Ropinirole (ropinirole hydrochloride 12 mg) Dailymed
Generic: ropinirole is used for the treatment of Parkinson Disease
Go PRO for all pill images
Recent Major Changes Section
Warnings and Precautions, Hallucinations/Psychotic-Like Behavior (5.5) 7/2021 Warnings and Precautions, Impulse Control/Compulsive Behaviors (5.7) 7/2021 Warnings and Precautions, Withdrawal Symptoms (5.9)                           7/2021 Warnings and Precautions, Melanoma-removal (5.10)                              7/2021
1 Indications And Usage
Ropinirole extended-release tablets are indicated for the treatment of Parkinson’s disease.
Ropinirole extended-release tablets are non-ergoline dopamine agonist indicated for the treatment of Parkinson’s disease. (1) 
2 Dosage And Administration
·    Ropinirole extended-release tablets are taken once daily, with or without food; tablets must be swallowed whole and not be chewed, crushed, or divided. (2.1)
·    The recommended starting dose is 2 mg taken once daily for 1 to 2 weeks; the dose should be increased by 2 mg/day at 1 week or longer intervals. The maximum recommended dose of ropinirole extended-release tablets are 24 mg/day. (2.2, 14.2)  
·    Renal Impairment: In patients with end-stage renal disease on hemodialysis, the maximum recommended dose is 18 mg/day. (2.2)  
·    If ropinirole extended-release tablets must be discontinued, it should be tapered gradually over a 7-day period; retitration of ropinirole extended-release tablets may be warranted if therapy is interrupted. (2.1, 2.2)  
·    Patients may be switched directly from immediate-release ropinirole to ropinirole extended-release tablets; the initial switching dose of ropinirole extended-release tablets should approximately match the total daily dose of immediate-release ropinirole. (2.3)
2.1 General Dosing Recommendations
 ·        Ropinirole extended-release tablets are taken once daily, with or without food [see Clinical Pharmacology (12.3)].
·        Tablets must be swallowed whole and must not be chewed, crushed, or divided.
·        If a significant interruption in therapy with ropinirole extended-release tablets has occurred, retitration of therapy may be warranted.
2.2 Dosing for Parkinson's Disease
The recommended starting dose of ropinirole extended-release tablets is 2 mg taken once daily for 1 to 2 weeks, followed by increases of 2 mg/day at weekly or longer intervals, based on therapeutic response and tolerability.  Monitor patients at least weekly during dose titration. Too rapid a rate of titration may lead to the selection of a dose that does not provide additional benefit, but increases the risk of adverse reactions.  
In fixed-dose studies designed to characterize the dose response to ropinirole extended-release tablets, there was no additional therapeutic benefit shown in patients with advanced stage Parkinson’s disease taking daily doses greater than 8 mg/day, or with early stage Parkinson’s disease taking doses greater than 12 mg/day [see Clinical Studies (14.1 and 14.2)]. Although the maximum recommended dose of ropinirole extended-release tablets is 24 mg, patients with advanced Parkinson’s disease should generally be maintained at daily doses of 8 mg or lower and patients with early Parkinson’s disease should generally be maintained at daily doses 12 mg or lower.
Ropinirole extended-release tablets should be discontinued gradually over a 7-day period [see Warnings and Precautions (5.9)].
 
Renal Impairment  
No dose adjustment is necessary in patients with moderate renal impairment (creatinine clearance of 30 to 50 mL/min). The recommended initial dose of ropinirole extended-release tablets for patients with end-stage renal disease on hemodialysis is 2 mg once daily. Further dose escalations should be based on tolerability and need for efficacy. The recommended maximum total daily dose is 18 mg/day in patients receiving regular dialysis. Supplemental doses after dialysis are not required. The use of ropinirole extended-release tablets in patients with severe renal impairment without regular dialysis has not been studied. 
2.3 Switching from Immediate-Release Ropinirole Tablets to Extended-Release Ropinirole Tablets
Patients may be switched directly from immediate-release ropinirole to extended-release ropinirole tablets. The initial dose of ropinirole extended-release tablets should approximately match the total daily dose of the immediate-release formulation of ropinirole, as shown in Table 1.
Table 1. Conversion from Immediate-Release Ropinirole Tablets to Extended-Release Ropinirole Tablets
Immediate-Release Ropinirole Tablets Total Daily Dose (mg)   Extended-Release Ropinirole Tablets Total Daily Dose (mg)     0.75 to 2.25  2  3 to 4.5  4  6  6  7.5 to 9  8  12  12  15 16  18 18   21 20   24  24
Following conversion to ropinirole extended-release tablets, the dose may be adjusted depending on therapeutic response and tolerability [see Dosage and Administration (2.2)].
2.4 Effect of Gastrointestinal Transit Time on Medication Release
Ropinirole extended-release tablets are designed to release medication over a 24-hour period. If rapid gastrointestinal transit occurs, there may be risk of incomplete release of medication and medication residue being passed in the stool.
3 Dosage Forms And Strengths
- 2 mg, pink, capsule shaped, film coated tablet, debossed with ‚ÄėL191‚Äô on one side and plain on other side.
- 4 mg, light brown, capsule shaped, film coated tablet, debossed with ‚ÄėL193‚Äô on one side and plain on other side.
- 6 mg, white to off white, capsule shaped, film coated tablet, debossed with ‚ÄėL321‚Äô on one side and plain on other side.
- 8 mg, dark brown to red, capsule shaped, film coated tablet, debossed with ‚ÄėL194‚Äô on one side and plain on other side.
- 12 mg, light green, capsule shaped, film coated tablet, debossed with ‚ÄėL195‚Äô on one side and plain on other side.
Tablets: 2 mg, 4 mg, 6 mg, 8 mg, and 12 mg (3)
4 Contraindications
 Ropinirole extended-release tablets are contraindicated in patients known to have a hypersensitivity/allergic reaction including urticaria, angioedema, rash, pruritus) to ropinirole or any of the excipients.
History of hypersensitivity/ allergic reaction (including urticaria, angioedema, rash, pruritus) to ropinirole or to any of the excipients (4)
5 Warnings And Precautions
‚ÄĘSudden onset of sleep and somnolence may occur (5.1) ‚ÄĘSyncope may occur (5.2) ‚ÄĘHypotension, including orthostatic hypotension may occur (5.3) ‚ÄĘElevation of blood pressure and changes in heart rate may occur (5.4) ‚ÄĘMay cause hallucinations and psychotic-like behaviors (5.5) ‚ÄĘMay cause or exacerbate dyskinesia (5.6) ‚ÄĘMay cause problems with impulse control or compulsive behaviors (5.7)
5.1 Falling Asleep during Activities of Daily Living and Somnolence
Patients treated with ropinirole extended-release tablets have reported falling asleep while engaged in activities of daily living, including driving or operating machinery, which sometimes resulted in accidents. Although many of these patients reported somnolence while on ropinirole, some perceived that they had no warning signs, such as excessive drowsiness, and believed that they were alert immediately prior to the event. Some have reported these events more than 1 year after initiation of treatment.
Among the 613 patients who received ropinirole extended-release tablets in flexible-dose clinical trials (Study 1 and Study 3), <1% of patients reported sudden onset of sleep and <1% of patients reported a motor vehicle accident in which it is not known if falling asleep was a contributing factor.
In a placebo-controlled fixed-dose trial in patients with advanced Parkinson’s disease (Study 2), sudden onset of sleep was reported in 4% of 276 patients on ropinirole extended-release tabletscompared with 3% of 74 patients on placebo. In a placebo-controlled fixed-dose trial in patients with early Parkinson’s disease (Study 4), sudden onset of sleep was reported in 5% of 146 patients on ropinirole extended-release tabletscompared with 0% of 40 patients on placebo [see Adverse Reactions (6.1)]. The incidence of sudden onset of sleep was not dose-related in either trial. 
During a placebo-controlled flexible-dose trial in patients with advanced Parkinson’s disease (Study 1), somnolence was reported in 7% of 202 patients on ropinirole extended-release tablets compared with 4% of 191 patients on placebo. During a flexible-dose, active-control, crossover trial in early Parkinson’s disease (Study 3), somnolence was reported in 11% of 140 patients on ropinirole extended-release tablets compared with 15% of 149 patients on an immediate-release formulation of ropinirole tablets[see Adverse Reactions (6.1)].  
In a placebo-controlled fixed-dose trial in patients with advanced Parkinson’s disease (Study 2), somnolence was reported in 8% of 276 patients on ropinirole extended-release tablets compared with 5% of 74 patients on placebo. In a placebo-controlled fixed-dose trial in patients with early Parkinson’s disease (Study 4), somnolence was reported in 10% of 146 patients on ropinirole extended-release tablets compared with 5% of 40 patients on placebo [see Adverse Reactions (6.1)]. The frequency of reported somnolence was not dose-related. 
It has been reported that falling asleep while engaged in activities of daily living usually occurs in a setting of pre-existing somnolence, although patients may not give such a history. For this reason, prescribers should reassess patients for drowsiness or sleepiness, especially since some of the events occur well after the start of treatment. Prescribers should also be aware that patients may not acknowledge drowsiness or sleepiness until directly questioned about drowsiness or sleepiness during specific activities.
Before initiating treatment with ropinirole extended-release tablets, patients should be advised of the potential to develop drowsiness and specifically asked about factors that may increase the risk with ropinirole extended-release tablets such as concomitant sedating medications or alcohol, the presence of sleep disorders, and concomitant medications that increase ropinirole plasma levels (e.g., ciprofloxacin) [see Drug Interactions (7.1)]. If a patient develops significant daytime sleepiness or episodes of falling asleep during activities that require active participation (e.g., driving a motor vehicle, conversations, eating), ropinirole extended-release tablets should ordinarily be discontinued [see Dosage and Administration (2.2)]. If a decision is made to continue ropinirole extended-release tablets, patients should be advised to not drive and to avoid other potentially dangerous activities. There is insufficient information to establish that dose reduction will eliminate episodes of falling asleep while engaged in activities of daily living.
5.2 Syncope
Syncope, sometimes associated with bradycardia, was observed in association with treatment with ropinirole extended-release tablets in patients with Parkinson’s disease.
In a placebo-controlled flexible-dose trial in patients with advanced Parkinson’s disease (Study 1), syncope occurred in 1% of patients on ropinirole extended-release tablets compared with 0% of patients on placebo [see Adverse Reactions (6.1)].
In the placebo-controlled fixed-dose trials (Study 2 and Study 4), one patient on ropinirole extended-release tablets with advanced Parkinson's disease and one patient on ropinirole extended-release tablets with early Parkinson's disease experienced syncope during the titration period for ropinirole extended-release tablets. Both patients discontinued prematurely from the respective trials. 
Because the trials conducted with ropinirole extended-release tablets excluded patients with significant cardiovascular disease, patients with significant cardiovascular disease should be treated with caution.
5.3 Hypotension/Orthostatic Hypotension
Patients with Parkinson’s disease may have impaired ability to respond normally to a fall in blood pressure after standing from lying down or seated position. Patients on ropinirole extended-release tablets should be monitored for signs and symptoms of orthostatic hypotension, especially during dose escalation, and should be informed of the risk for syncope and hypotension [see Patient Counseling Information (17)].
 
In a placebo-controlled flexible-dose trial in patients with advanced Parkinson‚Äôs disease (Study 1), hypotension was reported as an adverse reaction in 2% of patients on ropinirole extended-release tablets, compared with 0% of patients on placebo. In this study, orthostatic hypotension was reported as an adverse reaction in 5% of patients on ropinirole extended-release tablets, and 1% of patients on placebo [see Adverse Reactions (6.1)]. Some patients experienced hypotension or orthostatic hypotension that started in the titration and persisted into the maintenance period. There was also a higher incidence for the combined adverse reaction terms of ‚Äúhypotension‚ÄĚ, ‚Äúorthostatic hypotension‚ÄĚ, ‚Äúdizziness‚ÄĚ, ‚Äúvertigo‚ÄĚ, and ‚Äúblood pressure decreased‚ÄĚ in 7% of patients on ropinirole extended-release tablets compared with 3% of patients on placebo. The increased incidence of those events with ropinirole extended-release tablets was observed in a setting in which patients were very carefully titrated, and patients with clinically relevant cardiovascular disease or symptomatic orthostatic hypotension at baseline had been excluded from this trial. The frequency of orthostatic hypotension (systolic blood pressure decrements ‚Č•20 mm Hg) at any time during the trial was 38% for ropinirole extended-release tablets vs. 31% for placebo.
In a placebo-controlled fixed-dose trial in patients with advanced Parkinson‚Äôs disease (Study 2), a decrease in standing systolic blood pressure of ‚Č•20 mm Hg was observed in 26% of patients on ropinirole extended-release tablets compared with 18% of patients on placebo.
In a placebo-controlled fixed-dose trial of patients with early Parkinson's disease (Study 4), a decrease in standing systolic blood pressure of ‚Č•20 mm Hg was observed in 14% of patients on ropinirole extended-release tablets compared with 10% of patients on placebo.
Significant decrements in blood pressure unrelated to standing were also reported in some patients taking ropinirole extended-release tablets. 
5.4 Elevation of Blood Pressure and Changes in Heart Rate
The potential for elevation in blood pressure and changes in heart rate should be considered when treating patients with cardiovascular disease with ropinirole extended-release tablets.
In a placebo-controlled flexible-dose trial in patients with advanced Parkinson‚Äôs disease (Study 1), the frequency of systolic blood pressure increase (‚Č•40mm Hg) in the semi-supine position was 8% of patients on ropinirole extended-release tablets vs. 5% of patients on placebo. In the standing position, the frequency of systolic blood pressure increase (‚Č•40 mm Hg) was 9% for ropinirole extended-release tablets vs. 6% for placebo. There was no clear effect of ropinirole extended-release tablets on average heart rate.
In a placebo-controlled fixed-dose trial in patients with advanced Parkinson’s disease (Study 2), hypertension was reported as an adverse reaction in 3% of patients on ropinirole extended-release tablets, compared with 1% of patients on placebo [see Adverse Reactions (6.1)].
In a placebo-controlled fixed-dose trial in patients with early Parkinson’s disease (Study 4), hypertension was reported as an adverse reaction in 5% of patients on ropinirole extended-release tablets, compared with 0% of patients on placebo [see Adverse Reactions (6.1)].
5.5 Hallucinations/Psychotic-Like Behavior
In a placebo-controlled flexible-dose trial in patients with advanced Parkinson’s disease (Study 1), 8% of patients on ropinirole extended-release tablets reported hallucination, compared with 2% of patients on placebo [see Adverse Reactions (6.1)]. Hallucinations led to discontinuation of treatment in 2% of patients on ropinirole extended-release tablets and 1% of patients on placebo. The incidence of hallucination was increased in elderly patients (i.e., older than 65 years) treated with ropinirole extended-release tablets [see Use in Specific Populations (8.5)].
In a placebo-controlled fixed-dose trial in patients with advanced Parkinson’s disease (Study 2), the incidence of hallucination was 3% in patients on ropinirole extended-release tablets compared with 0% in patients on placebo [see Adverse Reactions (6.1)]. The most common adverse reaction associated with study discontinuation for any dose of ropinirole extended-release tablets was hallucination (2%).
Postmarketing reports indicate that patients with Parkinson’s disease may experience new or worsening mental status and behavioral changes, which may be severe, including psychotic-like behavior during treatment with ropinirole extended-release tablets or after starting or increasing the dose of ropinirole extended-release tablets. Other drugs prescribed to improve the symptoms of Parkinson’s disease can have similar effects on thinking and behavior. This abnormal thinking and behavior can consist of one or more of a variety of manifestations including paranoid ideation, delusions, hallucinations, confusion, psychotic-like behavior, symptoms of mania (e.g., insomnia, psychomotor agitation), disorientation, aggressive behavior, agitation, and delirium.
Patients with a major psychotic disorder should ordinarily not be treated with ropinirole extended-release tablets because of the risk of exacerbating the psychosis. In addition, certain medications used to treat psychosis may exacerbate the symptoms of Parkinson’s disease and may decrease the effectiveness of ropinirole extended-release tablets [see Drug Interactions (7.3)].
5.6 Dyskinesia
Ropinirole extended-release tablets may cause or exacerbate pre-existing dyskinesia in patients treated with L-dopa for Parkinson’s disease.
In a placebo-controlled flexible-dose trial in patients with advanced Parkinson’s disease (Study 1) the incidence of dyskinesia was 13% in patients on ropinirole extended-release tabletsand 3%  in patients on placebo [see Adverse Reactions (6.1)].
In a placebo-controlled fixed-dose trial in patients with advanced Parkinson’s disease (Study 2), the incidence of dyskinesia was 7% in patients on ropinirole extended-release tablets compared with 1% in patients on placebo [see Adverse Reactions (6.1)].
Decreasing the dose of dopaminergic medications may ameliorate this adverse reaction. 
5.7 Impulse Control/Compulsive Behaviors
Reports suggest that patients can experience intense urges to gamble, increased sexual urges, intense urges to spend money, binge or compulsive eating, and/or other intense urges, and the inability to control these urges while taking one or more of the medications, including ropinirole extended-release tablets, that increase central dopaminergic tone. In some cases, although not all, these urges were reported to have stopped when the dose was reduced or the medication was discontinued. Because patients may not recognize these behaviors as abnormal, it is important for prescribers to specifically ask patients or their caregivers about the development of new or increased gambling urges, sexual urges, uncontrolled spending, binge or compulsive eating, or other urges while being treated with ropinirole extended-release tablets for Parkinson’s disease. Physicians should consider dose reduction or stopping the medication if a patient develops such urges while taking ropinirole extended-release tablets.
5.8 Withdrawal-Emergent Hyperpyrexia and Confusion
A symptom complex resembling the neuroleptic malignant syndrome (characterized by elevated temperature, muscular rigidity, altered consciousness, and autonomic instability), with no other obvious etiology, has been reported in association with rapid dose reduction of, withdrawal of, or changes in, dopaminergic therapy. Therefore, it is recommended that the dose be tapered at the end of treatment with ropinirole extended-release tablets as a prophylactic measure [see Dosage and Administration (2.2)].
5.9 Withdrawal Symptoms
Symptoms including insomnia, apathy, anxiety, depression, fatigue, sweating, and pain have been reported during taper or after discontinuation of dopamine agonists, including ropinirole extended-release tablets. These symptoms generally do not respond to levodopa.
Prior to discontinuation of ropinirole extended-release tablets, patients should be informed about the potential withdrawal symptoms and monitored during and after discontinuation. In case of severe withdrawal symptoms, a trial re-administration of a dopamine agonist at the lowest effective dose may be considered.
5.10 Fibrotic Complications
Cases of retroperitoneal fibrosis, pulmonary infiltrates, pleural effusion, pleural thickening, pericarditis, and cardiac valvulopathy have been reported in some patients treated with ergot-derived dopaminergic agents. While these complications may resolve when the drug is discontinued, complete resolution does not always occur.
Although these adverse reactions are believed to be related to the ergoline structure of these compounds, whether other, non-ergot-derived dopamine agonists, such as ropinirole, can cause them is unknown.
Cases of possible fibrotic complications, including pleural effusion, pleural fibrosis, interstitial lung disease, and cardiac valvulopathy have been reported in the development program and postmarketing experience for ropinirole. In the clinical development program (N = 613), 2 patients treated with ropinirole extended-release tablets had pleural effusion. While the evidence is not sufficient to establish a causal relationship between ropinirole and these fibrotic complications, a contribution of ropinirole cannot be excluded.
5.11 Retinal Pathology
Retinal degeneration was observed in albino rats in the 2-year carcinogenicity study at all doses tested. The lowest dose tested (1.5 mg/kg/day) is less than the maximum recommended human dose (MRHD) of 24 mg/day on a mg/m2 basis. Retinal degeneration was not observed in a 3-month study in pigmented rats, in a 2-year carcinogenicity study in albino mice, or in 1-year studies in monkeys or albino rats. The significance of this effect for humans has not been established, but involves disruption of a mechanism that is universally present in vertebrates (e.g., disk shedding).
Ocular electroretinogram assessments were conducted during a 2-year, double-blind, multicenter, flexible-dose, L-dopa-controlled clinical trial of immediate-release ropinirole in patients with Parkinson’s disease; 156 patients (78 on immediate-release ropinirole, mean dose: 11.9 mg/day and 78 on L-dopa, mean dose: 555.2 mg/day) were evaluated for evidence of retinal dysfunction through electroretinograms. There was no clinically meaningful difference between the treatment groups in retinal function over the duration of the trial.
5.12 Binding to Melanin
Ropinirole binds to melanin-containing tissues (e.g., eyes, skin) in pigmented rats. After a single dose, long-term retention of drug was demonstrated, with a half-life in the eye of 20 days.
6 Adverse Reactions
The following adverse reactions are described in more detail in other sections of the label: ‚Äʬ†Hypersensitivity [see Contraindications (4)] ‚Äʬ†Falling asleep during activities of daily living and somnolence [see Warnings and Precautions (5.1)] ‚Äʬ†Syncope [see Warnings and Precautions (5.2)] ‚Äʬ†Hypotension/ orthostatic hypotension [see Warnings and Precautions (5.3)] ‚Äʬ†Elevation of blood pressure and changes in heart rate [see Warnings and Precautions (5.4)] ‚Äʬ†Hallucinations/ psychotic-like behavior [see Warnings and Precautions (5.5)] ‚Äʬ†Dyskinesia [see Warnings and Precautions (5.6)] ‚Äʬ†Impulse control/compulsive behaviors [see Warnings and Precautions (5.7)] ‚Äʬ†Withdrawal-emergent hyperpyrexia and confusion [see Warnings and Precautions (5.8)] ‚Äʬ†Withdrawal symptoms [see Warnings and Precautions (5.9)]¬† ‚Äʬ†Fibrotic complications [see Warnings and Precautions (5.10)] ‚Äʬ†Retinal pathology [see Warnings and Precautions (5.11)]¬† ¬†
·     Most common adverse reactions (incidence for ropinirole extended-release tablets all doses at least 5% greater than placebo in either a flexible- or fixed-dose study) in patients with advanced Parkinson’s disease were nausea, dyskinesia, dizziness, and hallucination. (6.1) 
·     Most common adverse reactions (incidence for ropinirole extended-release tablets all doses at least 5% greater than placebo in fixed-dose study) in patients with early Parkinson’s disease not taking L-dopa were nausea, somnolence, sudden onset of sleep, hypertension, and headache. In a flexible-dose study in patients with early Parkinson's, the most common adverse reactions (at least 5% incidence for ropinirole extended-release tablets) were nausea, somnolence, abdominal pain/discomfort, dizziness, headache, and constipation. (6.1)  
 
To report SUSPECTED ADVERSE REACTIONS, contact Alembic Pharmaceuticals Limited at 1-866-210-9797 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch  
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug (or of another development program of a different formulation of the same drug) and may not reflect the rates observed in practice.
During the premarketing development of ropinirole extended-release tablets, patients with advanced Parkinson’s disease received ropinirole extended-release tablets or placebo as adjunctive therapy with L-dopa in a flexible-dose clinical trial. In a flexible-dose trial, patients with early Parkinson’s disease were treated with ropinirole extended-release tablets or the immediate-release formulation of ropinirole tablets without L-dopa. In addition, placebo-controlled, fixed-dose, postmarketing trials evaluated the dose response of ropinirole extended-release tablets in patients with advanced Parkinson’s disease taking L-dopa and in patients with early Parkinson’s disease without concomitant L-dopa. 
 
Advanced Parkinson’s Disease (with L-dopa)
Study 1 was a 24-week, double-blind, placebo-controlled, flexible-dose trial in patients with advanced Parkinson’s disease. In Study 1, the most commonly observed adverse reactions in patients treated with ropinirole extended-release tablets (incidence at least 5% greater than placebo) were dyskinesia, nausea, dizziness, and  hallucinations.
In Study 1, approximately 6% of patients treated with ropinirole extended-release tablets discontinued treatment due to adverse reactions, compared with 5% of patients who received placebo. The most common adverse reaction in patients treated with ropinirole extended-release tablets causing discontinuation of treatment with ropinirole extended-release tablets in Study 1 was hallucination (2%) 
Table 2 uls adverse reactions that occurred in at least 2% (and were numerically greater than placebo) of patients with advanced Parkinson’s disease treated with ropinirole extended-release tablets who participated in Study 1. In this trial, either ropinirole extended-release tablets or placebo was used as an adjunct to L-dopa. 
                                               
Table 2. Incidence of Adverse Reactions in a Placebo-Controlled Flexible-Dose Trial in Advanced Stage Parkinson’s Disease in Patients Taking L-dopa (Study 1) (Events ³ 2% of Patients Treated with Ropinirole Extended-Release Tablets and More Common than on Placebo)a 
 
Body System/Adverse Reaction  Ropinirole Extended-Release Tablets   (n = 202) %  Placebo (n = 191) %  Ear and labyrinth disorders Vertigo 4 2 Gastrointestinal disorders     Nausea 11 4 Abdominal pain/discomfort 6 3 Constipation 4 2 Diarrhea 3 2 Dry mouth 2 <1 General disorders     Edema peripheral 4 1 Injury, poisoning, and procedural complication     Fallb 2 1 Musculoskeletal and connective tissue disorders     Back pain 3 2 Nervous system disorders     Dyskinesiab 13 3 Dizziness 8 3 Somnolence 7 4 Psychiatric disorders     Hallucination 8 2 Anxiety 2 1 Vascular disorders     Orthostatic hypotension 5 1 Hypertensionb 3 2 Hypotension 2 0
aPatients may have reported multiple adverse reactions during the trial or at discontinuation; thus, patients may be included in more than one category.
bDose-related.
 
Although this trial was not designed for optimally characterizing dose-related adverse reactions, there was a suggestion (based upon comparison of incidence of adverse reactions across dose ranges for ropinirole extended-release tablets and placebo) that the incidence for dyskinesia, hypertension, and fall was dose-related to ropinirole extended-release tablets.
During the titration phase, the incidence of adverse reactions in descending order of percent treatment difference was dyskinesia, nausea, abdominal pain/discomfort, orthostatic hypotension, dizziness, vertigo, hypertension, peripheral edema, and dry mouth. During the maintenance phase, the most frequently observed adverse reactions were dyskinesia, nausea, dizziness, hallucination, somnolence, fall, hypertension, abnormal dreams, constipation, chest pain, bronchitis, and nasopharyngitis. Some adverse reactions developing in the titration phase persisted(¬≥7 days) into the maintenance phase. These ‚Äúpersistent‚ÄĚ adverse reactions included dyskinesia, hallucination, orthostatic hypotension, and dry mouth.
The incidence of adverse reactions was similar in women and men.
Study 2 was an 18-week, double-blind, placebo-controlled, fixed-dose, dose-response trial in patients with advanced Parkinson’s disease. In Study 2, approximately 7% of patients treated with any dose of ropinirole extended-release tablets discontinued prematurely during the titration phase because of adverse reactions, compared with 4% of patients on placebo. The percentage of patients who discontinued from the study because of an adverse reaction was 4% for ropinirole extended-release tablets 4 mg, 9% for ropinirole extended-release tablets 8 mg, 8% for ropinirole extended-release tablets 12 mg, 8% for ropinirole extended-release tablets 16 mg, and 0% for ropinirole extended-release tablets 24 mg [see Warnings and Precautions (5.2, 5.5)]. Table 3 uls adverse reactions with an incidence of at least 5% of patients in any dose group of ropinirole extended-release tablets and numerically higher than on placebo in Study 2. The most common adverse reaction (incidence for ropinirole extended-release tablets all doses at least 5% greater than placebo) was dyskinesia.
 
Table 3. Incidence of Adverse Reactions in a Placebo-Controlled Fixed-Dose Trial in Advanced Stage Parkinson‚Äôs Disease in Patients Taking L-dopa (Study 2) (Events ‚Č•5% of Patients Treated with any Dose of Ropinirole Extended-Release Tablets¬†and More Common than on Placebo)
 
Adverse Reaction  Placebo N = 74 % Ropinirole Extended-Release Tablets   4 mg N = 25  % 8 mg N = 76  % 12 mg   N = 75 % 16 mg     N = 75 % 24 mg    N = 25 % All Doses      N = 276  % Nervous system disorders               Somnolence 5 4 5 12 11 0 8 Dyskinesia 1 4 4 7 11 4 7 Dizziness 3 8 4 8 5 4 6 Sudden onset of sleep 3 8 5 4 1 0 4 Vascular disorders                 Hypertension 1 8 1 1 4 8 3 Infections and infestations               Nasopharyngitis 1 0 3 3 0 8 2 Musculoskeletal and connective tissue disorders               Arthralgia 0 0 3 0 3 8 2 Psychiatric disorders               Insomnia 0 0 0 1 5 0 2
 
Early Parkinson’s Disease (without L-dopa)
Study 3 was a 36-week, flexible-dose crossover trial in patients with early Parkinson‚Äôs disease who were first treated with ropinirole extended-release tablets or the immediate-release formulation of ropinirole tablets and then crossed over to treatment with the other formulation. In Study 3, the most commonly observed adverse reactions (‚Č•5%) in patients treated with ropinirole extended-release tablets¬†were nausea (19%), somnolence (11%), abdominal pain/discomfort (7%), dizziness (6%), headache (6%), and constipation (5%).
Study 4 was an 18-week, double-blind, placebo-controlled, fixed-dose, dose-response trial in patients with early Parkinson’s disease. Overall, 7% of patients treated with any dose of ropinirole extended-release tablets, including 6% during the titration phase, discontinued prematurely from the study because of adverse reactions compared with 5% of patients on placebo. The percentage of patients discontinuing prematurely because of an adverse reaction was 8% for ropinirole extended-release tablets 2 mg, 5% for ropinirole extended-release tablets 4 mg, 8% for ropinirole extended-release tablets 8 mg, 5% for ropinirole extended-release tablets 12 mg, and 15% for ropinirole extended-release tablets 24 mg. 
Table 4 uls adverse reactions with an incidence of at least 10% of patients in any dose group of ropinirole extended-release tablets and numerically higher than on placebo in Study 4. The most common adverse reactions (incidence for ropinirole extended-release tablets all doses at least 5% greater than placebo) were nausea, somnolence, sudden onset of sleep, hypertension, and headache.
 
Table 4. Incidence of Adverse Reactions in a Double-Blind, Placebo-Controlled, Fixed-Dose Trial in Early Stage Parkinson‚Äôs Disease (Study 4) (Events ‚Č•10% of Patients Treated with any Dose of Ropinirole Extended-Release Tablets and Greater¬†Percent than on Placebo)
 
Adverse Reaction  Placebo N = 40 %  Ropinirole Extended-Release Tablets   2 mg N = 13 %  4 mg N = 41 %  8 mg N = 40 %  12 mg N = 39 %  24 mg N = 13 %  All Doses N = 146 %  Gastrointestinal disorders               Nausea 8 8 15 33 10 15 18 Vomiting 5 0 5 10 0 0 4 Nervous system disorders               Somnolence 5 15 12 10 8 8 10 Headache 3 8 10 8 5 15 8 Dizziness 5 0 5 10 8 8 7 Sudden onset of sleep 0 0 5 0 10 8 5 Vascular disorders               Hypertension 0 0 5 5 3 15 5 Musculoskeletal and connective tissue disorders               Back pain   3 0 5 3 3 15 4
 
Laboratory Abnormalities  
In the fixed-dose trial in advanced Parkinson’s disease (Study 2), 11% of patients on ropinirole extended-release tablets exhibited a shift in serum creatine phosphokinase (CPK) from normal at baseline to above the normal reference range during treatment, compared with 6% of patients on placebo. There was no clear dose response for abnormal shifts in CPK levels in patients with early or advanced stage Parkinson’s disease in either fixed-dose trial.
In the fixed-dose trial in early Parkinson’s disease patients (Study 4), serum CPK shifted during treatment from normal to above the normal reference range in 10% of patients on ropinirole extended-release tablets and in 5% of patients on placebo.
6.2 Adverse Reactions Observed during the Clinical Development of the Immediate-Release Formulation of Ropinirole Tablets for Parkinson's Disease (Advanced and Early)
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug (or of another development program of a different formulation of the same drug) and may not reflect the rates observed in practice.
In patients with advanced Parkinson’s disease who were treated with the immediate-release formulation of ropinirole tablets, the most common adverse reactions (³5% treatment difference from placebo presented in order of decreasing treatment difference frequency) were dyskinesia (21%), somnolence (12%), nausea (12%), dizziness (10%), confusion (7%), hallucinations (6%), headache (5%), and increased sweating (5%). In patients with early Parkinson’s disease who were treated with the immediate-release formulation of ropinirole tablets, the most common adverse reactions (³5% treatment difference from placebo presented in order of decreasing treatment difference frequency) were nausea (38%), somnolence (34%), dizziness (18%), syncope (11%), asthenic condition (11%), viral infection (8%), leg edema (6%), vomiting (5%), and dyspepsia (5%).
6.3 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of ropinirole extended-release tablets. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
General Disorders and Administration Site Conditions
  Withdrawal Symptoms [see Warnings and Precautions (5.9)]
7 Drug Interactions
·    Inhibitors or inducers of CYP1A2: May alter the clearance of ropinirole; dose adjustment of ropinirole extended-release tablets may be required. (7.1, 12.3)
·     Hormone replacement therapy (HRT): Starting or stopping HRT treatment may require dose adjustment of ropinirole extended-release tablets.  (7.2, 12.3)
·    Dopamine antagonists (e.g., neuroleptics  metoclopramide): May reduce efficacy of ropinirole extended-release tablets. (7.3)
7.1 Cytochrome P450 1A2 Inhibitors and Inducers
In vitro metabolism studies showed that  cytochrome P450 1A2 (CYP1A2)  is the major enzyme responsible for the metabolism of ropinirole. There is thus the potential for inducers or inhibitors of this enzyme to alter the clearance of ropinirole. Therefore, if therapy with a drug known to be a potent inducer or inhibitor of CYP1A2 is stopped or started during treatment with ropinirole extended-release tablets, adjustment of the dose of ropinirole extended-release tablets may be required. Coadministration of ciprofloxacin, an inhibitor of CYP1A2, with immediate-release ropinirole increases the AUC and Cmax of ropinirole [see Clinical Pharmacology (12.3)]. Cigarette smoking is expected to increase the clearance of ropinirole since CYP1A2 is known to be induced by smoking [see Clinical Pharmacology (12.3)].
7.2 Estrogens
Population pharmacokinetic analysis revealed that higher doses of estrogens (usually associated with hormone replacement therapy) reduced the clearance of ropinirole. Starting or stopping hormone replacement therapy may require adjustment of dosage of ropinirole extended-release tablets [see Clinical Pharmacology (12.3)].
7.3 Dopamine Antagonists
Because ropinirole is a dopamine agonist, it is possible that dopamine antagonists such as neuroleptics (e.g., phenothiazines, butyrophenones, thioxanthenes) or metoclopramide may reduce the efficacy of  ropinirole extended-release tablets.  
8 Use In Specific Populations
Pregnancy: Based on animal data, may cause fetal harm. (8.1)
8.1 Pregnancy
Risk Summary  
There are no adequate data on the developmental risk associated with the use of ropinirole extended-release tablets in pregnant women. In animal studies, ropinirole had adverse effects on development when administered to pregnant rats at doses similar to (neurobehavioral impairment) or greater than (teratogenicity and embryolethality at >36 times) the MRHD for Parkinson’s disease. Ropinirole doses associated with teratogenicity and embryolethality in pregnant rats were associated with maternal toxicity. In pregnant rabbits, ropinirole potentiated the teratogenic effects of L-dopa when these drugs were administered in combination [see Data].
In the U.S. general population, the estimated background risk of major birth defects and of miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. The background risk of major birth defects and miscarriage in the indicated populations is unknown.
 
Data  
 
Animal Data: Oral administration of ropinirole (0, 20, 60, 90, 120, or 150 mg/kg/day) to pregnant rats during organogenesis resulted in embryolethality, increased incidence of fetal malformations (digit, cardiovascular, and neural tube defects) and variations, and decreased fetal weight at the 2 highest doses. These doses were also associated with maternal toxicity. The highest no-effect dose for adverse effects on embryofetal development (90 mg/kg/day) is approximately 36 times the MRHD for Parkinson’s disease (24 mg/day) on a body surface area (mg/m2) basis.
No effect on embryofetal development was observed in rabbits when ropinirole was administered alone during organogenesis at oral doses of 0, 1, 5, or 20 mg/kg/day (up to 16 times the MRHD on a mg/m2 basis). In pregnant rabbits, there was a greater incidence and severity of fetal malformations (primarily digit defects) when ropinirole (10 mg/kg/day) was administered orally during gestation in combination with L-dopa (250 mg/kg/day) than when L-dopa was administered alone. This drug combination was also associated with maternal toxicity.
 
Oral administration of ropinirole (0, 0.1, 1, or 10 mg/kg/day) to rats during late gestation and continuing throughout lactation resulted in neurobehavioral impairment (decreased startle response) and decreased body weight in offspring at the highest dose. The no-effect dose of 1 mg/kg/day is less than the MRHD on a mg/m2 basis.
8.2 Lactation
Risk Summary  
There are no data on the presence of ropinirole in human milk, the effects of ropinirole on the breastfed infant, or the effects of ropinirole on milk production. However, inhibition of lactation is expected because ropinirole inhibits secretion of prolactin in humans. Ropinirole or metabolites, or both, are present in rat milk.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for ropinirole extended-release tablets and any potential adverse effects on the breastfed infant from ropinirole or from the underlying maternal condition. 
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established. 
8.5 Geriatric Use
Dose adjustment is not necessary in elderly (65 years and older) patients, as the dose of ropinirole extended-release tablets are  individually titrated to clinical therapeutic response and tolerability. Pharmacokinetic trials conducted in patients demonstrated that oral clearance of ropinirole is reduced by 15% in patients older than  65 years compared with younger patients [see Clinical Pharmacology (12.3)]. 
In flexible-dose clinical trials of ropinirole extended-release tablets, 387 patients were 65 years and older and 107 patients were 75 years and older. Among patients receiving ropinirole extended-release tablets, hallucination was more common in elderly patients (10%) compared with non-elderly patients (2%). In these trials, the incidence of overall adverse reactions increased with increasing age for both patients receiving ropinirole extended-release tablets and placebo.
In the fixed-dose clinical trials of ropinirole extended-release tablets, 176 patients were 65 years and older and 73 were 75 and older. Among patients with advanced Parkinson’s disease receiving ropinirole extended-release tablets, vomiting and nausea were more common in patients greater than 65 years (5% and 9%, respectively) compared with patients less than 65 (1% and 7%, respectively). 
8.6 Renal Impairment
No dose adjustment is necessary in patients with moderate renal impairment (creatinine clearance of 30 to 50 mL/min). For patients with end-stage renal disease on hemodialysis, a reduced maximum dose is recommended  [see Dosage and Administration (2.2), Clinical Pharmacology (12.3)].
The use of ropinirole extended-release tablets in patients with severe renal impairment (creatinine clearance  <30 mL/min) without regular dialysis has not been studied.
8.7 Hepatic Impairment
The pharmacokinetics of ropinirole have not been studied in patients with hepatic impairment.
10 Overdosage
The symptoms of overdose with ropinirole extended-release tablets are related to its dopaminergic activity. General supportive measures are recommended. Vital signs should be maintained, if necessary.
In clinical trials, there have been patients who accidentally or intentionally took more than their prescribed dose of ropinirole. The largest overdose reported with immediate-release ropinirole in clinical trials was 435 mg taken over a 7-day period (62.1 mg/day). Of patients who received a dose greater than 24 mg/day, reported symptoms included adverse events commonly reported during dopaminergic therapy (nausea, dizziness), as well as visual hallucinations, hyperhidrosis, claustrophobia, chorea, palpitations, asthenia, and nightmares. Additional symptoms reported for overdoses included vomiting, increased coughing, fatigue, syncope, vasovagal syncope, dyskinesia, agitation, chest pain, orthostatic hypotension, somnolence, and confusional state.
11 Description
Ropinirole extended-release tablets contain ropinirole, a non-ergoline dopamine agonist as the hydrochloride salt. The chemical name of ropinirole hydrochloride is 4-[2-(dipropylamino)ethyl]-1,3-dihydro-2H-indol-2-one and the empirical formula is C16H24N2O‚ÄĘHCl. The molecular weight is 296.84 (260.38 as the free base).
The structural formula is:
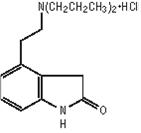
Ropinirole hydrochloride is a white to yellow solid with a melting range of 243¬į to 250¬įC and a solubility of 133 mg/mL in water. Each capsule shaped, film coated tablet contains 2.28 mg, 4.56 mg, 6.84 mg, 9.12 mg, or 13.68 mg ropinirole hydrochloride equivalent to ropinirole 2 mg, 4 mg, 6 mg, 8 mg, or 12 mg, respectively. Inactive ingredients consist of carboxymethylcellulose sodium, colloidal silicon dioxide, hydrogenated castor oil, hypromellose, magnesium stearate, povidone, pregelatinized starch, ethylcellulose and one or more of the following: FD&C Blue No. 2 aluminum lake, ferric oxides (black, red, yellow), polyethylene glycol 6000, polyethylene glycol 8000, titanium dioxide, talc.
12 Clinical Pharmacology
12.1 Mechanism of Action
Ropinirole is a non-ergoline dopamine agonist.
The precise mechanism of action of ropinirole as a treatment for Parkinson’s disease is unknown, although it is thought  to  be related to its ability to stimulate dopamine D2  receptors within the caudate-putamen in the brain.
12.2 Pharmacodynamics
Clinical experience with dopamine agonists, including ropinirole, suggests an association with impaired ability to regulate blood pressure resulting  in  orthostatic hypotension, especially during dose escalation. In some subjects in clinical trials, blood pressure changes were associated with the emergence of orthostatic symptoms, bradycardia, and, in one case in a healthy volunteer, transient sinus arrest with syncope [see Warnings and Precautions (5.2, 5.3)].
The mechanism of orthostatic hypotension induced by ropinirole is presumed to be due to a D2-mediated blunting of the noradrenergic response to standing and subsequent decrease in peripheral vascular resistance. Nausea is a common concomitant symptom of orthostatic signs and symptoms.
At oral doses as low as 0.2 mg, ropinirole suppressed serum prolactin concentrations in healthy male volunteers.
Immediate-release ropinirole had no dose-related effect on electrocardiogram wave form and rhythm in young, healthy, male volunteers in the range of 0.01 to 2.5 mg.
Immediate-release ropinirole had no dose- or exposure-related effect on mean QTc intervals in healthy male and female volunteers titrated to doses up to 4 mg/day. The effect of ropinirole on QTc intervals at higher exposures achieved either due to drug interactions, hepatic impairment, or at higher doses has not been systematically evaluated.
12.3 Pharmacokinetics
Increase in systemic exposure of ropinirole following oral administration of 2 to 12 mg of ropinirole extended-release tablets was approximately dose proportional. For ropinirole extended-release tablets, steady-state concentrations of ropinirole are expected to be achieved within 4 days of dosing. 
 
Absorption
In clinical trials with immediate-release ropinirole,  more than 88% of a radiolabeled dose was recovered in urine, and the absolute bioavailability was 45% to 55%, indicating approximately 50% first-pass effect.
The bioavailability of ropinirole extended-release tablets is similar to that of immediate-release ropinirole tablets. In a repeat-dose trial in subjects with Parkinson’s disease using ropinirole extended-release tablets 8 mg, the dose-normalized AUC(0-24) and Cmin for ropinirole extended-release tablets and immediate-release ropinirole were similar. Dose-normalized Cmax was, on average, 12% lower for ropinirole extended-release tablets than for the immediate-release formulation and the median time to peak concentration was 6 to 10 hours. In a single-dose trial, administration of ropinirole extended-release tablets to healthy volunteers with food (i.e., high-fat meal) increased AUC by approximately 30% and Cmax by approximately 44% compared with dosing under fasted conditions. In a repeat-dose trial in patients with Parkinson’s disease, food (i.e., high-fat meal) increased AUC by approximately 20% and Cmax by approximately 44%; Tmax was prolonged by 3 hours (median prolongation) compared with dosing under fasted conditions [see Dosage and Administration (2)].
 
Distribution
Ropinirole is widely distributed throughout the body, with an apparent volume of distribution of 7.5 L/kg. It is up to 40% bound to plasma proteins and has a blood-to-plasma ratio of 1:1.
Metabolism
Ropinirole is extensively metabolized by the liver. The major metabolic pathways are N-despropylation and hydroxylation to form the inactive N-despropyl metabolite and hydroxy metabolites. The N-despropyl metabolite is converted to carbamyl glucuronide, carboxylic acid, and N-despropyl hydroxy metabolites. The hydroxy metabolite of ropinirole is rapidly glucuronidated.
In vitro studies indicate that the major cytochrome P450 enzyme involved in the metabolism of ropinirole is CYP1A2, an enzyme known to be induced by smoking and omeprazole and inhibited by, for example, fluvoxamine, mexiletine, and the older fluoroquinolones such as ciprofloxacin and norfloxacin.
Elimination
The clearance of ropinirole after oral administration is 47 L/h and its elimination half-life is approximately 6 hours. Less than 10% of the administered dose is excreted as unchanged drug in urine. N-despropyl ropinirole is the predominant metabolite found in urine (40%), followed by the carboxylic acid metabolite (10%) and the glucuronide of the hydroxy metabolite (10%).
Specific Populations  
Because therapy with ropinirole extended-release tablets is initiated at a low dose and gradually titrated upward according to clinical tolerability to obtain the optimum therapeutic effect, adjustment of the initial dose based on gender, weight, or age is not necessary.
 
Geriatric Patients: Oral clearance of ropinirole is reduced by 15% in patients older than 65 years compared with younger patients. Dosage adjustment is not necessary in the elderly (older than 65 years), as the dose of ropinirole is to be individually titrated to clinical response.
Male and Female Patients: Male and female patients showed similar clearance. 
 
Racial or Ethnic Groups:  The influence of race on the pharmacokinetics of ropinirole has not been evaluated.
 
Cigarette Smoking: Smoking is expected to increase the clearance of ropinirole since CYP1A2 is known to be induced by smoking. In a trial in patients with Restless Legs Syndrome, smokers (n = 7) had an approximately 30% lower Cmax and a 38% lower AUC than did nonsmokers (n = 11) when those parameters were normalized for dose. 
 
Patients with Renal Impairment: Based on population pharmacokinetic analysis, no difference was observed in the pharmacokinetics of ropinirole in subjects with moderate renal impairment (creatinine clearance between 30 to 50 mL/min) compared with an age-matched population with creatinine clearance above 50 mL/min. Therefore, no dosage adjustment is necessary in patients with moderate renal impairment.
A trial of immediate-release ropinirole in subjects with end-stage renal disease on hemodialysis has shown that clearance of ropinirole was reduced by approximately 30%. The recommended maximum dose is lower in these patients [see Dosage and Administration (2.2)].
The use of ropinirole in subjects with severe renal impairment (creatinine clearance <30 mL/min) without regular dialysis has not been studied. 
 
Patients with Hepatic Impairment: The pharmacokinetics of ropinirole have not been studied in patients with hepatic impairment. Because ropinirole is extensively metabolized by the liver, these patients may have higher plasma levels and lower clearance of ropinirole than patients with normal hepatic function. 
 
Other Diseases: Population pharmacokinetic analysis revealed no change in the clearance of ropinirole in patients with concomitant diseases such as hypertension, depression, osteoporosis/arthritis, and insomnia compared with patients with Parkinson’s disease only.
Drug Interaction Studies
Digoxin: Coadministration of immediate-release ropinirole (2 mg 3 times daily) with digoxin (0.125 to 0.25 mg once daily) did not alter the steady-state pharmacokinetics of digoxin in 10 patients.
Theophylline: Administration of theophylline (300 mg twice daily), a substrate of CYP1A2, did not alter the steady-state pharmacokinetics of immediate-release ropinirole (2 mg 3 times daily) in 12 patients with Parkinson’s disease. Immediate-release ropinirole (2 mg 3 times daily) did not alter the pharmacokinetics of theophylline (5 mg/kg intravenously) in 12 patients with Parkinson’s disease.
Ciprofloxacin: Coadministration of ciprofloxacin (500 mg twice daily), an inhibitor of CYP1A2, with immediate-release ropinirole (2 mg 3 times daily) increased ropinirole AUC by 84% on average and Cmax by 60% (n = 12 patients).
Estrogens: Population pharmacokinetic analysis revealed that estrogens (mainly ethinylestradiol: intake 0.6 to 3 mg over 4-month to 23-year period) reduced the oral clearance of ropinirole by 36% in 16 patients.
L-dopa: Coadministration of carbidopa + L-dopa (10/100 mg twice daily) with immediate-release ropinirole (2 mg 3 times daily) had no effect on the steady-state pharmacokinetics of ropinirole (n = 28 patients). Oral administration of immediate-release ropinirole 2 mg 3 times daily increased mean steady-state Cmax of L-dopa by 20%, but its AUC was unaffected (n = 23 patients).
Commonly Administered Drugs: Population analysis showed that commonly administered drugs (e.g., selegiline, amantadine, tricyclic antidepressants, benzodiazepines, ibuprofen, thiazides, antihistamines, anticholinergics) did not affect the clearance of ropinirole. An in vitro study indicates that ropinirole is not a substrate for P-glycoprotein. Ropinirole and its circulating metabolites do not inhibit or induce P450 enzymes; therefore, ropinirole is unlikely to affect the pharmacokinetics of other drugs by a P450 mechanism.
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Two-year carcinogenicity studies of ropinirole were conducted in mice at oral doses of 0, 5, 15, and 50 mg/kg/day and in rats at oral doses of 0, 1.5, 15, and 50 mg/kg/day.
In rats, there was an increase in testicular Leydig cell adenomas at all doses tested. The lowest dose tested (1.5 mg/kg/day) is less than the MRHD  (24 mg/day) on a mg/m2 basis. The endocrine mechanisms believed to be involved in the production of these tumors in rats are not considered relevant to humans.
In mice, there was an increase in benign uterine endometrial polyps at a dose of 50 mg/kg/day. The highest dose not associated with this finding (15 mg/kg/day) is 3  times the MRHD on a mg/m2 basis.
Mutagenesis
Ropinirole was not mutagenic or clastogenic in in vitro (Ames, chromosomal aberration in human lymphocytes, mouse lymphoma tk) assays, or in the in vivo mouse micronucleus test.
Impairment of Fertility
When administered to female rats prior to and during mating and throughout pregnancy, ropinirole caused disruption of implantation at oral doses of 20 mg/kg/day (8 times the MRHD on a mg/m2 basis) or greater. This effect in rats is thought to be due to the prolactin-lowering effect of ropinirole. In rat studies using a low oral dose (5 mg/kg) during the prolactin-dependent phase of early pregnancy (gestation days 0 to 8), ropinirole did not affect female fertility at oral doses up to 100 mg/kg/day (40 times the MRHD on a mg/m2 basis). No effect on male fertility was observed in rats at oral doses up to 125 mg/kg/day (50 times the MRHD on a mg/m2 basis).
14 Clinical Studies
The effectiveness of ropinirole was initially established with the immediate-release formulation (ropinirole tablets) for the treatment of early and advanced Parkinson’s disease in 3 randomized, double-blind, placebo-controlled trials. 
The effectiveness of ropinirole extended-release tablets in the treatment of Parkinson’s disease was supported by 2 randomized, double-blind, multicenter, flexible-dose clinical trials and clinical pharmacokinetic considerations. One trial conducted in patients with advanced Parkinson’s disease compared ropinirole extended-release tablets with placebo as adjunctive therapy to L-dopa (Study 1). A second trial compared ropinirole extended-release tablets with ropinirole tablets in patients with early Parkinson’s disease not receiving L-dopa (Study 3). Ropinirole extended-release tablets has also been evaluated in 2 postmarketing, randomized, double-blind, multicenter, fixed-dose, dose-response clinical trials conducted in advanced and early Parkinson’s disease patients (Study 2 and Study 4, respectively). 
In these trials a variety of measures were used to assess the effects of treatment (e.g., Unified Parkinson‚Äôs Disease Rating Scale [UPDRS] scores,¬†patient diaries recording time ‚Äúon‚ÄĚ and ‚Äúoff,‚ÄĚ tolerability of L-dopa dose reductions). The UPDRS is a multi-li rating scale intended to evaluate mentation (Part I), activities of daily living (Part II), motor performance (Part III), and complications of therapy (Part IV). Part III of the UPDRS contains 14 lis designed to assess the severity of the cardinal motor findings in patients with Parkinson‚Äôs disease (e.g., tremor, rigidity, bradykinesia, postural instability) scored for different body regions and has a maximum (worst) score of 108.
14.1 Trials in Patients with Advanced Parkinson's Disease (with L-dopa)
Study 1 (Flexible-Dose Trial)
The effectiveness of ropinirole extended-release tablets as adjunctive therapy to L-dopa in patients with Parkinson‚Äôs disease was established in a 24-week, randomized, double-blind, placebo-controlled, parallel-group, flexible-dose, clinical trial in 393 patients (Hoehn & Yahr criteria Stages II-IV) who were not adequately controlled by L-dopa therapy. Patients were allowed to be on concomitant selegiline, amantadine, anticholinergics, and catechol-O-methyltransferase¬†inhibitors provided the doses were stable for at least 4 weeks prior to screening and throughout the trial. The primary efficacy endpoint evaluated was the mean change from baseline in total awake time spent ‚Äúoff‚ÄĚ.
Patients in this trial had a mean disease duration of 8.6 years, had a mean duration of exposure to L-dopa of 6.5 years, had experienced a minimum of 3 hours' awake time ‚Äúoff‚ÄĚ with a baseline average of approximately 7 hours' awake time ‚Äúoff‚ÄĚ, and had a mean baseline UPDRS motor score of approximately 30 points. The mean baseline dose of L-dopa was 824 mg/day in the group receiving ropinirole extended-release tablets and 776 mg/day¬†in the placebo group. Patients initiated treatment at 2 mg/day for 1 week, followed by increases of 2 mg/day at weekly intervals, to a minimum dose of 6 mg/day. The following week, the total daily dose of ropinirole extended-release tablets could be further increased (based upon therapeutic response and tolerability) to 8 mg/day. Once a daily dose of 8 mg/day was reached, the background L-dopa dosage was reduced. Thereafter, the daily dose could be increased by up to 4 mg/day approximately every 2 weeks until an optimal dose was achieved (based upon therapeutic response and tolerability). The mean dose of ropinirole extended-release tablets at the end of Week 24 was 18.8 mg/day. Dose titrations were based upon the degree of symptom control, planned L-dopa dosage reduction, and/or tolerability. The maximum allowed daily dosage for ropinirole extended-release tablets was 24 mg/day.
The primary efficacy endpoint was mean change from baseline in total awake time spent ‚Äúoff‚ÄĚ at Week 24. At baseline, the mean total awake time spent ‚Äúoff‚ÄĚ was approximately 7 hours in each treatment group. At Week 24, the total awake time spent ‚Äúoff‚ÄĚ, on average, had decreased by approximately 2 hours in the group receiving ropinirole extended-release tablets and by approximately one-half hour in the placebo group. The adjusted mean difference in total awake time spent ‚Äúoff‚ÄĚ between ropinirole extended-release tablets and placebo was -1.7 hours, which was statistically significant (analysis of covariance [ANCOVA], P<0.0001). Results for this endpoint, showing the statistical superiority of ropinirole extended-release tablets over placebo, are presented in Table 5.
Table 5. Change from Baseline in Total Awake Time Spent ‚ÄúOff‚ÄĚ (Primary Efficacy Endpoint) at Week 24 (Study 1)
 
Ropinirole Extended-Release Tablets ¬† (n = 201)¬† Placebo (n = 190)¬† Mean ‚Äúoff‚ÄĚ time at baseline (h) 7 7 Mean change from baseline in ‚Äúoff‚ÄĚ time (h) -2.1 -0.4 Treatment difference (Ropinirole Extended-Release Tablets ‚Äď PLACEBO) ¬† ¬† -1.7¬†
The difference between groups in favor of ropinirole extended-release tablets, with regard to a decrease in total ‚Äúoff‚ÄĚ hours, was primarily related to an increase in total ‚Äúon‚ÄĚ hours without troublesome dyskinesia. Patients treated with ropinirole extended-release tablets had a mean reduction in L-dopa dose of 278 mg/day (34%), while patients treated with placebo had a mean reduction of 164 mg/day (21%). In patients who reduced their L-dopa dose, reduction was sustained in 93% of patients treated with ropinirole extended-release tablets and in 72% of patients treated with placebo (P<0.001).
 
Study 2 (Fixed-Dose, Dose-Response Trial)  
A double-blind, placebo-controlled, fixed-dose, parallel-group trial evaluated the dose response of ropinirole extended-release tablets as adjunctive therapy to L-dopa in 352 randomized patients with advanced Parkinson‚Äôs disease (Hoehn & Yahr criteria Stages II-IV) over a total dosing period of 18 weeks. Patients initiated treatment with placebo or ropinirole extended-release tablets¬†at 2 mg/day for 1 week, and increased to a target dose of 4, 8, 12, 16, or 24 mg/day over a 13-week up-titration period. The dose remained stable over an additional 4-week maintenance period, followed by a 1-week down-titration period. The L-dopa dose was kept constant during the study, if possible. The primary efficacy endpoint was the mean change from baseline in total awake time spent ‚Äúoff‚ÄĚ at Week 4 of the maintenance period with daily doses of 4, 8, 12, 16, and 24 mg compared with placebo. The primary statistical analysis of the primary efficacy endpoint was Mixed Model Repeated Measures (MMRM).
At baseline, the mean ‚Äúoff‚ÄĚ time ranged from 5.6 to 6.5 hours across groups on ropinirole extended-release tablets and placebo. Table 6 shows the results for the primary efficacy endpoint. The greatest treatment difference (Ropinirole Extended-Release Tablets ‚Äď PLACEBO) for the primary efficacy endpoint was observed with the 8-mg dose; however, higher doses were not shown to provide additional benefit.
 
Table 6. Change from Baseline in Total Awake Time Spent ‚ÄúOff‚ÄĚ (Primary Efficacy Endpoint) at the End of the Maintenance Period (Study 2)
 
Endpoint¬† Daily Ropinirole Extended-Release Tablets Dose Placebo N = 65¬† 4 mg N = 21¬† 8 mg N = 60¬† 12 mg N = 61¬† 16 mg N = 65¬† 24 mg N = 25¬† Least squares mean change from baseline for ‚Äúoff‚ÄĚ time -1.91 -2.04 -2.92 -2.34 -2.80 -2.37 Treatment difference (Ropinirole Extended-Release Tablets ‚Äď PLACEBO) ¬† -0.13 -1.01 -0.43 -0.89 -0.46 P value a ¬† 0.81 0.01 0.29 0.03 0.39
a P value not adjusted for multiple comparisons. A hierarchical step-down approach for statistical testing was used starting with 16-mg dose.
14.2 Trials in Patients with Early Parkinson's Disease (without L-dopa)
Study 3 (Flexible-Dose Trial)
A 36-week, multicenter, double-blind, titration/3-period maintenance, flexible-dose, crossover trial compared the efficacy of ropinirole extended-release tablets with the immediate-release formulation of ropinirole tablets in 161 patients with early phase Parkinson’s disease (Hoehn & Yahr Stages I-III) with limited prior exposure to L-dopa or dopamine agonists. Eligible patients were randomized (1:1:1:1) to 4 treatment sequences (2 were titrated on immediate-release formulation of ropinirole tablets and 2 on ropinirole extended-release tablets). Titration rate of immediate-release formulation of ropinirole tablets was slower than that of the ropinirole extended-release tablets. Patients were titrated during the 12-week titration period to their optimal dosage, based upon tolerance and therapeutic response. This was followed by 3 consecutive 8-week maintenance periods, during which patients were either maintained on the prior formulation or switched to the alternative formulation. All switches were performed overnight by using the approximately equivalent doses of ropinirole. The primary efficacy endpoint was the change of UPDRS motor score within each maintenance period.
Patients in all 4 groups started out with similar UPDRS motor scores (about 21) at baseline. All groups exhibited similar improvement in UPDRS total motor scores from baseline until the completion of the titration phase, with a change in score of about -9 observed for the groups started on immediate-release formulation of ropinirole tablets and of about -10 for the groups started on ropinirole extended-release tablets. No difference was observed between groups when switches were made between identical formulations or between different formulations. This suggests therapeutic dosage equivalence between the immediate-release formulation of ropinirole tablets and ropinirole extended-release tablets.
The optimal daily dose at the end of the titration period for patients on immediate-release formulation of ropinirole tablets was substantially lower (mean: 7 mg) compared with the dose at the end of the titration period for patients on ropinirole extended-release tablets (mean: 18 mg). In this trial, the marked difference in the final optimal dosages suggests that the higher doses afforded no additional benefit when compared with the lower doses [see Dosage and Administration (2.2)].
Study 4 (Fixed-Dose, Dose-Response Trial)
A double-blind, placebo-controlled, fixed-dose, parallel-group trial evaluated the dose response of ropinirole extended-release tablets without L-dopa in 186 randomized patients with early Parkinson’s disease (Hoehn & Yahr Stages I-III) over a total dosing period of 18 weeks. Patients initiated treatment with placebo or ropinirole extended-release tablets at 2 mg/day for 1 week and were either maintained at a target dose of 2 mg/day or further increased to a target dose of 4, 8, 12, or 24 mg/day over a 13-week up-titration period. The dose remained stable over an additional 4-week maintenance period, followed by a 1-week down-titration period. The primary statistical analysis of the primary efficacy endpoint was Mixed Model Repeated Measures (MMRM).
The primary efficacy endpoint was the change from baseline in UPDRS motor score at Week 4 of the maintenance period with daily doses of 2, 4, 8, 12, and 24 mg compared with placebo. At baseline, the mean UPDRS motor score ranged from approximately 21 to 25 across all groups receiving ropinirole extended-release tablets and placebo. Table 7 shows results for the primary efficacy endpoint. The greatest treatment difference (Ropinirole Extended-Release Tablets ‚Äď PLACEBO) for the primary efficacy endpoint occurred with the 12-mg dose. At Week 4 of the maintenance period, the primary efficacy analysis (MMRM) did not show a significant difference between placebo (mean adjusted change: -3.98) and any dose of ropinirole extended-release tablets (mean adjusted changes ranged from -4.09 to -6.14). Data were also analyzed by nonparametric ANCOVA as pre-specified because of non-normality. This analysis and showed that there was a significant reduction from baseline in the UPDRS motor score for the group receiving ropinirole extended-release tablets¬†12 mg/day (P = 0.047); however, higher doses were not shown to provide additional benefit.
Table 7. Change from Baseline in Unified Parkinson’s Disease Rating Scale (UPDRS) Part III Motor Score (Primary Efficacy Endpoint) at the End of the Maintenance Period (Study 4)
Endpoint Daily Ropinirole Extended-Release Tablets Dose Placebo N = 35 2 mg N = 13 4 mg N = 35 8 mg N = 33 12 mg N = 34 24 mg N = 10 Least square mean change from baseline in UPDRS Part III motor score -3.98 -4.09 -4.97 -5.90 -6.14 -4.85 Treatment difference (Ropinirole Extended-Release Tablets ‚Äď PLACEBO) ¬† -0.11 -0.99 -1.92 -2.16 -0.87 P value a ¬† 0.95 0.48 0.18 0.13 0.68
a P value not adjusted for multiple comparisons. A hierarchical step-down approach for statistical testing was used starting with 12-mg dose.
16 How Supplied/storage And Handling
Each capsule shaped, film coated tablet contains ropinirole hydrochloride equivalent to the labeled amount of ropinirole as follows:
2 mg: pink tablets debossed with ‚ÄėL191‚Äô
NDC 62332-107-30                bottle of 30 tablets
NDC 62332-107-90                bottle of 90 tablets
NDC 62332-107-31                bottle of 100 tablets
NDC 62332-107-71                bottle of 500 tablets
NDC 62332-107-91                bottle of 1000 tablets
NDC 62332-107-10                carton of 100 (10X10) unit dose tablets
4 mg: light brown tablets debossed with ‚ÄėL193‚Äô
NDC 62332-108-30                bottle of 30 tablets
NDC 62332-108-90                bottle of 90 tablets
NDC 62332-108-31                bottle of 100 tablets
NDC 62332-108-71                bottle of 500 tablets
NDC 62332-108-91                bottle of 1000 tablets
NDC 62332-108-10                carton of 100 (10X10) unit dose tablets
6 mg: white to off white tablets debossed with ‚ÄėL321‚Äô
NDC 62332-109-30                bottle of 30 tablets
NDC 62332-109-90                bottle of 90 tablets
NDC 62332-109-31                bottle of 100 tablets
NDC 62332-109-71                bottle of 500 tablets
NDC 62332-109-91                bottle of 1000 tablets
NDC 62332-109-10                carton of 100 (10X10) unit dose tablets
8 mg: dark brown to red tablets debossed with ‚ÄėL194‚Äô
NDC 62332-110-30                bottle of 30 tablets
NDC 62332-110-90                bottle of 90 tablets
NDC 62332-110-31                bottle of 100 tablets
NDC 62332-110-71                bottle of 500 tablets
NDC 62332-110-91                bottle of 1000 tablets
NDC 62332-110-10                carton of 100 (10X10) unit dose tablets
12 mg: light green tablets debossed with ‚ÄėL195‚Äô
NDC 62332-111-30                bottle of 30 tablets
NDC 62332-111-90                bottle of 90 tablets
NDC 62332-111-31                bottle of 100 tablets
NDC 62332-111-71                bottle of 500 tablets
NDC 62332-111-91                bottle of 1000 tablets
NDC 62332-111-10                carton of 100 (10X10) unit dose tablets
  
Storage
Store at 20¬į to 25¬įC (68¬į to 77¬įF). [See USP Controlled Room Temperature.]
Dispense in a tight, light-resistant container as defined in the USP.
17 Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Dosing Instructions
Instruct patients to take ropinirole extended-release tablets only as prescribed. If a dose is missed, advise patients not to double their next dose. Ropinirole extended-release tablets can be taken with or without food. Inform patients to swallow ropinirole extended-release tablets whole and not to chew, crush, or divide the tablets [see Dosage and Administration (2.1)].
Ropinirole is the active ingredient in both ropinirole extended-release tablets and ropinirole tablets (the immediate-release formulation). Ask your patients if they are taking another medication containing ropinirole.
Hypersensitivity/Allergic Reactions
Advise patients about the potential for developing a hypersensitivity/allergic reaction including manifestations such as urticaria, angioedema, rash, and pruritus when taking any ropinirole product. Inform patients who experience these or similar reactions after starting ropinirole tablets or ropinirole extended-release tablets, to immediately contact their healthcare professional [see Contraindications (4)].
Falling Asleep during Activities of Daily Living and Somnolence
Alert patients to the potential sedating effects caused by ropinirole extended-release tablets, including somnolence and the possibility of falling asleep while engaged in activities of daily living. Because somnolence is a frequent adverse reaction with potentially serious consequences, patients should not drive a car, operate machinery, or engage in other potentially dangerous activities until they have gained sufficient experience with ropinirole extended-release tablets to gauge whether or not it adversely  affects their mental and/or motor performance.  Advise patients that if increased somnolence or episodes of falling asleep during activities of daily living (e.g., conversations, eating, driving a motor vehicle) are experienced at any time during treatment, they should not drive or participate in potentially dangerous activities until they have contacted their physician.
Advise patients of possible additive effects when patients are taking other sedating medications, alcohol, or other central nervous system depressants (e.g., benzodiazepines, antipsychotics, antidepressants) in combination with ropinirole extended-release tablets or when taking a concomitant medication (e.g., ciprofloxacin) that increases plasma levels of ropinirole [see Warnings and Precautions (5.1)].
Syncope and Hypotension/Orthostatic Hypotension
Advise patients that they may experience syncope and may develop hypotension with or without symptoms such as dizziness, nausea, syncope, and sometimes sweating while taking ropinirole extended-release tablets, especially if they are elderly. Hypotension and/or orthostatic symptoms may occur more frequently during initial therapy or with an increase in dose at any time (cases have been seen after weeks of treatment). Postural/orthostatic symptoms may be related to sitting up or standing. Accordingly, caution patients against standing rapidly after sitting or lying down, especially if they have been doing so for prolonged periods and especially at the initiation of treatment with ropinirole extended-release tablets[see Warnings and Precautions (5.2, 5.3)].
Elevation of Blood Pressure and Changes in Heart Rate
Alert patients to the possibility of increases in blood pressure during treatment with ropinirole extended-release tablets. Exacerbation of hypertension may occur. Medication dose adjustment may be necessary if elevation of blood pressure is sustained over multiple evaluations. Alert patients with cardiovascular disease who may not tolerate marked changes in heart rate to the possibility that they may experience significant increases or decreases in heart rate during treatment with ropinirole extended-release tablets[see Warnings and Precautions (5.4)].
Hallucinations/Psychotic-Like Behavior Inform patients that they may experience hallucinations (unreal visions, sounds, or sensations), and  that other psychotic-like behavior can occur while taking ropinirole extended-release tablets. In patients with Parkinson’s disease, the elderly are at greater risk than younger patients. This risk is greater in patients who are taking ropinirole extended-release tablets with L-dopa or taking higher doses of ropinirole extended-release tablets, and may also be further increased in patients taking any other drugs that increase dopaminergic tone. Tell patients to report hallucinations or psychotic-like behavior to their healthcare provider promptly should they develop [see Warnings and Precautions (5.5)].
Dyskinesia Inform patients that ropinirole extended-release tablets may cause and/or exacerbate pre-existing dyskinesias [see Warnings and Precautions (5.6)].
Impulse Control/ Compulsive Behaviors
Advise patients that they may experience impulse control and/or compulsive behaviors while taking ropinirole extended-release tablets. Advise patients to inform their physician or healthcare provider if they develop new or increased gambling urges, sexual urges, uncontrolled spending, binge or compulsive eating, or other urges while being treated with ropinirole extended-release tablets. Physicians should consider dose reduction or stopping the medication if a patient develops such urges while taking ropinirole extended-release tablets[see Warnings and Precautions (5.7)].
Withdrawal-Emergent Hyperpyrexia and Confusion
Advise patients to contact their healthcare provider if they wish to discontinue ropinirole extended-release tablets or decrease the dose of ropinirole extended-release tablets. Advise patients who have been prescribed a lower dose or who have been withdrawn from the drug to notify their healthcare provider if they present with fever, muscular rigidity, or altered consciousness [see Warnings and Precautions (5.8)].
Withdrawal Symptoms
Advise patients that withdrawal symptoms may occur during or after discontinuation or dose reduction of ropinirole extended-release tablets. Advise patients who have been prescribed a lower dose or who have been withdrawn from the drug to notify their healthcare provider if they have withdrawal symptoms such as apathy, anxiety, depression, fatigue, insomnia, sweating, or pain. Notify patients that in case of severe withdrawal symptoms, a trial re-administration of a dopamine agonist at the lowest effective dose may be considered [see Warnings and Precautions (5.9)].
  
Nursing Mothers
Because of the possibility that ropinirole may be excreted in breast milk, discuss the developmental and health benefits of breastfeeding along with the mother’s clinical need for ropinirole extended-release tablets and any potential adverse effects on the breastfed child from ropinirole or from the underlying maternal condition [see Use in Specific Populations (8.2)]. Advise patients that ropinirole extended-release tablets could inhibit lactation because ropinirole inhibits prolactin secretion.
Pregnancy
Because experience with ropinirole in pregnant women is limited and ropinirole has been shown to have adverse effects on embryofetal development in animals, including teratogenic effects,  advise patients of this potential risk. Advise patients to notify their physician if they become pregnant or intend to become pregnant during therapy [see Use in Specific Populations (8.1)].
Patient Information
Ropinirole (roe PIN i role) Extended-Release Tablets
 Important Note: Ropinirole extended-release tablets have not been studied in RLS and are not approved for the treatment of RLS. However, an immediate-release form of ropinirole is approved for the treatment of moderate to severe primary RLS.
What is the most important information I should know about ropinirole extended-release tablets? Ropinirole extended-release tablets can cause serious side effects including: ‚Äʬ†Falling asleep during normal activities. You may fall asleep while doing normal activities such as driving a car, doing physical tasks, or using hazardous machinery while taking ropinirole extended-release tablets. You may suddenly fall asleep without being drowsy or without warning. This may result in having accidents. Your chances of falling asleep while doing normal activities while taking ropinirole extended-release tablets are greater if you take other medicines that cause drowsiness. Tell your healthcare provider right away if this happens. Before starting ropinirole extended-release tablets, be sure to tell your healthcare provider if you take any medicines that make you drowsy. ‚Äʬ†Fainting. Fainting can happen, and sometimes your heart rate may be decreased. This can happen especially when you start taking ropinirole extended-release tablets or your dose is increased. Tell your healthcare provider if you faint, feel dizzy or feel light-headed. ‚Äʬ†Decrease in blood pressure. Ropinirole extended-release tablets can decrease your blood pressure (hypotension),¬† especially when you start taking ropinirole extended-release tablets or when your dose is changed. If you faint or feel dizzy, nauseated, or sweaty when you stand up from sitting or lying down (orthostatic hypotension), this may mean that your blood pressure is decreased. When you change position from lying down or sitting to standing up, you should do it carefully and slowly. Call your healthcare provider if you have any of the symptoms of decreased blood pressure uled above. ‚Äʬ†Increase in blood pressure. Ropinirole extended-release tablets may increase your blood pressure. ‚Äʬ†Changes in heart rate (decrease or increase). Ropinirole extended-release tablets can decrease or increase your heart rate. ‚Äʬ†Hallucinations and other psychotic-like behavior. Ropinirole extended-release tablets can cause or worsen psychotic-like behavior including hallucinations (seeing or hearing things that are not real), confusion, excessive suspicion, aggressive behavior, agitation, delusional beliefs (believing things that are not real), and disorganized thinking. The chances of having hallucinations or these other psychotic-like changes are higher in people with Parkinson‚Äôs disease who are taking ropinirole extended-release tablets or taking higher doses of these drugs. If you have hallucinations or any of these other psychotic-like changes, talk with your healthcare provider.¬† ‚ÄĘUncontrolled sudden movements. Ropinirole extended-release tablets may cause uncontrolled sudden movements or make such movements you already have worse or more frequent. Tell your healthcare provider if this happens. The doses of your anti-Parkinson‚Äôs medicines may need to be changed. ‚ÄĘUnusual urges. Some patients taking ropinirole extended-release tablets get urges to behave in a way unusual for them. Examples of this are an unusual urge to gamble, increased sexual urges and behaviors, or an uncontrollable urge to shop, spend money, or eat. If you notice or your family notices that you are developing any unusual behaviors, talk to your healthcare provider.
‚Äʬ†Withdrawal Symptoms. Ropinirole extended-release tablets are dopamine agonist medicines. Dopamine agonist medicines, including ropinirole extended-release tablets, can cause withdrawal symptoms as your dose is slowly lowered (tapered) or when treatment with ropinirole extended-release tablets is stopped. Tell your doctor right away if you get any of the following withdrawal symptoms:
o fever                                 o fatigue
o confusion                          o sweating
o severe muscle stiffness    o pain
o insomnia                           o feeling like you do not care about things you usually care about (apathy)
o anxiety
After you have stopped taking ropinirole extended-release tablets, your healthcare provider may need to restart you at a low dose of ropinirole extended-release tablets if you get severe withdrawal symptoms.
What are ropinirole extended-release tablets? Ropinirole extended-release tablets are long-acting prescription medicine containing ropinirole (taken 1 time a day) that is used only to treat Parkinson’s disease but not to treat Restless Legs Syndrome (RLS). Having one of these conditions does not mean you have or will develop the other condition. You should not be taking more than 1 medicine containing ropinirole. Tell your healthcare provider if you are taking any other medicine containing ropinirole. It is not known if ropinirole extended-release tablets are safe and effective for use in children younger than 18 years of age.
Do not take ropinirole extended-release tablets if you: ‚Äʬ†are allergic to ropinirole or any of the ingredients in ropinirole extended-release tablets. See the end of this page for a complete ul of the ingredients in ropinirole extended-release tablets. ‚Äʬ†Get help right away if any of the symptoms of an allergic reaction cause problems swallowing or breathing. Call your healthcare provider if you have any of the¬† symptoms of an allergic reaction. Symptoms of an allergic reaction may include:
¬†‚Äʬ†hives ‚Äʬ†rash¬†¬† ¬†‚Äʬ†swelling of the face, lips, mouth, tongue, or throat ¬†‚Äʬ†itching
Before¬†taking ropinirole extended-release tablets, tell your healthcare provider about all of your medical conditions, including if you: ‚Äʬ†have daytime sleepiness from a sleep disorder or have unexpected or unpredictable sleepiness or periods of sleep. ‚Äʬ†start or stop taking other medicines while you are taking ropinirole extended-release tablets. This may increase your chances of getting side effects. ‚Äʬ†start or stop smoking while you are taking ropinirole extended-release tablets. Smoking may decrease the treatment effect of ropinirole extended-release tablets. ‚Äʬ†feel dizzy, nauseated, sweaty, or faint when you first stand up from sitting or lying down. ‚Äʬ†drink alcoholic beverages. This may increase your chances of becoming drowsy or sleepy while taking ropinirole extended-release tablets. ‚Äʬ†have high or low blood pressure. ‚Äʬ†have or have had heart problems. ‚Äʬ†are pregnant or plan to become pregnant. It is not known if ropinirole extended-release tablets can harm your unborn baby. ‚Äʬ†are breastfeeding or plan to breastfeed. It is not known if ropinirole passes into your breast milk. The amount of breast milk you make may be decreased while taking ropinirole extended-release tablets. Talk to your healthcare provider to decide if you should breastfeed while taking ropinirole extended-release tablets. Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Some of these medicines may increase your chances of getting side effects while taking ropinirole extended-release tablets.
How should I take ropinirole extended-release tablets ? ‚Äʬ†Take ropinirole extended-release tablets exactly as directed by your healthcare provider. ‚Äʬ†Take ropinirole extended-release tablets with or without food. ‚Äʬ†Do not suddenly stop taking ropinirole extended-release tablets without talking to your healthcare provider. If you stop this medicine, you may develop withdrawal symptoms (See ‚ÄúWhat is the most important information I should know about ropinirole extended-release tablets?‚ÄĚ) ‚Äʬ†Before starting ropinirole extended-release tablets, you should talk to your healthcare provider about what to do if you miss a dose. If you have missed the previous dose and it is time for your next dose, do not double the dose. ‚Äʬ†Your healthcare provider will start you on a low dose of ropinirole extended-release tablets. Your healthcare provider will change the dose until you are taking the right amount of medicine to control your symptoms. It may take several weeks before you reach a dose that controls your symptoms. ‚Äʬ†Contact your healthcare provider if you stop taking ropinirole extended-release tablets for any reason. Do not restart without talking with your healthcare provider. ‚Äʬ†Your healthcare provider may prescribe ropinirole extended-release tablets alone, or add ropinirole extended-release tablets to medicine that you are already taking for Parkinson‚Äôs disease. ‚Äʬ†You should not substitute immediate-release ropinirole tablets for ropinirole extended-release tablets or ropinirole extended-release tablets for immediate-release ropinirole tablets without talking with your healthcare provider. If you are taking ropinirole extended-release tablets: ‚Äʬ†Take ropinirole extended-release tablets 1 time each day for Parkinson‚Äôs disease, preferably at or around the same time of day. ‚Äʬ†Swallow ropinirole extended-release tablets whole. Do not chew, crush, or split ropinirole extended-release tablets. ‚Äʬ†Ropinirole extended-release tablets release drug over a 24-hour period. If you have a condition where medicine passes through your body too quickly, such as diarrhea, the tablet(s) may not dissolve completely and you may see tablet residue in your stool. If this happens, let your healthcare provider know as soon as possible. What are the possible side effects of ropinirole extended-release tablets? Ropinirole extended-release tablets can cause serious side effects, including: ‚Äʬ†See ‚ÄúWhat is the most important information I should know about ropinirole extended-release tablets?‚ÄĚ The most common side effects of ropinirole extended-release tablets include:
‚Äʬ†fainting¬† ‚Äʬ†sleepiness or drowsiness ‚Äʬ†hallucinations (seeing or hearing things that are not real)¬† ‚Äʬ†dizziness¬† ¬†‚Äʬ†nausea or vomiting ¬†‚Äʬ†uncontrolled sudden movements ¬†‚Äʬ†upset stomach, abdominal pain or discomfort ¬†‚Äʬ†fatigue, tiredness, or weakness ¬†‚Äʬ†confusion ¬†‚Äʬ†headache ¬†‚Äʬ†leg swelling ¬†‚Äʬ†increased sweating ¬†‚Äʬ†constipation ¬†‚Äʬ†suddenly falling asleep ¬†‚Äʬ†high blood pressure (hypertension) ¬†
Tell your healthcare provider about any side effect that bothers you or that does not go away.
These are not all of the possible side effects with ropinirole extended-release tablets.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. How should I store ropinirole extended-release tablets? ‚Äʬ†Store ropinirole extended-release tablets at room temperature between¬† 68¬į F¬†and 77¬įF (20¬į¬†and 25¬įC). ‚Äʬ†Keep ropinirole extended-release tablets in a tightly closed container and out of direct sunlight. Keep ropinirole extended-release tablets and all medications out of the reach of children.
General information about the safe and effective use of ropinirole extended-release tablets. Medicines are sometimes prescribed for purposes other than those uled in a Patient Information leaflet. Do not use  ropinirole extended-release tablets for a condition for which it was not prescribed. Do not give ropinirole extended-release tablets to other people, even if they have the same symptoms that you have. It may harm them.  You can ask your pharmacist  or healthcare provider for information about ropinirole extended-release tablets that is written for health professionals. What are the ingredients in ropinirole extended-release tablets? Active ingredient: ropinirole (as ropinirole hydrochloride) Inactive ingredients: carboxymethylcellulose sodium, colloidal silicon dioxide, hydrogenated castor oil, hypromellose, magnesium stearate, povidone, pregelatinized starch, ethylcellulose and one or more of the following: FD&C Blue No. 2 aluminum lake, ferric oxides (black, red, yellow), polyethylene glycol 6000, polyethylene glycol 8000, titanium dioxide, talc. For more information call Alembic Pharmaceuticals Limited at 1-866-210-9797. This Patient Information has been approved by the U.S. Food and Drug Administration. Medication Guide available at http://www.alembicusa.com/medicationguide.aspx or call 1-866-210-9797.
Manufactured by: Alembic Pharmaceuticals Limited (Formulation Division), Panelav 389350, Gujarat, India
Manufactured for: Alembic Pharmaceuticals, Inc.
Bedminster, NJ 07921, USA
Revised: 08/2021
Package Label.principal Display Panel - 2mg
NDC 62332-107-30 rOPINIRole Extended-Release Tablets 2 mg* PHARMACIST: Dispense the accompanying Patient Information Leaflet to each patient. Rx only 30 Tablets
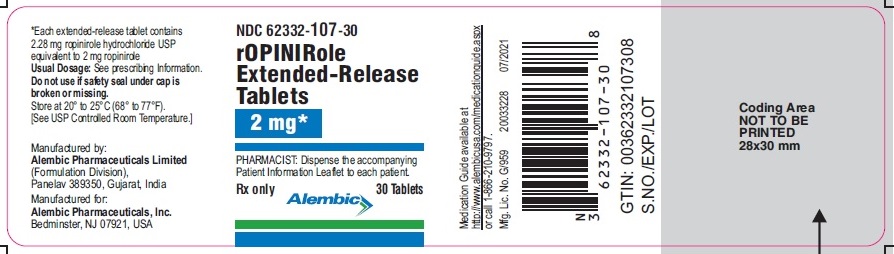
Package Label.principal Display Panel - 4mg
NDC 62332-108-30 rOPINIRole Extended-Release Tablets  4  mg* PHARMACIST: Dispense the accompanying Patient Information Leaflet to each patient. Rx only 30 Tablets
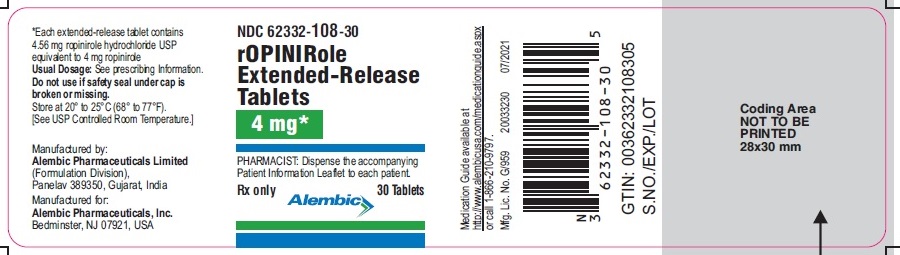
Package Label.principal Display Panel - 6mg
NDC 62332-109-30 rOPINIRole Extended-Release Tablets  6  mg* PHARMACIST: Dispense the accompanying Patient Information Leaflet to each patient. Rx only 30 Tablets
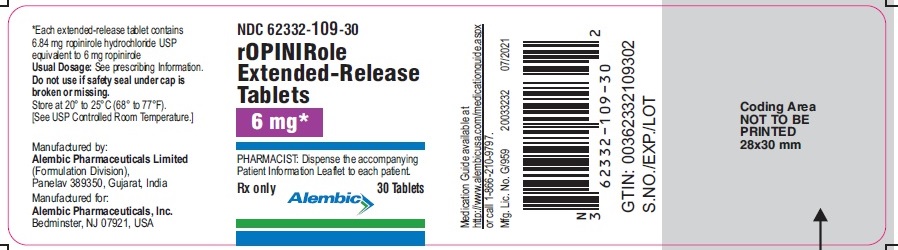
Package Label.principal Display Panel - 8mg
NDC 62332-110-30 rOPINIRole Extended-Release Tablets  8  mg* PHARMACIST: Dispense the accompanying Patient Information Leaflet to each patient. Rx only 30 Tablets
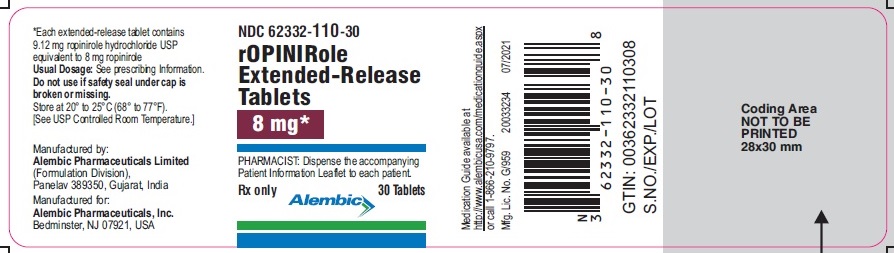
Package Label.principal Display Panel - 12mg
NDC 62332-111-30 rOPINIRole Extended-Release Tablets  12  mg* PHARMACIST: Dispense the accompanying Patient Information Leaflet to each patient. Rx only 30 Tablets
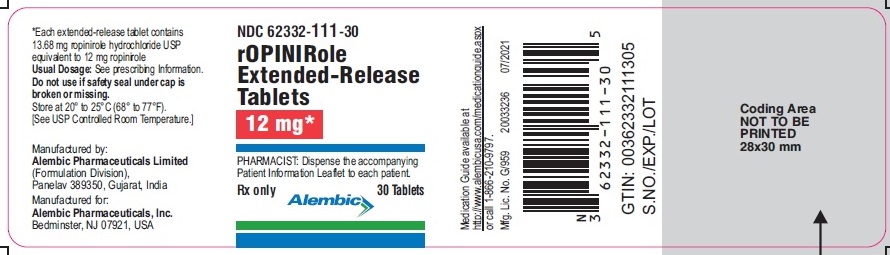
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site