NEXIUM (esomeprazole magnesium 40 mg) Dailymed
Generic: esomeprazole magnesium is used for the treatment of Duodenal Ulcer Esophagitis Gastroesophageal Reflux Heartburn Stomach Ulcer Zollinger-Ellison Syndrome Helicobacter Infections
Go PRO for all pill images
Recent Major Changes
Indications and Usage, Treatment of GERD (1.1) 12/2011
Dosage and Administration (2) 12/2011
Warnings and Precautions 06/2011
Hypomagnesemia (5.6)
Warnings and Precautions 06/2011
Concomitant use of NEXIUM with St Johnâs Wort or Rifampin (5.7)
Interactions with Diagnostic Investigations for Neuroendocrine Tumors (5.8)
1 Indications And Usage
NEXIUM is a proton pump inhibitor indicated for the following:
Treatment of gastroesophageal reflux disease (GERD) (1.1)
Risk reduction of NSAID-associated gastric ulcer (1.2)
H. pylori eradication to reduce the risk of duodenal ulcer recurrence (1.3)
Pathological hypersecretory conditions, including Zollinger-Ellison syndrome (1.4)
1.1 Treatment of Gastroesophageal Reflux Disease (GERD)
Healing of Erosive Esophagitis
NEXIUM is indicated for the short-term treatment (4 to 8 weeks) in the healing and symptomatic resolution of diagnostically confirmed erosive esophagitis. For those patients who have not healed after 4 to 8 weeks of treatment, an additional 4 to 8 week course of NEXIUM may be considered.
In infants 1 month to less than 1 year, NEXIUM is indicated for short-term treatment (up to 6 weeks) of erosive esophagitis due to acid-mediated GERD.
Maintenance of Healing of Erosive Esophagitis
NEXIUM is indicated to maintain symptom resolution and healing of erosive esophagitis. Controlled studies do not extend beyond 6 months.
Symptomatic Gastroesophageal Reflux Disease
NEXIUM is indicated for short-term treatment (4 to 8 weeks) of heartburn and other symptoms associated with GERD in adults and children 1 year or older.
1.2 Risk Reduction of NSAID-Associated Gastric Ulcer
NEXIUM is indicated for the reduction in the occurrence of gastric ulcers associated with continuous NSAID therapy in patients at risk for developing gastric ulcers. Patients are considered to be at risk due to their age (⥠60) and/or documented history of gastric ulcers. Controlled studies do not extend beyond 6 months.
1.3 Eradication to Reduce the Risk of Duodenal Ulcer Recurrence
Triple Therapy (NEXIUM plus amoxicillin and clarithromycin): NEXIUM, in combination with amoxicillin and clarithromycin, is indicated for the treatment of patients with H. pylori infection and duodenal ulcer disease (active or history of within the past 5 years) to eradicate H. pylori. Eradication of H. pylori has been shown to reduce the risk of duodenal ulcer recurrence [see Dosage and Administration (2) and Clinical Studies (14) ].
In patients who fail therapy, susceptibility testing should be done. If resistance to clarithromycin is demonstrated or susceptibility testing is not possible, alternative antimicrobial therapy should be instituted [see Clinical Pharmacology (12.4) and the prescribing information for clarithromycin].
1.4 Pathological Hypersecretory Conditions Including Zollinger-Ellison Syndrome
NEXIUM is indicated for the long-term treatment of pathological hypersecretory conditions, including Zollinger-Ellison Syndrome.
2 Dosage And Administration
NEXIUM is supplied as delayed-release capsules for oral administration or in packets for preparation of delayed-release oral suspensions. The recommended dosages are outlined in Table 1. NEXIUM should be taken at least one hour before meals.
The duration of proton pump inhibitor administration should be based on available safety and efficacy data specific to the defined indication and dosing frequency, as described in the prescribing information, and individual patient medical needs. Proton pump inhibitor treatment should only be initiated and continued if the benefits outweigh the risks of treatment
Table 1: Recommended Dosage Schedule of NEXIUM
Indication
Dose
Frequency
Gastroesophageal Reflux Disease (GERD)
Healing of Erosive Esophagitis
20 mg or 40 mg
Once Daily for 4 to 8 Weeks
Maintenance of Healing of Erosive Esophagitis
20 mg
Once DailyControlled studies did not extend beyond six months.
Symptomatic Gastroesophageal Reflux Disease
20 mg
Once Daily for 4 Weeks
Pediatric GERD
12 to 17 Year Olds
Short-term Treatment of GERD
20 mg or 40 mg
Once Daily for up to 8 Weeks
1 to 11 Year Olds
Short-term Treatment of Symptomatic GERD
10 mg
Once Daily for up to 8 Weeks
Healing of Erosive Esophagitis
weight < 20 kg
10 mg
Once Daily for 8 Weeks
weight ⥠20 kg
10 mg or 20 mg
Once Daily for 8 Weeks
1 month to < 1 year old
Erosive esophagitis due to acidmediated GERD
weight 3 kg to 5 kg
2.5 mg
Once Daily for up to 6 Weeks
weight > 5 kg to 7.5 kg
5 mg
Once Daily for up to 6 Weeks
weight >7.5 kg to 12 kg
10 mg
Once Daily for up to 6 Weeks
Risk Reduction of NSAID-Associated Gastric Ulcer
20 mg or 40 mg
Once Daily for up to 6 months
H. pylori Eradication to Reduce the Risk of Duodenal Ulcer Recurrence
Triple Therapy:
NEXIUM
40 mg
Once Daily for 10 Days
Amoxicillin
1000 mg
Twice Daily for 10 Days
Clarithromycin
500 mg
Twice Daily for 10 Days
Pathological Hypersecretory Conditions Including Zollinger-Ellison Syndrome
40 mg
Twice Daily
Please refer to amoxicillin and clarithromycin prescribing information for Contraindications, Warnings, and dosing in elderly and renally-impaired patients.
Special Populations
Hepatic Insufficiency
In patients with mild to moderate liver impairment (Child Pugh Classes A and B), no dosage adjustment is necessary. For patients with severe liver impairment (Child Pugh Class C), a dose of 20 mg of NEXIUM should not be exceeded [see Clinical Pharmacology (12.3)].
Directions for use specific to the route and available methods of administration for each of these dosage forms are presented in Table 2.
Table 2: Administration Options
Administration Options
(See text following table for additional instructions.)
Type Route Options
Delayed-Release Capsules
Oral
Capsule can be swallowed whole.
-or-
Capsule can be opened and mixed with applesauce.
Delayed-Release Capsules
Nasogastric Tube
Capsule can be opened and the intact granules emptied into a syringe and delivered through the nasogastric tube.
For Delayed-Release Oral Suspension
Oral
For the 2.5 mg and 5 mg strengths, mix the contents of packet with 5 mL of water, leave 2 to 3 minutes to thicken, stir and drink within 30 minutes.
For the 10 mg, 20 mg and 40 mg strengths, mix contents of packet with 15 mL of water, and follow the instructions above.
For Delayed-Release Oral Suspension
Nasogastric or Gastric Tube
For the 2.5 mg and 5 mg strengths, add 5 mL of water to a syringe and then add contents of packet. Shake the syringe; leave 2 to 3 minutes to thicken. Shake the syringe and inject through the nasogastric or gastric tube within 30 minutes.
For the 10 mg, 20 mg and 40 mg strengths, add 15 mL of water, and follow the instructions above.
NEXIUM Delayed-Release Capsules
NEXIUM Delayed-Release Capsules should be swallowed whole.
Alternatively, for patients who have difficulty swallowing capsules, one tablespoon of applesauce can be added to an empty bowl and the NEXIUM Delayed-Release Capsule can be opened, and the granules inside the capsule carefully emptied onto the applesauce. The granules should be mixed with the applesauce and then swallowed immediately: do not store for future use. The applesauce used should not be hot and should be soft enough to be swallowed without chewing. The granules should not be chewed or crushed. If the granules/applesauce mixture is not used in its entirety, the remaining mixture should be discarded immediately.
For patients who have a nasogastric tube in place, NEXIUM Delayed-Release Capsules can be opened and the intact granules emptied into a 60 mL catheter tipped syringe and mixed with 50 mL of water. It is important to only use a catheter tipped syringe when administering NEXIUM through a nasogastric tube. Replace the plunger and shake the syringe vigorously for 15 seconds. Hold the syringe with the tip up and check for granules remaining in the tip. Attach the syringe to a nasogastric tube and deliver the contents of the syringe through the nasogastric tube into the stomach. After administering the granules, the nasogastric tube should be flushed with additional water. Do not administer the granules if they have dissolved or disintegrated.
The mixture must be used immediately after preparation.
NEXIUM For Delayed-Release Oral Suspension
NEXIUM For Delayed-Release Oral Suspension should be administered as follows:
Empty the contents of a 2.5 mg or 5 mg packet into a container containing 5 mL of water. For the 10 mg, 20 mg, and 40 mg strengths, the contents of a packet should be emptied into a container containing 15 mL of water.
Stir.
Leave 2 to 3 minutes to thicken.
Stir and drink within 30 minutes.
If any medicine remains after drinking, add more water, stir, and drink immediately.
In cases where there is a need to use two packets, they may be mixed in a similar way by adding twice the required amount of water or follow the mixing instructions provided by your pharmacist or doctor.
For patients who have a nasogastric or gastric tube in place, NEXIUM For Delayed-Release Oral Suspension can be administered as follows:
Add 5 mL of water to a catheter tipped syringe and then add the contents of a 2.5 mg or 5 mg NEXIUM packet. For the 10 mg, 20 mg, and 40 mg strengths, the volume of water in the syringe should be 15 mL. It is important to only use a catheter tipped syringe when administering NEXIUM through a nasogastric tube or gastric tube.
Immediately shake the syringe and leave 2 to 3 minutes to thicken.
Shake the syringe and inject through the nasogastric or gastric tube, French size 6 or larger, into the stomach within 30 minutes.
Refill the syringe with an equal amount of water (5 mL or 15 mL).
Shake and flush any remaining contents from the nasogastric or gastric tube into the stomach.
Indication Dose Frequency
Gastroesophageal Reflux Disease (GERD)
Adults
20 mg or 40 mg
Once daily for 4 to 8 weeks
12 to 17 years
20 mg or 40 mg
Once daily for up to 8 weeks
1 to 11 years
10 mg or 20 mg
Once daily for up to 8 weeks
1 month to less than 1 year: 2.5 mg, 5 mg or 10 mg (based on weight). Once daily, up to 6 weeks for erosive esophagitis (EE) due to acid-mediated GERD only.
Risk Reduction of NSAID-Associated Gastric Ulcer
20 mg or 40 mg
Once daily for up to 6 months
H. pylori Eradication (Triple Therapy):
NEXIUM
40 mg
Once daily for 10 days
Amoxicillin
1000 mg
Twice daily for 10 days
Clarithromycin
500 mg
Twice daily for 10 days
Pathological Hypersecretory Conditions
40 mg
Twice daily
See full prescribing information for administration options (2)
Patients with severe liver impairment-do not exceed dose of 20 mg (2)
3 Dosage Forms And Strengths
NEXIUM Delayed-Release Capsules, 20 mg - opaque, hard gelatin, amethyst colored capsules with two radial bars in yellow on the cap and NEXIUM 20 mg in yellow on the body.
NEXIUM Delayed-Release Capsules, 40 mg - opaque, hard gelatin, amethyst colored capsules with three radial bars in yellow on the cap and NEXIUM 40 mg in yellow on the body.
NEXIUM For Delayed-Release Oral Suspension, 2.5 mg, 5 mg, 10 mg, 20 mg or 40 mg - unit dose packet containing a fine yellow powder, consisting of white to pale brownish esomeprazole granules and pale yellow inactive granules.
NEXIUM Delayed-Release Capsules: 20 mg and 40 mg (3)
NEXIUM For Delayed-Release Oral Suspension: 2.5 mg, 5 mg, 10 mg, 20 mg, and 40 mg (3)
4 Contraindications
NEXIUM is contraindicated in patients with known hypersensitivity to proton pump inhibitors. Hypersensitivity reactions, e.g., angioedema and anaphylactic shock, have been reported with NEXIUM use.
Patients with known hypersensitivity to proton pump inhibitors (PPIs) (angioedema and anaphylaxis have occurred) (4)
5 Warnings And Precautions
Symptomatic response does not preclude the presence of gastric malignancy (5.1)
Atrophic gastritis has been noted with long-term omeprazole therapy (5.2)
Bone Fracture: Long-term and multiple daily dose PPI therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist or spine. (5.3)
Triple therapy for H. pylori â there are risks due to the antibiotics; see separate prescribing information for individual antibiotics (5.4, 5.5)
Hypomagnesemia has been reported rarely with prolonged treatment with PPIs (5.6)
Avoid concomitant use of NEXIUM with St Johnâs Wort or rifampin due to the potential reduction in esomeprazole levels (5.7) (7.3)
Interactions with diagnostic investigations for Neuroendocrine Tumors: Increases in intragastric pH may result in hypergastrinemia and enterochromaffin-like cell hyperplasia and increased chromogranin A levels which may interfere with diagnostic investigations for neuroendocrine tumors. (5.8, 12.2)
5.1 Concurrent Gastric Malignancy
Symptomatic response to therapy with NEXIUM does not preclude the presence of gastric malignancy.
5.2 Atrophic Gastritis
Atrophic gastritis has been noted occasionally in gastric corpus biopsies from patients treated long-term with omeprazole, of which esomeprazole is an enantiomer.
5.3 Bone Fracture
Several published observational studies suggest that proton pump inhibitor (PPI) therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist, or spine. The risk of fracture was increased in patients who received high-dose, defined as multiple daily doses, and long-term PPI therapy (a year or longer). Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated. Patients at risk for osteoporosis-related fractures should be managed according to established treatment guidelines. [see Dosage and Administration (2) and Adverse Reactions (6.2)]
5.4 Risks of Amoxicillin (as Part of Triple Therapy)
[See Warnings and Precautions in the prescribing information for amoxicillin.]
Serious and occasionally fatal hypersensitivity (anaphylactic) reactions have been reported in patients on penicillin therapy. These reactions are more apt to occur in individuals with a history of penicillin hypersensitivity and/or a history of sensitivity to multiple allergens.
There have been well documented reports of individuals with a history of penicillin hypersensitivity reactions that have experienced severe hypersensitivity reactions when treated with a cephalosporin. Before initiating therapy with any penicillin, careful inquiry should be made concerning previous hypersensitivity reactions to penicillins, cephalosporins, and other allergens. If an allergic reaction occurs, amoxicillin should be discontinued and the appropriate therapy instituted.
Serious anaphylactic reactions require immediate emergency treatment with epinephrine. Oxygen, intravenous steroids, and airway management, including intubation, should also be administered as indicated.
Pseudomembranous colitis has been reported with nearly all antibacterial agents, including clarithromycin and amoxicillin, and may range in severity from mild to life threatening. Therefore, it is important to consider this diagnosis in patients who present with diarrhea subsequent to the administration of antibacterial agents.
Treatment with antibacterial agents alters the normal flora of the colon and may permit overgrowth of clostridia. Studies indicate that a toxin produced by Clostridium difficile is a primary cause of âantibiotic-associated colitisâ.
After the diagnosis of pseudomembranous colitis has been established, therapeutic measures should be initiated. Mild cases of pseudomembranous colitis usually respond to discontinuation of the drug alone. In moderate to severe cases, consideration should be given to management with fluids and electrolytes, protein supplementation, and treatment with an antibacterial drug clinically effective against Clostridium difficile colitis.
5.5 Risks of Clarithromycin (as Part of Triple Therapy)
[See Warnings and Precautions in the prescribing information for clarithromycin]
Clarithromycin should not be used in pregnant women except in clinical circumstances where no alternative therapy is appropriate. If pregnancy occurs while taking clarithromycin, the patient should be apprised of the potential hazard to the fetus.
Concomitant administration of clarithromycin with cisapride, pimozide, astemizole, terfenadine, ergotamine, or dihydroergotamine is contraindicated.
5.6Hypomagnesemia
Hypomagnesemia, symptomatic and asymptomatic, has been reported rarely in patients treated with PPIs for at least three months, in most cases after a year of therapy. Serious adverse events include tetany, arrhythmias, and seizures. In most patients, treatment of hypomagnesemia required magnesium replacement and discontinuation of the PPI.
For patients expected to be on prolonged treatment or who take PPIs with medications such as digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), health care professionals may consider monitoring magnesium levels prior to initiation of PPI treatment and periodically. [See Adverse Reactions (6.2)]
5.7 Concomitant use of NEXIUM with St Johns Wort or rifampin
Drugs which induce CYP2C19 or CYP3A4 (such as St Johnâs Wort or rifampin) can substantially decrease esomeprazole concentrations. [see Drug Interactions (7.3) ] Avoid concomitant use of NEXIUM with St Johnâs Wort, or rifampin.
5.8 Interactions with Diagnostic Investigations for Neuroendocrine Tumors
Serum chromogranin A (CgA) levels increase secondary to drug-induced decreases in gastric acidity. The increased CgA level may cause false positive results in diagnostic investigations for neuroendocrine tumors. Providers should temporarily stop esomeprazole treatment before assessing CgA levels and consider repeating the test if initial CgA levels are high. If serial tests are performed (e.g. for monitoring), the same commercial laboratory should be used for testing, as reference ranges between tests may vary.
6 Adverse Reactions
Most common adverse reactions (6.1):
Adults (⥠18 years) (incidence ⥠1%) are headache, diarrhea, nausea, flatulence, abdominal pain, constipation, and dry mouth
Pediatric (⤠17 years) (incidence ⥠2%) are headache, diarrhea, abdominal pain, nausea, and somnolence
Pediatric (1 month to < 1 year) (incidence 1%) are abdominal pain, regurgitation, tachypnea, and increased ALT
To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca at 1-800-236-9933 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adults
The safety of NEXIUM was evaluated in over 15,000 patients (aged 18 to 84 years) in clinical trials worldwide including over 8,500 patients in the United States and over 6,500 patients in Europe and Canada. Over 2,900 patients were treated in long-term studies for up to 6-12 months. In general, NEXIUM was well tolerated in both short and long-term clinical trials.
The safety in the treatment of healing of erosive esophagitis was assessed in four randomized comparative clinical trials, which included 1,240 patients on NEXIUM 20 mg, 2,434 patients on NEXIUM 40 mg, and 3,008 patients on omeprazole 20 mg daily. The most frequently occurring adverse reactions (â¥1%) in all three groups were headache (5.5, 5, and 3.8, respectively) and diarrhea (no difference among the three groups). Nausea, flatulence, abdominal pain, constipation, and dry mouth occurred at similar rates among patients taking NEXIUM or omeprazole.
Additional adverse reactions that were reported as possibly or probably related to NEXIUM with an incidence < 1% are uled below by body system:
Body as a Whole: abdomen enlarged, allergic reaction, asthenia, back pain, chest pain, substernal chest pain, facial edema, peripheral edema, hot flushes, fatigue, fever, flu-like disorder, generalized edema, leg edema, malaise, pain, rigors;
Cardiovascular: flushing, hypertension, tachycardia;
Endocrine: goiter;
Gastrointestinal: bowel irregularity, constipation aggravated, dyspepsia, dysphagia, dysplasia GI, epigastric pain, eructation, esophageal disorder, frequent stools, gastroenteritis, GI hemorrhage, GI symptoms not otherwise specified, hiccup, melena, mouth disorder, pharynx disorder, rectal disorder, serum gastrin increased, tongue disorder, tongue edema, ulcerative stomatitis, vomiting;
Hearing: earache, tinnitus;
Hematologic: anemia, anemia hypochromic, cervical lymphadenopathy, epistaxis, leukocytosis, leukopenia, thrombocytopenia;
Hepatic: bilirubinemia, hepatic function abnormal, SGOT increased, SGPT increased;
Metabolic/Nutritional: glycosuria, hyperuricemia, hyponatremia, increased alkaline phosphatase, thirst, vitamin B12 deficiency, weight increase, weight decrease;
Musculoskeletal: arthralgia, arthritis aggravated, arthropathy, cramps, fibromyalgia syndrome, hernia, polymyalgia rheumatica;
Nervous System/Psychiatric: anorexia, apathy, appetite increased, confusion, depression aggravated, dizziness, hypertonia, nervousness, hypoesthesia, impotence, insomnia, migraine, migraine aggravated, paresthesia, sleep disorder, somnolence, tremor, vertigo, visual field defect;
Reproductive: dysmenorrhea, menstrual disorder, vaginitis;
Respiratory: asthma aggravated, coughing, dyspnea, larynx edema, pharyngitis, rhinitis, sinusitis;
Skin and Appendages: acne, angioedema, dermatitis, pruritus, pruritus ani, rash, rash erythematous, rash maculo-papular, skin inflammation, sweating increased, urticaria;
Special Senses: otitis media, parosmia, taste loss, taste perversion;
Urogenital: abnormal urine, albuminuria, cystitis, dysuria, fungal infection, hematuria, micturition frequency, moniliasis, genital moniliasis, polyuria;
Visual: conjunctivitis, vision abnormal.
The following potentially clinically significant laboratory changes in clinical trials, irrespective of relationship to NEXIUM, were reported in ⤠1% of patients: increased creatinine, uric acid, total bilirubin, alkaline phosphatase, ALT, AST, hemoglobin, white blood cell count, platelets, serum gastrin, potassium, sodium, thyroxine and thyroid stimulating hormone [see Clinical Pharmacology (12)]. Decreases were seen in hemoglobin, white blood cell count, platelets, potassium, sodium, and thyroxine.
Endoscopic findings that were reported as adverse reactions include: duodenitis, esophagitis, esophageal stricture, esophageal ulceration, esophageal varices, gastric ulcer, gastritis, hernia, benign polyps or nodules, Barrettâs esophagus, and mucosal discoloration.
The incidence of treatment-related adverse reactions during 6-month maintenance treatment was similar to placebo. There were no differences in types of related adverse reactions seen during maintenance treatment up to 12 months compared to short-term treatment.
Two placebo-controlled studies were conducted in 710 patients for the treatment of symptomatic gastroesophageal reflux disease. The most common adverse reactions that were reported as possibly or probably related to NEXIUM were diarrhea (4.3%), headache (3.8%), and abdominal pain (3.8%).
Pediatrics
The safety of NEXIUM was evaluated in 316 pediatric and adolescent patients aged 1 to 17 years in four clinical trials for the treatment of symptomatic GERD [see Clinical Studies (14.2) ]. In 109 pediatric patients aged 1 to 11 years, the most frequently reported (at least 1%) treatment-related adverse reactions in these patients were diarrhea (2.8%), headache (1.9%) and somnolence (1.9%). In 149 pediatric patients aged 12 to 17 years the most frequently reported (at least 2%) treatment-related adverse reactions in these patients were headache (8.1%), abdominal pain (2.7%), diarrhea (2%), and nausea (2%).
The safety of NEXIUM was evaluated in 167 pediatric patients from birth to <1 year of age in three clinical trials. [See Clinical Studies (14.6) ] In a study that included 26 pediatric patients aged birth to 1 month there were no treatment related adverse reactions. In a study that included 43 pediatric patients age 1 to 11 months, inclusive the most frequently reported (at least 5%) adverse reactions, irrespective of causality, were irritability and vomiting. In a study that included 98 pediatric patients, age 1 to 11 months, inclusive exposed to esomeprazole for up to 6 weeks (including 39 patients randomized to the withdrawal phase), there were 4 treatment-related adverse reactions: abdominal pain (1%), regurgitation (1%), tachypnea (1%), and increased ALT (1%).
No new safety concerns were identified in pediatric patients.
Combination Treatment with Amoxicillin and Clarithromycin
In clinical trials using combination therapy with NEXIUM plus amoxicillin and clarithromycin, no additional adverse reactions specific to these drug combinations were observed. Adverse reactions that occurred were limited to those observed when using NEXIUM, amoxicillin, or clarithromycin alone.
The most frequently reported drug-related adverse reactions for patients who received triple therapy for 10 days were diarrhea (9.2%), taste perversion (6.6%), and abdominal pain (3.7%). No treatment-emergent adverse reactions were observed at higher rates with triple therapy than were observed with NEXIUM alone.
For more information on adverse reactions with amoxicillin or clarithromycin, refer to their package inserts, Adverse Reactions sections.
In clinical trials using combination therapy with NEXIUM plus amoxicillin and clarithromycin, no additional increased laboratory abnormalities particular to these drug combinations were observed.
For more information on laboratory changes with amoxicillin or clarithromycin, refer to their package inserts, Adverse Reactions section.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of NEXIUM. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These reports are uled below by body system:
Blood And Lymphatic: agranulocytosis, pancytopenia;
Eye: blurred vision;
Gastrointestinal: pancreatitis, stomatitis;
Hepatobiliary: hepatic failure, hepatitis with or without jaundice;
Immune System: anaphylactic reaction/shock;
Infections and Infestations: GI candidiasis;
Metabolism and nutritional disorders: hypomagnesemia
Musculoskeletal and Connective Tissue: muscular weakness, myalgia, bone fracture;
Nervous System: hepatic encephalopathy, taste disturbance;
Psychiatric: aggression, agitation, depression, hallucination;
Renal and Urinary: interstitial nephritis;
Reproductive System and Breast: gynecomastia;
Respiratory, Thoracic, and Mediastinal: bronchospasm;
Skin and Subcutaneous Tissue: alopecia, erythema multiforme, hyperhidrosis, photosensitivity, Stevens-Johnson syndrome, toxic epidermal necrolysis (some fatal).
7 Drug Interactions
May affect plasma levels of antiretroviral drugs â use with atazanavir and nelfinavir is not recommended; if saquinavir is used with NEXIUM, monitor for toxicity and consider saquinavir dose reduction (7.1)
May interfere with drugs for which gastric pH affects bioavailability (e.g., ketoconazole, iron salts, and digoxin). Patients treated with NEXIUM and digoxin may need to be monitored for digoxin toxicity. (7.2)
Combined inhibitor of CYP 2C19 and 3A4 may raise esomeprazole levels (7.3)
May increase systemic exposure of cilostazol and an active metabolite. Consider dose reduction (7.3)
Tacrolimus: NEXIUM may increase serum levels of tacrolimus (7.4)
7.1 Interference with Antiretroviral Therapy
Concomitant use of atazanavir and nelfinavir with proton pump inhibitors is not recommended. Co-administration of atazanavir with proton pump inhibitors is expected to substantially decrease atazanavir plasma concentrations and may result in a loss of therapeutic effect and the development of drug resistance. Co-administration of saquinavir with proton pump inhibitors is expected to increase saquinavir concentrations, which may increase toxicity and require dose reduction.
Omeprazole, of which esomeprazole is an enantiomer, has been reported to interact with some antiretroviral drugs. The clinical importance and the mechanisms behind these interactions are not always known. Increased gastric pH during omeprazole treatment may change the absorption of the antiretroviral drug. Other possible interaction mechanisms are via CYP 2C19.
Reduced concentrations of atazanavir and nelfinavir
For some antiretroviral drugs, such as atazanavir and nelfinavir, decreased serum levels have been reported when given together with omeprazole. Following multiple doses of nelfinavir (1250 mg, twice daily) and omeprazole (40 mg daily), AUC was decreased by 36% and 92%, Cmax by 37% and 89% and Cmin by 39% and 75% respectively for nelfinavir and M8. Following multiple doses of atazanavir (400 mg, daily) and omeprazole (40 mg, daily, 2 hr before atazanavir), AUC was decreased by 94%, Cmax by 96%, and Cmin by 95%. Concomitant administration with omeprazole and drugs such as atazanavir and nelfinavir is therefore not recommended.
Increased concentrations of saquinavir
For other antiretroviral drugs, such as saquinavir, elevated serum levels have been reported, with an increase in AUC by 82%, in Cmax by 75%, and in Cmin by 106%, following multiple dosing of saquinavir/ritonavir (1000/100 mg) twice daily for 15 days with omeprazole 40 mg daily co-administered days 11 to 15. Therefore, clinical and laboratory monitoring for saquinavir toxicity is recommended during concurrent use with NEXIUM. Dose reduction of saquinavir should be considered from the safety perspective for individual patients.
There are also some antiretroviral drugs of which unchanged serum levels have been reported when given with omeprazole.
7.2 Drugs for Which Gastric pH Can Affect Bioavailability
Esomeprazole inhibits gastric acid secretion. Therefore, esomeprazole may interfere with the absorption of drugs where gastric pH is an important determinant of bioavailability (e.g., ketoconazole, atazanavir, iron salts, and digoxin). Concomitant treatment with omeprazole (20 mg daily) and digoxin in healthy subjects increased the bioavailability of digoxin by 10% (30% in two subjects). Esomeprazole is an enantiomer of omeprazole. Coadministration of digoxin with esomeprazole is expected to increase the systemic exposure of digoxin. Therefore, patients may need to be monitored when digoxin is taken concomitantly with esomeprazole.
7.3 Effects on Hepatic Metabolism/Cytochrome P-450 Pathways
Esomeprazole is extensively metabolized in the liver by CYP 2C19 and CYP 3A4. In vitro and in vivo studies have shown that esomeprazole is not likely to inhibit CYPs 1A2, 2A6, 2C9, 2D6, 2E1, and 3A4. No clinically relevant interactions with drugs metabolized by these CYP enzymes would be expected. Drug interaction studies have shown that esomeprazole does not have any clinically significant interactions with phenytoin, warfarin, quinidine, clarithromycin, or amoxicillin.
However, post-marketing reports of changes in prothrombin measures have been received among patients on concomitant warfarin and esomeprazole therapy. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. Patients treated with proton pump inhibitors and warfarin concomitantly may need to be monitored for increases in INR and prothrombin time.
Esomeprazole may potentially interfere with CYP 2C19, the major esomeprazole metabolizing enzyme. Coadministration of esomeprazole 30 mg and diazepam, a CYP 2C19 substrate, resulted in a 45% decrease in clearance of diazepam.
Omeprazole acts as an inhibitor of CYP 2C19. Omeprazole, given in doses of 40 mg daily for one week to 20 healthy subjects in cross-over study, increased Cmax and AUC of cilostazol by 18% and 26% respectively. Cmax and AUC of one of its active metabolites, 3,4-dihydrocilostazol, which has 4-7 times the activity of cilostazol, were increased by 29% and 69% respectively. Co-administration of cilostazol with esomeprazole is expected to increase concentrations of cilostazol and its above mentioned active metabolite. Therefore a dose reduction of cilostazol from 100 mg twice daily to 50 mg twice daily should be considered.
Concomitant administration of esomeprazole and a combined inhibitor of CYP 2C19 and CYP 3A4, such as voriconazole, may result in more than doubling of the esomeprazole exposure. Dose adjustment of esomeprazole is not normally required. However, in patients with Zollinger-Ellisonâs Syndrome, who may require higher doses up to 240 mg/day, dose adjustment may be considered.
Drugs known to induce CYP2C19 or CYP3A4 or both (such as rifampin) may lead to decreased esomeprazole serum levels. Omeprazole, of which esomeprazole is an enantiomer, has been reported to interact with St. Johnâs wort an inducer of CYP3A4. In a cross-over study in 12 healthy male subjects, St Johnâs wort (300 mg three times daily for 14 days) significantly decreased the systemic exposure of omeprazole in CYP2C19 poor metabolisers (Cmax and AUC decreased by 37.5% and 37.9%, respectively) and extensive metabolisers (Cmax and AUC decreased by 49.6 % and 43.9%, respectively). Avoid concomitant use of St. Johnâs Wort or rifampin with NEXIUM.
7.4 Interactions With Investigations of Neuroendocrine Tumors
Drug-induced decrease in gastric acidity results in enterochromaffin-like cell hyperplasia and increased Chromogranin A levels which may interfere with investigations for neuroendocrine tumors. [see Warnings and Precautions (5.7) and Clinical Pharmacology (12.2) ]
7.5 Tacrolimus
Concomitant administration of esomeprazole and tacrolimus may increase the serum levels of tacrolimus.
7.6 Combination Therapy with Clarithromycin
Co-administration of esomeprazole, clarithromycin, and amoxicillin has resulted in increases in the plasma levels of esomeprazole and 14-hydroxyclarithromycin [see Clinical Pharmacology (12.4) ].
Concomitant administration of clarithromycin with cisapride, pimozide, astemizole, terfenadine, ergotamine, or dihydroergotamine is contraindicated [see prescribing information for clarithromycin].
8 Use In Specific Populations
8.1 Pregnancy
Pregnancy Category B
Reproductive studies in rats and rabbits with NEXIUM (esomeprazole) and multiple cohort studies in pregnant women with omeprazole use during the first trimester do not show an increased risk of congenital anomalies or adverse pregnancy outcomes. There are, however, no adequate and well controlled studies of NEXIUM use in pregnancy. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Esomeprazole is the s-isomer of omeprazole. In four population-based cohort studies that included 1226 women exposed during the first trimester of pregnancy to omeprazole there was no increased risk of congenital anomalies.
Reproductive studies with esomeprazole have been performed in rats at doses up to 57 times the human dose and in rabbits at doses up to 35 times the human dose and have revealed no evidence of impaired fertility or harm to the fetus. [ See Animal Toxicology and/or Pharmacology (13.2)]
Reproductive studies conducted with omeprazole on rats at oral doses up to 56 times the human dose and in rabbits at doses up to 56 times the human dose did not show any evidence of teratogenicity. In pregnant rabbits, omeprazole at doses about 5.5 to 56 times the human dose produced dose-related increases in embryo-lethality, fetal resorptions, and pregnancy loss. In rats treated with omeprazole at doses about 5.6 to 56 times the human dose, dose-related embryo/fetal toxicity and postnatal developmental toxicity occurred in offspring.
8.3Nursing Mothers
Omeprazole concentrations have been measured in breast milk of one woman taking omeprazole 20 mg per day. However, the excretion of esomeprazole in milk has not been studied. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for tumorigenicity shown for NEXIUM in rat carcinogenicity studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4Pediatric Use
The safety and effectiveness of NEXIUM have been established in pediatric patients 1 to 17 years of age for short-term treatment (up to eight weeks) of GERD. The safety and effectiveness of NEXIUM have been established in pediatric patients 1 month to less than 1 year for short-term treatment (up to 6 weeks) of acid-mediated GERD with erosive esophagitis. However, the safety and effectiveness of NEXIUM have not been established in patients less than 1 month of age.
1 to 17 years of age
Use of NEXIUM in pediatric and adolescent patients 1 to 17 years of age for short-term treatment (up to eight weeks) of GERD is supported by extrapolation of results from adequate and well-controlled studies for adults and safety and pharmacokinetic studies performed in pediatric and adolescent patients [see Clinical Pharmacology (12.3), Dosage and Administration (2), Adverse Reactions (6.1), and Clinical Studies, (14.3) ]. The safety and effectiveness of NEXIUM for other pediatric uses have not been established.
Erosive esophagitis due to acid-mediated GERD in infants 1 month to less than one year of age
Use of NEXIUM in pediatric patients 1 month to < 1 year of age for treatment (up to 6 weeks) of acid-mediated GERD with erosive esophagitis is supported by extrapolation of results from adequate and well-controlled studies for adults and safety, pharmacokinetic, and pharmacodynamic studies performed in pediatric patients [see Clinical Pharmacology (12.3), Dosage and Administration (2), Adverse Reactions (6.1), and Clinical Studies, (14.3) ]..
Symptomatic GERD in infants 1 month to less than one year of age
There was no statistically significant difference between NEXIUM and placebo in the rate of discontinuation due to symptom worsening in a multicenter, randomized, double-blind, controlled, treatment-withdrawal study of 98 patients ages 1 to 11 months, inclusive. Patients were enrolled if they had either a clinical diagnosis of suspected GERD, symptomatic GERD, or endoscopically proven GERD. Twenty of 98 enrolled patients underwent endoscopy, and 6 patients were found to have erosive esophagitis on endoscopy at baseline. All patients received NEXIUM Delayed-Release Oral Suspension once daily during a two-week, open-label phase of the study.
There were 80 patients who attained a pre-specified level of symptom improvement and who entered the double-blind phase, in which they were randomized in equal proportions to receive NEXIUM or placebo for the next four weeks. Efficacy was assessed by observing the time from randomization to study discontinuation due to symptom worsening during the four-week, treatment-withdrawal phase.
The following pharmacokinetic and pharmacodynamic information was obtained in pediatric patients with GERD aged birth to less than one year of age. In infants (1 to 11 months old, inclusive) given NEXIUM 1 mg/kg once daily, the percent time with intragastric pH > 4 increased from 29% at baseline to 69% on Day 7, which is similar to the pharmacodynamic effect in adults [see Clinical Pharmacology (12.2) ]. Apparent clearance (CL/F) increases with age in pediatric patients from birth to 2 years of age.
Neonates 0 to 1 month of age
Following administration of oral NEXIUM in neonates the geometric mean (range) for the apparent clearance (CL/F) was 0.55 L/h/kg (0.25-1.6 L/h/kg).
The safety and effectiveness of NEXIUM in neonates have not been established.
8.5Geriatric Use
Of the total number of patients who received NEXIUM in clinical trials, 1459 were 65 to 74 years of age and 354 patients were ⥠75 years of age.
No overall differences in safety and efficacy were observed between the elderly and younger individuals, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
10 Overdosage
A single oral dose of esomeprazole at 510 mg/kg (about 103 times the human dose on a body surface area basis), was lethal to rats. The major signs of acute toxicity were reduced motor activity, changes in respiratory frequency, tremor, ataxia, and intermittent clonic convulsions.
The symptoms described in connection with deliberate NEXIUM overdose (limited experience of doses in excess of 240 mg/day) are transient. Single doses of 80 mg of esomeprazole were uneventful. Reports of overdosage with omeprazole in humans may also be relevant. Doses ranged up to 2,400 mg (120 times the usual recommended clinical dose). Manifestations were variable, but included confusion, drowsiness, blurred vision, tachycardia, nausea, diaphoresis, flushing, headache, dry mouth, and other adverse reactions similar to those seen in normal clinical experience (see omeprazole package insert - Adverse Reactions). No specific antidote for esomeprazole is known. Since esomeprazole is extensively protein bound, it is not expected to be removed by dialysis. In the event of overdosage, treatment should be symptomatic and supportive.
As with the management of any overdose, the possibility of multiple drug ingestion should be considered. For current information on treatment of any drug overdose contact a Poison Control Center at 1â800â222â1222.
11 Description
The active ingredient in the proton pump inhibitor NEXIUM® (esomeprazole magnesium) Delayed-Release Capsules for oral administration and NEXIUM (esomeprazole magnesium) For Delayed-Release Oral Suspension is bis(5-methoxy-2-[(S)-[(4-methoxy-3,5-dimethyl-2-pyridinyl)methyl]sulfinyl]-1H-benzimidazole-1-yl) magnesium trihydrate. Esomeprazole is the S-isomer of omeprazole, which is a mixture of the S- and R- isomers. (Initial U.S. approval of esomeprazole magnesium: 2001). Its molecular formula is (C17H18N3O3S)2Mg x 3 H2O with molecular weight of 767.2 as a trihydrate and 713.1 on an anhydrous basis. The structural formula is:
Figure 1
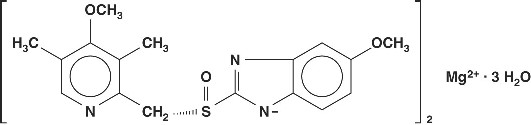
The magnesium salt is a white to slightly colored crystalline powder. It contains 3 moles of water of solvation and is slightly soluble in water. The stability of esomeprazole magnesium is a function of pH; it rapidly degrades in acidic media, but it has acceptable stability under alkaline conditions. At pH 6.8 (buffer), the half-life of the magnesium salt is about 19 hours at 25°C and about 8 hours at 37°C.
NEXIUM is supplied in delayed-release capsules and in packets for a delayed-release oral suspension. Each delayed-release capsule contains 20 mg, or 40 mg of esomeprazole (present as 22.3 mg, or 44.5 mg esomeprazole magnesium trihydrate) in the form of enteric-coated granules with the following inactive ingredients: glyceryl monostearate 40-55, hydroxypropyl cellulose, hypromellose, magnesium stearate, methacrylic acid copolymer type C, polysorbate 80, sugar spheres, talc, and triethyl citrate. The capsule shells have the following inactive ingredients: gelatin, FD&C Blue #1, FD&C Red #40, D&C Red #28, titanium dioxide, shellac, ethyl alcohol, isopropyl alcohol, n-butyl alcohol, propylene glycol, sodium hydroxide, polyvinyl pyrrolidone, and D&C Yellow #10.
Each packet of NEXIUM For Delayed-Release Oral Suspension contains 2.5 mg, 5 mg, 10 mg, 20 mg, or 40 mg of esomeprazole, in the form of the same enteric-coated granules used in NEXIUM Delayed-Release Capsules, and also inactive granules. The inactive granules are composed of the following ingredients: dextrose, xanthan gum, crospovidone, citric acid, iron oxide, and hydroxypropyl cellulose. The esomeprazole granules and inactive granules are constituted with water to form a suspension and are given by oral, nasogastric, or gastric administration.
12 Clinical Pharmacology
12.1 Mechanism of Action
Esomeprazole is a proton pump inhibitor that suppresses gastric acid secretion by specific inhibition of the H+/K+-ATPase in the gastric parietal cell. The S- and R-isomers of omeprazole are protonated and converted in the acidic compartment of the parietal cell forming the active inhibitor, the achiral sulphenamide. By acting specifically on the proton pump, esomeprazole blocks the final step in acid production, thus reducing gastric acidity. This effect is dose-related up to a daily dose of 20 to 40 mg and leads to inhibition of gastric acid secretion.
12.2 Pharmacodynamics
Antisecretory Activity
The effect of NEXIUM on intragastric pH was determined in patients with symptomatic gastroesophageal reflux disease in two separate studies. In the first study of 36 patients, NEXIUM 40 mg and 20 mg capsules were administered over 5 days. The results are shown in the Table 3:
Table 3: Effect on Intragastric pH on Day 5 (N=36)
Parameter
NEXIUM
40 mg
NEXIUM
20 mg
% Time Gastric pH >4(Hours)
70%p< 0.01 NEXIUM 40 mg vs. NEXIUM 20 mg
(16.8 h)
53%
(12.7 h)
Coefficient of variation
26%
37%
Median 24 Hour pH
4.9
4.1
Coefficient of variation
16%
27%
In a second study, the effect on intragastric pH of NEXIUM 40 mg administered once daily over a five day period was similar to the first study, (% time with pH > 4 was 68% or 16.3 hours).
Serum Gastrin Effects
The effect of NEXIUM on serum gastrin concentrations was evaluated in approximately 2,700 patients in clinical trials up to 8 weeks and in over 1,300 patients for up to 6 to 12 months. The mean fasting gastrin level increased in a dose-related manner. This increase reached a plateau within two to three months of therapy and returned to baseline levels within four weeks after discontinuation of therapy.
Increased gastrin causes enterochromaffin-like cell hyperplasia and increased serum Chromogranin A (CgA) levels. The increased CgA levels may cause false positive results in diagnostic investigations for neuroendocrine tumors.
Enterochromaffin-like (ECL) Cell Effects
In 24-month carcinogenicity studies of omeprazole in rats, a dose-related significant occurrence of gastric ECL cell carcinoid tumors and ECL cell hyperplasia was observed in both male and female animals [see Nonclinical Toxicology (13.1) ]. Carcinoid tumors have also been observed in rats subjected to fundectomy or long-term treatment with other proton pump inhibitors or high doses of H2-receptor antagonists.
Human gastric biopsy specimens have been obtained from more than 3,000 patients treated with omeprazole in long-term clinical trials. The incidence of ECL cell hyperplasia in these studies increased with time; however, no case of ECL cell carcinoids, dysplasia, or neoplasia has been found in these patients.
In over 1,000 patients treated with NEXIUM (10, 20 or 40 mg/day) up to 6 to 12 months, the prevalence of ECL cell hyperplasia increased with time and dose. No patient developed ECL cell carcinoids, dysplasia, or neoplasia in the gastric mucosa.
Endocrine Effects
NEXIUM had no effect on thyroid function when given in oral doses of 20 or 40 mg for 4 weeks. Other effects of NEXIUM on the endocrine system were assessed using omeprazole studies. Omeprazole given in oral doses of 30 or 40 mg for 2 to 4 weeks had no effect on carbohydrate metabolism, circulating levels of parathyroid hormone, cortisol, estradiol, testosterone, prolactin, cholecystokinin, or secretin.
12.3 Pharmacokinetics
Absorption
NEXIUM Delayed-Release Capsules and NEXIUM For Delayed-Release Oral Suspension contain a bioequivalent enteric-coated granule formulation of esomeprazole magnesium. Bioequivalency is based on a single dose (40 mg) study in 94 healthy male and female volunteers under fasting condition. After oral administration peak plasma levels (Cmax) occur at approximately 1.5 hours (Tmax). The Cmax increases proportionally when the dose is increased, and there is a three-fold increase in the area under the plasma concentration-time curve (AUC) from 20 to 40 mg. At repeated once-daily dosing with 40 mg, the systemic bioavailability is approximately 90% compared to 64% after a single dose of 40 mg. The mean exposure (AUC) to esomeprazole increases from 4.32 µmol*hr/L on Day 1 to 11.2 µmol*hr/L on Day 5 after 40 mg once daily dosing.
The AUC after administration of a single 40 mg dose of NEXIUM is decreased by 43% to 53% after food intake compared to fasting conditions. NEXIUM should be taken at least one hour before meals.
The pharmacokinetic profile of NEXIUM was determined in 36 patients with symptomatic gastroesophageal reflux disease following repeated once daily administration of 20 mg and 40 mg capsules of NEXIUM over a period of five days. The results are shown in the Table 4:
Table 4: Pharmacokinetic Parameters of NEXIUM on Day 5 Following Oral Dosing for 5 Days
Parameter * (CV)
NEXIUM
40 mg
NEXIUM
20 mg
AUC (μmol*h/L)
12.6 (42%)
4.2 (59%)
Cmax (μmol/L)
4.7 (37%)
2.1 (45%)
Tmax (h)
1.6
1.6
t1/2 (h)
1.5
1.2
* Values represent the geometric mean, except the Tmax, which is the arithmetic mean; CV = Coefficient of variation
Distribution
Esomeprazole is 97% bound to plasma proteins. Plasma protein binding is constant over the concentration range of 2 to 20 μmol/L. The apparent volume of distribution at steady state in healthy volunteers is approximately 16 L.
Metabolism
Esomeprazole is extensively metabolized in the liver by the cytochrome P450 (CYP) enzyme system. The metabolites of esomeprazole lack antisecretory activity. The major part of esomeprazoleâs metabolism is dependent upon the CYP 2C19 isoenzyme, which forms the hydroxy and desmethyl metabolites. The remaining amount is dependent on CYP 3A4 which forms the sulphone metabolite. CYP 2C19 isoenzyme exhibits polymorphism in the metabolism of esomeprazole, since some 3% of Caucasians and 15 to 20% of Asians lack CYP 2C19 and are termed Poor Metabolizers. At steady state, the ratio of AUC in Poor Metabolizers to AUC in the rest of the population (Extensive Metabolizers) is approximately 2.
Following administration of equimolar doses, the S- and R-isomers are metabolized differently by the liver, resulting in higher plasma levels of the S- than of the R-isomer.
Excretion
The plasma elimination half-life of esomeprazole is approximately 1 to 1.5 hours. Less than 1% of parent drug is excreted in the urine. Approximately 80% of an oral dose of esomeprazole is excreted as inactive metabolites in the urine, and the remainder is found as inactive metabolites in the feces.
Pharmacokinetics: Combination Therapy with Antimicrobials
Esomeprazole magnesium 40 mg once daily was given in combination with clarithromycin 500 mg twice daily and amoxicillin 1000 mg twice daily for 7 days to 17 healthy male and female subjects. The mean steady state AUC and Cmax of esomeprazole increased by 70% and 18%, respectively during triple combination therapy compared to treatment with esomeprazole alone. The observed increase in esomeprazole exposure during co-administration with clarithromycin and amoxicillin is not expected to produce significant safety concerns.
The pharmacokinetic parameters for clarithromycin and amoxicillin were similar during triple combination therapy and administration of each drug alone. However, the mean AUC and Cmax for 14-hydroxyclarithromycin increased by 19% and 22%, respectively, during triple combination therapy compared to treatment with clarithromycin alone. This increase in exposure to 14-hydroxyclarithromycin is not considered to be clinically significant.
Special Populations
Geriatric
The AUC and Cmax values were slightly higher (25% and 18%, respectively) in the elderly as compared to younger subjects at steady state. Dosage adjustment based on age is not necessary.
Pediatric (1 to 11 month of age)
The pharmacokinetic parameters following repeated dose administration of 1.0 mg/kg esomeprazole in 1 to 11 month old infants are summarized in Table 5.
Table 5: Summary of PK parameters in 1 month to < 1 year Olds with GERD Following 7/8 Days of Once-Daily Oral Esomeprazole Treatment
1 month to < 1 year
Parameter
1.0 mg/kg
AUC (μmol*h/L) (n=7)Geometric mean
3.51
C,max (μmol/L) (n=15)
0.87
t½ (hours) (n=8)
0.93
tmax (hours) (n=15)
3.0
Subsequent pharmacokinetic simulation analyses showed that a dosage regimen of 2.5 mg once-daily for pediatric patients with body weight 3-5 kg, 5.0 mg once-daily for >5 to 7.5 kg and 10 mg once-daily for >7.5 to 12 kg would achieve comparable steady-state plasma exposures (AUC) to that observed after 10 mg in 1 to 11 year olds, and 20 mg in 12 to 18 year-olds as well as adults.
1 to 11 Years of Age
The pharmacokinetics of esomeprazole were studied in pediatric patients with GERD aged 1 to 11 years. Following once daily dosing for 5 days, the total exposure (AUC) for the 10 mg dose in patients aged 6 to 11 years was similar to that seen with the 20 mg dose in adults and adolescents aged 12 to 17 years. The total exposure for the 10 mg dose in patients aged 1 to 5 years was approximately 30% higher than the 10 mg dose in patients aged 6 to 11 years. The total exposure for the 20 mg dose in patients aged 6 to 11 years was higher than that observed with the 20 mg dose in 12 to 17 year-olds and adults, but lower than that observed with the 40 mg dose in 12 to 17 year-olds and adults. See Table 6.
Table 6: Summary of PK Parameters in 1 to 11 Year Olds with GERD following 5 Days of Once-Daily Oral Esomeprazole Treatment
1 to 5 Year Olds
6 to 11 Year Olds
Parameter
10 mg (N=8)
10 mg (N=7)
20 mg (N=6)
AUC (μmol*h/L)Geometric mean;
4.83
3.70
6.28
Cmax (μmol/L)
2.98
1.77
3.73
tmax (h)
1.44
1.79
1.75
t½λz (h)
0.74
0.88
0.73
Cl/F (L/h)
5.99
7.84
9.22
12 to 17 Years of Age
The pharmacokinetics of NEXIUM were studied in 28 adolescent patients with GERD aged 12 to 17 years inclusive, in a single center study. Patients were randomized to receive NEXIUM 20 mg or 40 mg once daily for 8 days. Mean Cmax and AUC values of esomeprazole were not affected by body weight or age; and more than dose-proportional increases in mean Cmax and AUC values were observed between the two dose groups in the study. Overall, NEXIUM pharmacokinetics in adolescent patients aged 12 to 17 years were similar to those observed in adult patients with symptomatic GERD. See Table 7.
Table 7: Comparison of PK Parameters in 12 to 17 Year Olds with GERD and Adults with Symptomatic GERD Following the Repeated Daily Oral Dose Administration of Esomeprazole
12 to 17 Year Olds (N=28)
Adults (N=36)
Parameter
20 mg
40 mg
20 mg
40 mg
AUC (μmol*h/L)
3.65
13.86
4.2
12.6
Cmax (μmol/L)
1.45
5.13
2.1
4.7
tmax (h)
2.00
1.75
1.6
1.6
t½λz (h)
0.82
1.22
1.2
1.5
Data presented are geometric means for AUC, Cmax and t½λz, and median value for tmax.
Gender
The AUC and Cmax values were slightly higher (13%) in females than in males at steady state. Dosage adjustment based on gender is not necessary.
Hepatic Insufficiency
The steady state pharmacokinetics of esomeprazole obtained after administration of 40 mg once daily to 4 patients each with mild (Child Pugh Class A), moderate (Child Pugh Class B), and severe (Child Pugh Class C) liver insufficiency were compared to those obtained in 36 male and female GERD patients with normal liver function. In patients with mild and moderate hepatic insufficiency, the AUCs were within the range that could be expected in patients with normal liver function. In patients with severe hepatic insufficiency the AUCs were 2 to 3 times higher than in the patients with normal liver function. No dosage adjustment is recommended for patients with mild to moderate hepatic insufficiency (Child Pugh Classes A and B). However, in patients with severe hepatic insufficiency (Child Pugh Class C) a dose of 20 mg once daily should not be exceeded [see Dosage and Administration (2)].
Renal Insufficiency
The pharmacokinetics of NEXIUM in patients with renal impairment are not expected to be altered relative to healthy volunteers as less than 1% of esomeprazole is excreted unchanged in urine.
Other pharmacokinetic observations
Coadministration of oral contraceptives, diazepam, phenytoin, or quinidine did not seem to change the pharmacokinetic profile of esomeprazole.
Studies evaluating concomitant administration of esomeprazole and either naproxen (non-selective NSAID) or rofecoxib (COX-2 selective NSAID) did not identify any clinically relevant changes in the pharmacokinetic profiles of esomeprazole or these NSAIDs.
12.4 Microbiology
NEXIUM, amoxicillin, and clarithromycin triple therapy has been shown to be active against most strains of Helicobacter pylori (H. pylori) in vitro and in clinical infections [see Indications and Usage (1) and Clinical Studies (14)].
Helicobacter pylori: Susceptibility testing of H. pylori isolates was performed for amoxicillin and clarithromycin using agar dilution methodology, and minimum inhibitory concentrations (MICs) were determined.
Pretreatment Resistance: Clarithromycin pretreatment resistance rate (MIC ⥠1 mcg/mL) to H. pylori was 15% (66/445) at baseline in all treatment groups combined. A total of > 99% (394/395) of patients had H. pylori isolates that were considered to be susceptible (MIC ⤠0.25 mcg/mL) to amoxicillin at baseline. One patient had a baseline H. pylori isolate with an amoxicillin MIC = 0.5 mcg/mL.
Clarithromycin Susceptibility Test Results and Clinical/Bacteriologic Outcomes: The baseline H. pylori clarithromycin susceptibility results and the H. pylori eradication results at the Day 38 visit are shown in the Table 8:
Table 8: Clarithromycin Susceptibility Test Results and Clinical/Bacteriological Outcomes for Triple Therapy - (Esomeprazole magnesium 40 mg once daily/amoxicillin 1000 mg twice daily/clarithromycin 500Â mg twice daily for 10 days)
Clarithromycin Pretreatment Results
H. pylori negative (Eradicated)
H. pylori positive
(Not Eradicated)
Post-treatment susceptibility results
SSusceptible (S) MIC ⤠0.25 mcg/mL, Intermediate (I) MIC = 0.5 mcg/mL, Resistant (R) MIC ⥠1.0 mcg/mL
I
R
No MIC
Susceptible182
162
4
0
2
14
Intermediate1
1
0
0
0
0
Resistant29
13
1
0
13
2
Patients not eradicated of H. pylori following NEXIUM/amoxicillin/clarithromycin triple therapy will likely have clarithromycin resistant H. pylori isolates. Therefore, clarithromycin susceptibility testing should be done, when possible. Patients with clarithromycin resistant H. pylori should not be re-treated with a clarithromycin-containing regimen.
Amoxicillin Susceptibility Test Results and Clinical/Bacteriological Outcomes:
In the NEXIUM/amoxicillin/clarithromycin clinical trials, 83% (176/212) of the patients in the NEXIUM/amoxicillin/clarithromycin treatment group who had pretreatment amoxicillin susceptible MICs (⤠0.25 mcg/mL) were eradicated of H. pylori, and 17% (36/212) were not eradicated of H. pylori. Of the 36 patients who were not eradicated of H. pylori on triple therapy, 16 had no post-treatment susceptibility test results and 20 had post-treatment H. pylori isolates with amoxicillin susceptible MICs. Fifteen of the patients who were not eradicated of H. pylori on triple therapy also had post-treatment H. pylori isolates with clarithromycin resistant MICs. There were no patients with H. pylori isolates who developed treatment emergent resistance to amoxicillin.
Susceptibility Test for Helicobacter pylori: The reference methodology for susceptibility testing of H. pylori is agar dilution MICs. One to three microliters of an inoculum equivalent to a No. 2 McFarland standard (1 x 107 - 1 x 108 CFU/mL for H. pylori) are inoculated directly onto freshly prepared antimicrobial containing Mueller-Hinton agar plates with 5% aged defibrinated sheep blood (⥠2 weeks old). The agar dilution plates are incubated at 35°C in a microaerobic environment produced by a gas generating system suitable for Campylobacter. After 3 days of incubation, the MICs are recorded as the lowest concentration of antimicrobial agent required to inhibit growth of the organism. The clarithromycin and amoxicillin MIC values should be interpreted according to the following criteria:
Table 9: Clarithromycin and Amoxicillin MIC values and interpretation
Clarithromycin MIC (mcg/mL)These are breakpoints for the agar dilution methodology and they should not be used to interpret results obtained using alternative methods.
Interpretation
⤠0.25
Susceptible (S)
0.5
Intermediate (I)
â¥1.0
Resistant (R)
Amoxicillin MIC (mcg/mL)
Interpretation
⤠0.25
Susceptible (S)
Standardized susceptibility test procedures require the use of laboratory control microorganisms to control the technical aspects of the laboratory procedures. Standard clarithromycin and amoxicillin powders should provide the following MIC values:
Table 10: MIC values
Microorganism
Antimicrobial Agent
MIC (mcg/mL)
H. pylori ATCC 43504
Clarithromycin
0.016 â 0.12 (mcg/mL)
H. pylori ATCC 43504
Amoxicillin
0.016 â 0.12 (mcg/mL)
Effects on Gastrointestinal Microbial Ecology: Decreased gastric acidity due to any means, including proton pump inhibitors, increases gastric counts of bacteria normally present in the gastrointestinal tract. Treatment with proton pump inhibitors may lead to slightly increased risk of gastrointestinal infections such as Salmonella and Campylobacter and possibly Clostridium difficile in hospitalized patients.
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
The carcinogenic potential of NEXIUM was assessed using studies of omeprazole, of which esomeprazole is an enantiomer. In two 24-month oral carcinogenicity studies in rats, omeprazole at daily doses of 1.7, 3.4, 13.8, 44, and 141 mg/kg/day (about 0.7 to 57 times the human dose of 20 mg/day expressed on a body surface area basis) produced gastric ECL cell carcinoids in a dose-related manner in both male and female rats; the incidence of this effect was markedly higher in female rats, which had higher blood levels of omeprazole. Gastric carcinoids seldom occur in the untreated rat. In addition, ECL cell hyperplasia was present in all treated groups of both sexes. In one of these studies, female rats were treated with 13.8Â mg omeprazole/kg/day (about 5.6 times the human dose on a body surface area basis) for 1 year, then followed for an additional year without the drug. No carcinoids were seen in these rats. An increased incidence of treatment-related ECL cell hyperplasia was observed at the end of 1 year (94% treated vs. 10% controls). By the second year the difference between treated and control rats was much smaller (46% vs. 26%) but still showed more hyperplasia in the treated group. Gastric adenocarcinoma was seen in one rat (2%). No similar tumor was seen in male or female rats treated for 2 years. For this strain of rat no similar tumor has been noted historically, but a finding involving only one tumor is difficult to interpret. A 78-week mouse carcinogenicity study of omeprazole did not show increased tumor occurrence, but the study was not conclusive.
Esomeprazole was negative in the Ames mutation test, in the in vivo rat bone marrow cell chromosome aberration test, and the in vivo mouse micronucleus test. Esomeprazole, however, was positive in the in vitro human lymphocyte chromosome aberration test. Omeprazole was positive in the in vitro human lymphocyte chromosome aberration test, the in vivo mouse bone marrow cell chromosome aberration test, and the in vivo mouse micronucleus test.
The potential effects of esomeprazole on fertility and reproductive performance were assessed using omeprazole studies. Omeprazole at oral doses up to 138 mg/kg/day in rats (about 56 times the human dose on a body surface area basis) was found to have no effect on reproductive performance of parental animals.
13.2 Animal Toxicology and/or Pharmacology
Reproductive Toxicology Studies
Reproductive studies have been performed in rats at oral doses up to 280 mg/kg/day (about 57 times the human dose on a body surface area basis) and in rabbits at oral doses up to 86 mg/kg/day (about 35 times the human dose on a body surface area basis) and have revealed no evidence of impaired fertility or harm to the fetus due to esomeprazole.
Reproductive studies conducted with omeprazole in rats at oral doses up to 138 mg/kg/day (about 56 times the human dose on a body surface area basis) and in rabbits at doses up to 69 mg/kg/day (about 56 times the human dose on a body surface area basis) did not disclose any evidence for a teratogenic potential of omeprazole. In rabbits, omeprazole in a dose range of 6.9 to 69.1 mg/kg/day (about 5.5 to 56 times the human dose on a body surface area basis) produced dose-related increases in embryo-lethality, fetal resorptions, and pregnancy disruptions. In rats, dose-related embryo/fetal toxicity and postnatal developmental toxicity were observed in offspring resulting from parents treated with omeprazole at 13.8 to 138.0 mg/kg/day (about 5.6 to 56 times the human dose on a body surface area basis).
14 Clinical Studies
14.1 Healing of Erosive Esophagitis
The healing rates of NEXIUM 40 mg, NEXIUM 20 mg, and omeprazole 20 mg (the approved dose for this indication) were evaluated in patients with endoscopically diagnosed erosive esophagitis in four multicenter, double-blind, randomized studies. The healing rates at Weeks 4 and 8 were evaluated and are shown in the Table 11:
Table 11: Erosive Esophagitis Healing Rate (Life-Table Analysis)
Study
No. of Patients
Treatment Groups
Week 4
Week 8
Significance Level
1
588
NEXIUM 20 mg
68.7%
90.6%
N.S.N.S. = not significant (p > 0.05)
588
Omeprazole 20 mg
69.5%
88.3%
2
654
NEXIUM 40 mg
75.9%
94.1%
p < 0.001
656
NEXIUM 20 mg
70.5%
89.9%
p < 0.05
650
Omeprazole 20 mg
64.7%
86.9%
3
576
NEXIUM 40 mg
71.5%
92.2%
N.S.
572
Omeprazole 20 mg
68.6%
89.8%
4
1216
NEXIUM 40 mg
81.7%
93.7%
p < 0.001
1209
Omeprazole 20 mg
68.7%
84.2%
In these same studies of patients with erosive esophagitis, sustained heartburn resolution and time to sustained heartburn resolution were evaluated and are shown in the Table 12:
Table 12: Sustained Resolution of Heartburn (Erosive Esophagitis Patients)
Cumulative Percent with Sustained Resolution
Study
No. of Patients
Treatment Groups
Day 14
Day 28
Significance Level
1
573
NEXIUM 20 mg
64.3%
72.7%
N.S.N.S. = not significant (p > 0.05)
555
Omeprazole 20 mg
64.1%
70.9%
2
621
NEXIUM 40 mg
64.8%
74.2%
p <0.001
620
NEXIUM 20 mg
62.9%
70.1%
N.S.
626
Omeprazole 20 mg
56.5%
66.6%
3
568
NEXIUM 40 mg
65.4%
73.9%
N.S.
551
Omeprazole 20 mg
65.5%
73.1%
4
1187
NEXIUM 40 mg
67.6%
75.1%
p <0.001
1188
Omeprazole 20 mg
62.5%
70.8%
In these four studies, the range of median days to the start of sustained resolution (defined as 7 consecutive days with no heartburn) was 5 days for NEXIUM 40 mg, 7 to 8 days for NEXIUM 20 mg and 7 to 9 days for omeprazole 20 mg.
There are no comparisons of 40 mg of NEXIUM with 40 mg of omeprazole in clinical trials assessing either healing or symptomatic relief of erosive esophagitis.
Long-Term Maintenance of Healing of Erosive Esophagitis
Two multicenter, randomized, double-blind placebo-controlled 4-arm trials were conducted in patients with endoscopically confirmed, healed erosive esophagitis to evaluate NEXIUM 40 mg (n=174), 20 mg (n=180), 10 mg (n=168) or placebo (n=171) once daily over six months of treatment.
No additional clinical benefit was seen with NEXIUM 40 mg over NEXIUM 20 mg.
The percentages of patients that maintained healing of erosive esophagitis at the various time points are shown in the Figures 2 and 3:
Figure 2: Maintenance of Healing Rates by Month (Study 177)
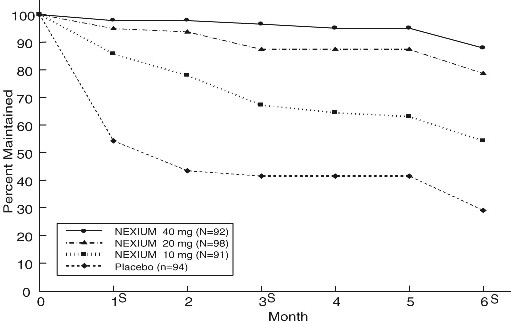
s= scheduled visit
Figure 3: Maintenance of Healing Rates by Month (Study 178)
s= scheduled visit
Patients remained in remission significantly longer and the number of recurrences of erosive esophagitis was significantly less in patients treated with NEXIUM compared to placebo.
In both studies, the proportion of patients on NEXIUM who remained in remission and were free of heartburn and other GERD symptoms was well differentiated from placebo.
In a third multicenter open label study of 808 patients treated for 12 months with NEXIUM 40 mg, the percentage of patients that maintained healing of erosive esophagitis was 93.7% for six months and 89.4% for one year.
14.2 Symptomatic Gastroesophageal Reflux Disease (GERD)
Two multicenter, randomized, double-blind, placebo-controlled studies were conducted in a total of 717 patients comparing four weeks of treatment with NEXIUM 20 mg or 40 mg once daily versus placebo for resolution of GERD symptoms. Patients had ⥠6-month history of heartburn episodes, no erosive esophagitis by endoscopy, and heartburn on at least four of the seven days immediately preceding randomization.
The percentage of patients that were symptom-free of heartburn was significantly higher in the NEXIUM groups compared to placebo at all follow-up visits (Weeks 1, 2, and 4).
No additional clinical benefit was seen with NEXIUM 40 mg over NEXIUM 20 mg.
The percent of patients symptom-free of heartburn by day are shown in the Figures 4 and 5:
Figure 4: Percent of Patients Symptom-Free of Heartburn by Day (Study 225)
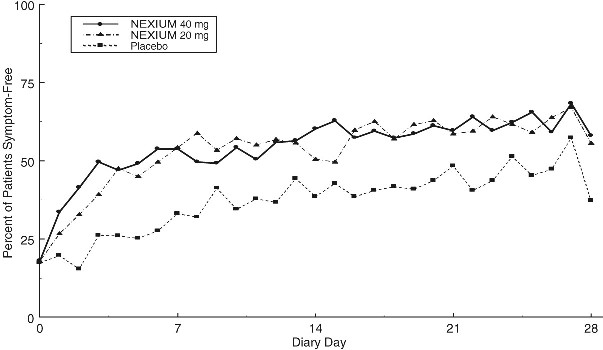
Figure 5: Percent of Patients Symptom-Free of Heartburn by Day (Study 226)
In three European symptomatic GERD trials, NEXIUM 20 mg and 40 mg and omeprazole 20 mg were evaluated. No significant treatment related differences were seen.
14.3 Pediatric Gastroesophageal Reflux Disease (GERD)
1 to 11 Years of Age
In a multicenter, parallel-group study, 109 pediatric patients with a history of endoscopically-proven GERD (1 to 11 years of age; 53 female; 89 Caucasian, 19 Black, 1 Other) were treated with NEXIUM once daily for up to 8 weeks to evaluate safety and tolerability. Dosing by patient weight was as follows:
weight < 20 kg: once daily treatment with NEXIUM 5 mg or 10 mg
weight ⥠20 kg: once daily treatment with NEXIUM 10 mg or 20 mg
Patients were endoscopically characterized as to the presence or absence of erosive esophagitis.
Of the 109 patients, 53 had erosive esophagitis at baseline (51 had mild, 1 moderate, and 1 severe esophagitis). Although most of the patients who had a follow up endoscopy at the end of 8 weeks of treatment healed, spontaneous healing cannot be ruled out because these patients had low grade erosive esophagitis prior to treatment, and the trial did not include a concomitant control.
12 to 17 Years of Age
In a multicenter, randomized, double-blind, parallel-group study, 149 adolescent patients (12 to 17 years of age; 89 female; 124 Caucasian, 15 Black, 10 Other) with clinically diagnosed GERD were treated with either NEXIUM 20 mg or NEXIUM 40 mg once daily for up to 8 weeks to evaluate safety and tolerability. Patients were not endoscopically characterized as to the presence or absence of erosive esophagitis.
14.4 Risk Reduction of NSAID-Associated Gastric Ulcer
Two multicenter, double-blind, placebo-controlled studies were conducted in patients at risk of developing gastric and/or duodenal ulcers associated with continuous use of non-selective and COX-2 selective NSAIDs. A total of 1429 patients were randomized across the 2 studies. Patients ranged in age from 19 to 89 (median age 66.0 years) with 70.7% female, 29.3% male, 82.9% Caucasian, 5.5% Black, 3.7% Asian, and 8.0% Others. At baseline, the patients in these studies were endoscopically confirmed not to have ulcers but were determined to be at risk for ulcer occurrence due to their age (â¥60 years) and/or history of a documented gastric or duodenal ulcer within the past 5 years. Patients receiving NSAIDs and treated with NEXIUM 20 mg or 40 mg once-a-day experienced significant reduction in gastric ulcer occurrences relative to placebo treatment at 26 weeks. See Table 13. No additional benefit was seen with NEXIUM 40 mg over NEXIUM 20 mg. These studies did not demonstrate significant reduction in the development of NSAID-associated duodenal ulcer due to the low incidence.
Table 13: Cumulative percentage of patients without gastric ulcers at 26 weeks:
Study
No. of Patients
Treatment Group
% of Patients Remaining Gastric Ulcer Free
1
191
194
184
NEXIUM 20 mg
NEXIUM 40 mg
Placebo
95.4
96.7
88.2
2
267
271
257
NEXIUM 20 mg
NEXIUM 40 mg
Placebo
94.7
95.3
83.3
14.5 Eradication in Patients with Duodenal Ulcer Disease
Triple Therapy (NEXIUM/amoxicillin/clarithromycin): Two multicenter, randomized, double-blind studies were conducted using a 10 day treatment regimen. The first study (191) compared NEXIUM 40 mg once daily in combination with amoxicillin 1000 mg twice daily and clarithromycin 500 mg twice daily to NEXIUM 40 mg once daily plus clarithromycin 500 mg twice daily. The second study (193) compared NEXIUM 40 mg once daily in combination with amoxicillin 1000 mg twice daily and clarithromycin 500 mg twice daily to NEXIUM 40 mg once daily. H. pylori eradication rates, defined as at least two negative tests and no positive tests from CLOtest®, histology and/or culture, at 4 weeks post-therapy were significantly higher in the NEXIUM plus amoxicillin and clarithromycin group than in the NEXIUM plus clarithromycin or NEXIUM alone group. The results are shown in table 14:
Table 14: H. pylori Eradication Rates at 4 Weeks after 10 Day Treatment Regimen % of Patients Cured [95% Confidence Interval] (Number of Patients)
Study
Treatment Group
Per-Protocol
Intent-to-Treat
191
NEXIUM plus amoxicillin and clarithromycin
84%p < 0.05 compared to NEXIUM plus clarithromycin
[78, 89]
(n=196)
77%
[71, 82]
(n=233)
NEXIUM plus clarithromycin
55%
[48, 62]
(n=187)
52%
[45, 59]
(n=215)
193
NEXIUM plus amoxicillin and clarithromycin
85%p < 0.05 compared to NEXIUM alone
[74, 93]
(n=67)
78%
[67, 87]
(n=74)
NEXIUM
5%
[0, 23]
(n=22)
4%
[0, 21]
(n=24)
The percentage of patients with a healed baseline duodenal ulcer by 4 weeks after the 10 day treatment regimen in the NEXIUM plus amoxicillin and clarithromycin group was 75% (n=156) and 57% (n=60) respectively, in the 191 and 193 studies (per-protocol analysis).
14.6 Pathological Hypersecretory Conditions Including Zollinger-Ellison Syndrome
In a multicenter, open-label dose-escalation study of 21 patients (15 males and 6 females, 18 Caucasian and 3 Black, mean age of 55.5 years) with pathological hypersecretory conditions, such as Zollinger-Ellison Syndrome, NEXIUM significantly inhibited gastric acid secretion. Initial dose was 40 mg twice daily in 19/21 patients and 80 mg twice daily in 2/21 patients. Total daily doses ranging from 80 mg to 240 mg for 12 months maintained gastric acid output below the target levels of 10 mEq/h in patients without prior gastric acid-reducing surgery and below 5 mEq/hr in patients with prior gastric acid-reducing surgery. At the Month 12 final visit, 18/20 (90%) patients had Basal Acid Output (BAO) under satisfactory control (median BAO = 0.17 mmol/hr). Of the 18 patients evaluated with a starting dose of 40 mg twice daily, 13 (72%) had their BAO controlled with the original dosing regimen at the final visit. See Table 15.
Table 15: Adequate Acid Suppression at Final Visit by Dose Regimen
NEXIUM dose at the Month 12 visit
BAO under adequate control at the Month 12 visit (N=20)
40 mg twice daily
13/15
80 mg twice daily
4/4
80 mg three times daily
1/1
16 How Supplied/storage And Handling
NEXIUM Delayed-Release Capsules, 20 mg, are opaque, hard gelatin, amethyst colored capsules with two radial bars in yellow on the cap and NEXIUM 20 mg in yellow on the body. They are supplied as follows:
Bottles of 30 NDC 54868-4635-0
NEXIUM Delayed-Release Capsules, 40 mg, are opaque, hard gelatin, amethyst colored capsules with three radial bars in yellow on the cap and NEXIUM 40 mg in yellow on the body. They are supplied as follows:
Bottles of 10 NDC 54868-4510-1 Bottles of 30 NDC 54868-4510-0 Bottles of 60 NDC 54868-4510-3 Bottles of 90 NDC 54868-4510-2
Store at 25°C (77°F); excursions permitted to 15 to 30°C (59 to 86°F). [See USP Controlled Room Temperature]. Keep NEXIUM Delayed-Release Capsules container tightly closed. Dispense in a tight container if the NEXIUM Delayed-Release Capsules product package is subdivided.
17 Patient Counseling Information
âSee FDA-Approved Patient Labeling (Patient Information)â
⢠Advise patients to let you know if they are taking, or begin taking, other medications, because NEXIUM can interfere with antiretroviral drugs and drugs that are affected by gastric pH changes [see Drug Interactions (7.1)].
⢠Let patients know that antacids may be used while taking NEXIUM.
⢠Advise patients to take NEXIUM at least one hour before a meal.
⢠For patients who are prescribed NEXIUM Delayed-Release Capsules, advise them not to chew or crush the capsules.
⢠Advise patients that, if they open NEXIUM Delayed-Release Capsules to mix the granules with food, the granules should only be mixed with applesauce. Use with other foods has not been evaluated and is not recommended.
⢠For patients who are advised to open the NEXIUM Delayed-Release Capsules before taking them or who are prescribed NEXIUM For Delayed-Release Oral Suspension, instruct them in the proper technique for administration [see Dosage and Administration (2)] and tell them to follow the dosing instructions in the PATIENT INFORMATION insert included in the package. Instruct patients to rinse the syringe with water after each use.
⢠For patients who are prescribed NEXIUM for Delayed-Release Oral Suspension and need to use more than one packet for their dose, instruct them regarding the correct amount of water to use when mixing their dose.
Advise patients to immediately report and seek care for any cardiovascular or neurological symptoms including palpitations, dizziness, seizures, and tetany as these may be signs of hypomagnesemia [see Warnings and Precautions (5.6)].
Distributed by:
AstraZeneca LP
Wilmington, DE 19850
NEXIUM and the color purple as applied to the capsule are registered trademarks of the AstraZeneca group of companies.
©AstraZeneca 2011
Relabeling and Repackaging by: Physicians Total Care, Inc.Tulsa, Oklahoma      74146
Fda-approved Patient Labeling
NEXIUM® (nex-e-um) (esomeprazole magnesium)
Delayed-Release Capsules and Delayed-Release Oral Suspension
Read the Patient Information that comes with NEXIUM before you start taking it and each time you get a refill. There may be new information. This leaflet does not take the place of talking with your doctor about your medical condition or your treatment.
If you have any questions about NEXIUM, ask your doctor.
What is Nexium?
NEXIUM is a prescription medicine called a proton pump inhibitor (PPI).
NEXIUM is used in adults:
⢠for 4 to 8 weeks to treat the symptoms of gastroesophageal reflux disease (GERD). NEXIUM may also be prescribed to heal acid-related damage to the lining of the esophagus (erosive esophagitis), and to help continue this healing.
GERD is a chronic condition (lasts a long time) that occurs when acid from the stomach backs up into the esophagus (food pipe) causing symptoms, such as heartburn, or damage to the lining of the esophagus. Common symptoms include frequent heartburn that will not go away, a sour or bitter taste in the mouth, and difficulty swallowing.
⢠for up to 6 months to reduce the risk of stomach ulcers in some people taking pain medicines called non-steroidal anti-inflammatory drugs (NSAIDs).
⢠to treat patients with a stomach infection (Helicobacter pylori), along with the antibiotics amoxicillin and clarithromycin.
⢠for the long-term treatment of conditions where your stomach makes too much acid, including Zollinger-Ellison Syndrome. Zollinger-Ellison Syndrome is a rare condition in which the stomach produces a more than normal amount of acid.
For children and adolescents 1 year to 17 years of age, NEXIUM may be prescribed for up to 8 weeks for short-term treatment of GERD.
In children ages 1 month to less than 1 year of age, NEXIUM is only used to treat GERD with acid-related damage to the esophagus (erosive esophagitis) for up to 6 weeks.
It is not known if NEXIUM is effective in children under 1 month of age.
Who should not take Nexium?
Do not take NEXIUM if you:
⢠are allergic to any of the ingredients in NEXIUM. See the end of this leaflet for a complete ul of ingredients in NEXIUM.
⢠are allergic to any other Proton Pump Inhibitor (PPI) medicine.
What should I tell my doctor before taking Nexium?
Tell your doctor about all your medical conditions, including if you:
have been told that you have low magnesium levels in your blood
have liver problems
are pregnant, think you may be pregnant, or are planning to become pregnant.
are breastfeeding or planning to breastfeed. Talk with your doctor about the best way to feed your baby if you take NEXIUM.
Tell your doctor about all of the medicines you take including prescription and non-prescription drugs, vitamins and herbal supplements. NEXIUM may affect how other medicines work, and other medicines may affect how NEXIUM works. Especially tell your doctor if you take:
warfarin (Coumadin)
ketoconazole (Nizoral)
voriconazole (Vfend)
atazanavir (Reyataz)
nelfinavir (Viracept)
saquinavir (Fortovase)
products that contain iron
digoxin (Lanoxin, Lanoxicaps)
St.Johnâs Wort (Hypericum perforatum)
Rifampin
cilostazol (Pletal)
diazepam (Valium)
tacrolimus (Prograf)
How should I take Nexium?
Take NEXIUM exactly as prescribed by your doctor.
Do not change your dose or stop NEXIUM without talking to your doctor.
Take NEXIUM at least 1 hour before a meal.
Swallow NEXIUM capsules whole. Never chew or crush NEXIUM.
If you have difficulty swallowing NEXIUM capsules, you may open the capsule and empty the contents into a tablespoon of applesauce. Be sure to swallow the applesauce right away. Do not store it for later use.
If you forget to take a dose of NEXIUM, take it as soon as you remember. If it is almost time for your next dose, do not take the missed dose. Take the next dose on time. Do not take a double dose to make up for a missed dose.
If you take too much NEXIUM, tell your doctor right away.
See the âInstructions for Useâ at the end of this leaflet for instructions how to take NEXIUM For Delayed-Release Oral Suspension, and how to mix and give NEXIUM Delayed-Release Capsules and NEXIUM For Delayed-Release Oral Suspension, through a nasogastric tube or gastric tube.
What are the possible side effects of Nexium?
Serious allergic reactions. Tell your doctor if you get any of the following symptoms with NEXIUM.
rash
face swelling
throat tightness
difficulty breathing
Your doctor may stop NEXIUM if these symptoms happen.
Low magnesium levels in your body. This problem can be serious. Low magnesium can happen in some people who take a proton pump inhibitor medicine for at least 3 months. If low magnesium levels happen, it is usually after a year of treatment. You may or may not have symptoms of low magnesium.
Tell your doctor right away if you have any of these symptoms:
seizures
dizziness
abnormal or fast heart beat
jitteriness
jerking movements or shaking (tremors)
muscle weakness
spasms of the hands and feet
cramps or muscle aches
spasm of the voice box
Your doctor may check the level of magnesium in your body before you start taking NEXIUM or during treatment if you will be taking NEXIUM for a long period of time.
The most common side effects with NEXIUM may include:
Headache
Diarrhea
Nausea
Gas
Abdominal pain
Constipation
Dry mouth
Drowsiness
People who are taking multiple daily doses of proton pump inhibitor medicines for a long period of time may have an increased risk of fractures of the hip, wrist or spine.
Tell your doctor about any side effects that bother you or that do not go away. These are not all the possible side effects with NEXIUM. Talk with your doctor or pharmacist if you have any questions about side effects.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store Nexium?
Store NEXIUM at room temperature between 68°F to 77°F (20°C to 25°C).
Keep the container of NEXIUM closed tightly.
Keep NEXIUM and all medicines out of the reach of children.
General Information about Nexium
Medicines are sometimes prescribed for purposes other than those uled in the Patient Information leaflet. Do not use NEXIUM for a condition for which it was not prescribed. Do not give NEXIUM to other people, even if they have the same symptoms you have. It may harm them.
This Patient Information leaflet provides a summary of the most important information about NEXIUM. For more information, ask your doctor. You can ask your doctor or pharmacist for information that is written for healthcare professionals. For more information, go to www.purplepill.com or call toll free 1-800-463-9486.
What are the ingredients in Nexium?
Active ingredient: esomeprazole magnesium trihydrate
Inactive ingredients in NEXIUM Delayed-Release Capsules (including the capsule shells): glyceryl monostearate 40-55, hydroxypropyl cellulose, hypromellose, magnesium stearate, methacrylic acid copolymer type C, polysorbate 80, sugar spheres, talc, triethyl citrate, gelatin, FD&C Blue #1, FD&C Red #40, D&C Red #28, titanium dioxide, shellac, ethyl alcohol, isopropyl alcohol, n-butyl alcohol, propylene glycol, sodium hydroxide, polyvinyl pyrrolidone, and D&C Yellow #10.
Inactive granules in NEXIUM Delayed-Release Oral Suspension: dextrose, xanthan gum, crospovidone, citric acid, iron oxide, and hydroxypropyl cellulose.
Instructions for Use
For instructions on taking Delayed-Release Capsules, see the section of this leaflet called âHow should I take Nexium?â
Take NEXIUM for Delayed-Release Oral Suspension as follows:
NEXIUM for Delayed-Release Oral Suspension comes in foil packets containing 2.5 mg, 5 mg, 10 mg, 20 mg, or 40 mg strengths.
You should use an oral syringe to measure the amount of water needed to mix your dose. Ask your pharmacist for an oral syringe.
If your prescribed dose is 2.5 mg or 5 mg, add 5 mL of water to a container, then add the contents of a foil packet containing the dose prescribed by your doctor.
If your prescribed dose is 10 mg, 20 mg, or 40 mg, add 15 mL of water to a container, then add the contents of a foil packet containing the dose prescribed by your doctor.
If you or your child are instructed to use more than one foil packet for the prescribed dose, follow the mixing instructions provided by your pharmacist or doctor.
Stir.
Leave 2 to 3 minutes to thicken.
Stir and take dose within 30 minutes. If not used within 30 minutes, throw away this dose and mix a new dose.
If any medicine remains after drinking, add more water, stir, and take dose right away.
For young children, you can give the dose with an oral syringe. Rinse the oral syringe with water after each use.
NEXIUM Delayed-Release Capsules and NEXIUM for Delayed-Release Oral Suspension may be given through a nasogastric tube (NG tube) or gastric tube, as prescribed by your doctor. Follow the instructions below:
NEXIUM Delayed-Release Capsules:
Open the capsule and empty the granules into a 60 mL catheter tipped syringe. Mix with 50 mL of water. Use only a catheter tipped syringe to give NEXIUM through a NG tube.
Replace the plunger and shake the syringe well for 15 seconds. Hold the syringe with the tip up and check for granules in the tip.
Give the medicine right away.
Do not give the granules if they have dissolved or have broken into pieces.
Attach the syringe to the NG tube. Give the medicine in the syringe through the NG tube into the stomach.
After giving the granules, flush the NG tube with more water.
NEXIUM For Delayed-Release Oral Suspension:
NEXIUM for Delayed-Release Oral Suspension comes in foil packets containing 2.5 mg, 5 mg, 10 mg, 20 mg, or 40 mg strengths.
Use only a catheter tipped syringe to give NEXIUM through a NG tube or gastric tube
If your prescribed dose is 2.5 mg or 5 mg, add 5 mL of water to a catheter tipped syringe, then add the contents of a foil packet containing the dose prescribed by your doctor.
If your prescribed dose is 10 mg, 20 mg, or 40 mg, add 15 mL of water to a catheter tipped syringe, then add the contents of a foil packet containing the dose prescribed by your doctor.
Shake the syringe right away and then leave it for 2 to 3 minutes to thicken.
Shake the syringe and give the medicine through the NG or gastric tube (French size 6 or larger) into the stomach within 30 minutes.
Refill the syringe with the same amount of water (either 5 mL or 15 mL of water depending on your dose).
Shake the syringe and flush any remaining medicine from the NG tube or gastric tube into the stomach.
This Patient Information has been approved by the U.S. Food and Drug Administration.
AstraZeneca Pharmaceuticals LP
Wilmington, DE 19850
December 2011
NEXIUM is a registered trademark of the AstraZeneca group of companies.
©2011 AstraZeneca Pharmaceuticals LP. All rights reserved
Principal Display Panel
NEXIUM Delayed-Release Capsules, 20 mg NEXIUM Delayed-Release Capsules, 40 mg
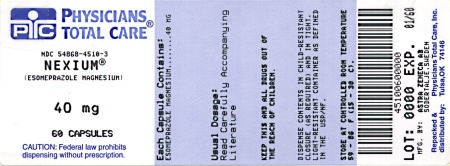
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site