
  103 (42)
  138 (57)
 Median* (months) (95% CI)
  91 (71, NE)  
  56 (47, 69)  
Hazard Ratio †   (95% CI)
  0.66 (0.51, 0.85)
Note: All results are based on the analysis performed at a median follow-up duration of 40 months except for the overall survival analysis, which was performed at a median follow-up of 78.5 months.
CI = Confidence Interval; IPI = International Prognostic Index; LDH = Lactate dehydrogenase * Based on Kaplan-Meier product limit estimates. † Hazard ratio estimate is based on a Cox’s model stratified by IPI risk and stage of disease. A hazard ratio <1 indicates an advantage for BR-CAP. ‡  Based on Log rank test stratified with IPI risk and stage of disease. § Includes CR by independent radiographic assessment, bone marrow, and LDH using ITT population. ¶ Includes CR + Cru + PR by independent radiographic assessment, regardless of the verification by bone marrow and LDH, using ITT population.
Figure 5: Progression-Free Survival BR-CAP vs R-CHOP (previously Untreated Mantle Cell Lymphoma Study)
 
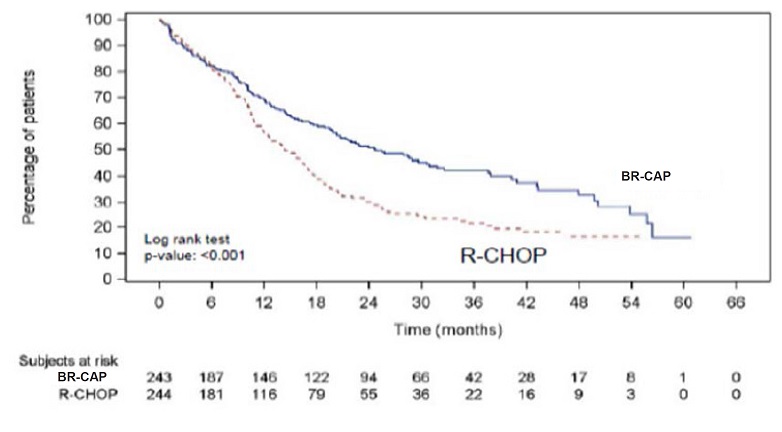
Key: R-CHOP=rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone;
BR-CAP= bortezomib, rituximab, cyclophosphamide, doxorubicin, and prednisone.
Figure 6: Overall Survival BR-CAP vs R-CHOP (previously Untreated Mantle Cell Lymphoma Study)
Key: R-CHOP = rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone; BR-CAP = bortezomib, rituximab, cyclophosphamide, doxorubicin, and prednisone.
A Phase 2 Single-Arm Clinical Study in Relapsed Mantle Cell Lymphoma after Prior Therapy  The safety and efficacy of bortezomib in relapsed or refractory mantle cell lymphoma were evaluated in an open-label, single-arm, multicenter study (NCT00063713) of 155 patients with progressive disease who had received at least one  prior therapy. The median age of the patients was 65 years (42, 89), 81% were male, and 92% were Caucasian. Of the total, 75% had one or more extra-nodal sites of disease, and 77% were Stage 4. In 91% of the patients, prior therapy included all of the following: an anthracycline or mitoxantrone, cyclophosphamide, and rituximab. A total of thirty-seven percent (37%) of patients were refractory to their last prior therapy. An intravenous bolus injection of bortezomib 1.3 mg/m 2/dose was administered twice weekly for  two weeks on Days 1, 4, 8, and 11 followed by a  ten day rest period (Days 12 to 21) for a maximum of 17 treatment cycles. Patients achieving a CR or CRu were treated for  four cycles beyond first evidence of CR or CRu. The study employed dose modifications for toxicity [see Dosage and Administration (2.6, 2.7)]. Responses to bortezomib are shown in Table 19. Response rates to bortezomib were determined according to the International Workshop Response Criteria (IWRC) based on independent radiologic review of CT scans. The median number of cycles administered across all patients was four; in responding patients the median number of cycles was eight. The median time to response was 40 days (range: 31 to 204 days). The median duration of follow-up was more than 13 months.
Table 19: Response Outcomes in a Phase 2 Relapsed Mantle Cell Lymphoma Study
Response Analyses (N = 155)
N (%)
95% CI
Overall Response Rate (IWRC) (CR + CRu + PR)
48 (31)
(24, 39)
Complete Response (CR + CRu)
12 (8)
(4, 13)
CR
10 (6)
(3, 12)
CRu
2 (1)
(0, 5)
Partial Response (PR)
36 (23)
(17, 31)
Duration of Response
Median
95% CI
CR + CRu + PR (N = 48)
9.3 months
(5.4, 13.8)
CR + CRu (N = 12)
15.4 months
(13.4, 15.4)
PR (N=36)
6.1 months
(4.2, 9.3)
15 References
1. ‚ÄúOSHA Hazardous Drugs‚ÄĚ (refer to antineoplastic weblinks including OSHA Technical Manual). OSHA. http://www.osha.gov/SLTC/hazardousdrugs/index.html
16 How Supplied/storage And Handling
Bortezomib for Injection is supplied as individually cartoned 10 mL vials containing 3.5 mg of bortezomib as a white to off-white cake or powder.
NDC 68001-541-36
3.5 mg single-dose vial
Unopened vials may be stored at controlled room temperature 25¬ļC (77¬ļF); excursions permitted from 15¬ļC to 30¬ļC (59¬ļF to 86¬ļF) [see USP Controlled Room Temperature]. Retain in original package to protect from light.
Follow guidelines for handling and disposal for hazardous drugs, including the use of gloves and other protective clothing to prevent skin contact 1.
17 Patient Counseling Information
Discuss the following with patients prior to treatment with bortezomib for injection:
Peripheral Neuropathy Advise patients to report the development or worsening of sensory and motor peripheral neuropathy to their healthcare provider [see Warnings and Precautions (5.1)]. Hypotension Advise patients to drink adequate fluids to avoid dehydration and to report symptoms of hypotension to their healthcare provider [see Warnings and Precautions (5.2)]. Instruct patients to seek medical advice if they experience symptoms of dizziness, light headedness or fainting spells, or muscle cramps. Cardiac Toxicity Advise patients to report signs or symptoms of heart failure to their healthcare provider [see Warnings and Precautions (5.3)]. Pulmonary Toxicity Advise patients to report symptoms of ARDS, pulmonary hypertension, pneumonitis, and pneumonia immediately to their healthcare provider [see Warnings and Precautions (5.4)]. Posterior Reversible Encephalopathy Syndrome (PRES) Advise patients to seek immediate medical attention for signs or symptoms of PRES [see Warnings and Precautions (5.5)]. Gastrointestinal Toxicity Advise patients to report symptoms of gastrointestinal toxicity to their healthcare provider and to drink adequate fluids to avoid dehydration. Instruct patients to seek medical advice if they experience symptoms of dizziness, light headedness or fainting spells, or muscle cramps [see Warnings and Precautions (5.6)]. Thrombocytopenia/Neutropenia Advise patients to report signs or symptoms of bleeding or infection immediately to their healthcare provider [see Warnings and Precautions (5.7)].
Tumor Lysis Syndrome Advise patients of the risk of tumor lysis syndrome and to drink adequate fluids to avoid dehydration [see Warnings and Precautions (5.8)]. Hepatic Toxicity Advise patients to report signs or symptoms of hepatic toxicity to their healthcare provider [see Warnings and Precautions (5.9)]. Thrombotic Microangiopathy Advise patients to seek immediate medical attention if any signs or symptoms of thrombotic microangiopathy occur [see Warnings and Precautions (5.10)] . Ability to Drive or Operate Machinery or Impairment of Mental Ability Bortezomib may cause fatigue, dizziness, syncope, orthostatic/postural hypotension. Advise patients not to drive or operate machinery if they experience any of these symptoms [see Warnings and Precautions (5.2, 5.5)]. Embryo-Fetal Toxicity Advise females of the potential risk to the fetus and to use effective contraception during treatment with bortezomib and for seven months following the last dose. Advise male patients with female partners of reproductive potential to use effective contraception during treatment with bortezomib and for four months following the last dose. Instruct patients to report pregnancy to their physicians immediately if they or their female partner becomes pregnant during treatment or within seven months following last dose [see Warnings and Precautions (5.11)] . Lactation Advise women not to breastfeed while receiving bortezomib and for two months after last dose [see Use in Specific Populations (8.2)]. Concomitant Medications Advise patients to speak with their physicians about any other medication they are currently taking. Diabetic Patients Advise patients to check their blood sugar frequently if using an oral antidiabetic medication and to notify their physicians of any changes in blood sugar level. Dermal Advise patients to contact their physicians if they experience rash, severe injection site reactions [ see Dosage and Administration (2.9)], or skin pain. Discuss with patients the option for antiviral prophylaxis for herpes virus infection [ see Adverse Reactions (6.1)]. Other Instruct patients to contact their physicians if they develop an increase in blood pressure, bleeding,fever, constipation, or decreased appetite.
Manufactured by:
MSN Laboratories Private Limited
Telangana ‚Äď 509 228,
INDIA
For BluePoint Laboratories
Rev: 05/2022
Recent Major Changes Section
Package Label.principal Display Panel
Bortezomib -Carton
Bortezomib-Vial-Label
Bortezomib-intravenous-sticker-label
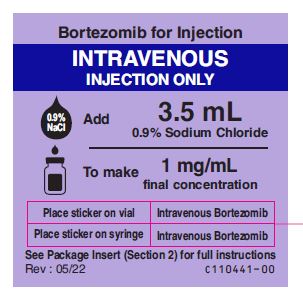
Bortezomib-subcutaneous-sticker-label
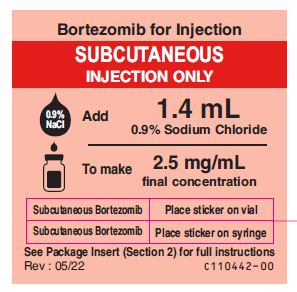
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site