Zydelig (idelalisib 150 mg) Dailymed
Generic: idelalisib is used for the treatment of Hypersensitivity Leukemia, Lymphoid Lymphoma, Non-Hodgkin
Boxed Warning
Warning: Fatal And Serious Toxicities: Hepatic, Severe Diarrhea, Colitis, Pneumonitis, Infections, And Intestinal Perforation
-
Fatal and/or serious hepatotoxicity occurred in 16% of Zydelig-treated patients. Monitor hepatic function prior to and during treatment. Interrupt and then reduce or discontinue Zydelig. (
5.1 ) -
Fatal and/or serious and severe diarrhea or colitis occurred in 20% of Zydelig-treated patients. Monitor for the development of severe diarrhea or colitis. Interrupt and then reduce or discontinue Zydelig. (
5.2 ) -
Fatal and/or serious pneumonitis occurred in 4% of Zydelig-treated patients. Monitor for pulmonary symptoms and bilateral interstitial infiltrates. Interrupt or discontinue Zydelig. (
5.3 ) -
Fatal and/or serious infections occurred in 48% of Zydelig-treated patients. Monitor for signs and symptoms of infection. Interrupt Zydelig if infection is suspected. (
5.4 ) -
Fatal and serious intestinal perforation can occur in Zydelig-treated patients across clinical trials. Discontinue Zydelig if intestinal perforation is suspected. (
5.5 )
Go PRO for all pill images
Warning: Fatal And Serious Toxicities: Hepatic, Severe Diarrhea, Colitis, Pneumonitis, Infections, And Intestinal Perforation
Fatal and/or serious hepatotoxicity occurred in 16% of Zydelig-treated patients. Monitor hepatic function prior to and during treatment. Interrupt and then reduce or discontinue Zydelig as recommended [see Dosage and Administration (2.2), Warnings and Precautions (5.1)].
Fatal and/or serious and severe diarrhea or colitis occurred in 20% of Zydelig-treated patients. Monitor for the development of severe diarrhea or colitis. Interrupt and then reduce or discontinue Zydelig as recommended [see Dosage and Administration (2.2), Warnings and Precautions (5.2)].
Fatal and/or serious pneumonitis occurred in 4% of Zydelig-treated patients. Monitor for pulmonary symptoms and bilateral interstitial infiltrates. Interrupt or discontinue Zydelig as recommended [see Dosage and Administration (2.2), Warnings and Precautions (5.3)].
Fatal and/or serious infections occurred in 48% of Zydelig-treated patients. Monitor for signs and symptoms of infection. Interrupt Zydelig if infection is suspected [see Dosage and Administration (2.2), Warnings and Precautions (5.4)].
Fatal and serious intestinal perforation can occur in Zydelig-treated patients across clinical trials. Discontinue Zydelig for intestinal perforation [see Warnings and Precautions (5.5)].
WARNING: FATAL AND SERIOUS TOXICITIES: HEPATIC, SEVERE DIARRHEA, COLITIS, PNEUMONITIS, INFECTIONS, and INTESTINAL PERFORATION
See full prescribing information for complete boxed warning.
- Fatal and/or serious hepatotoxicity occurred in 16% of Zydelig-treated patients. Monitor hepatic function prior to and during treatment. Interrupt and then reduce or discontinue Zydelig. (
5.1 )- Fatal and/or serious and severe diarrhea or colitis occurred in 20% of Zydelig-treated patients. Monitor for the development of severe diarrhea or colitis. Interrupt and then reduce or discontinue Zydelig. (
5.2 )- Fatal and/or serious pneumonitis occurred in 4% of Zydelig-treated patients. Monitor for pulmonary symptoms and bilateral interstitial infiltrates. Interrupt or discontinue Zydelig. (
5.3 )- Fatal and/or serious infections occurred in 48% of Zydelig-treated patients. Monitor for signs and symptoms of infection. Interrupt Zydelig if infection is suspected. (
5.4 )- Fatal and serious intestinal perforation can occur in Zydelig-treated patients across clinical trials. Discontinue Zydelig if intestinal perforation is suspected. (
5.5 )
Recent Major Changes Section
Indications and Usage, Relapsed Follicular B-cell non-Hodgkin Lymphoma – Accelerated Approval Indication Removed ( 1 )      2/2022Indications and Usage, Relapsed Small Lymphocytic Lymphoma – Accelerated Approval Indication Removed ( 1 )      2/2022
1indications And Usage
Zydelig is indicated, in combination with rituximab, for the treatment of patients with relapsed chronic lymphocytic leukemia (CLL) for whom rituximab alone would be considered appropriate therapy due to other co-morbidities.
Zydelig is a kinase inhibitor indicated for the treatment of patients with:
- Relapsed chronic lymphocytic leukemia (CLL), in combination with rituximab, in patients for whom rituximab alone would be considered appropriate therapy due to other co-morbidities. (
1 )
Limitations of use:
Zydelig is not indicated and is not recommended for first-line treatment of any patient, including patients with CLL, small lymphocytic lymphoma (SLL), follicular lymphoma (FL), and other indolent non-Hodgkin lymphomas. (1 ,6.1 )
Zydelig is not indicated and is not recommended in combination with bendamustine and rituximab, or in combination with rituximab for the treatment of patients with FL, SLL, and other indolent non-Hodgkin lymphomas. (6.1 )
Limitations of Use
Zydelig is not indicated and is not recommended for first-line treatment of any patient, including patients with CLL, small lymphocytic lymphoma (SLL), follicular lymphoma (FL), and other indolent non-Hodgkin lymphomas.
Zydelig is not indicated and is not recommended in combination with bendamustine and rituximab, or in combination with rituximab for the treatment of patients with FL, SLL, and other indolent non-Hodgkin lymphomas.
2 Dosage And Administration
Recommended dosage: 150 mg orally twice daily. (2.1 )
2.1 Recommended Dosage
The recommended dosage of Zydelig is 150 mg administered orally twice daily with or without food until disease progression or unacceptable toxicity. The optimal and safe dosing regimen for patients who receive treatment longer than several months is unknown.
Swallow tablets whole.
If a planned dose of Zydelig is missed by less than 6 hours, take the missed dose as soon as possible and take the next dose as usual. If a dose of Zydelig is missed by more than 6 hours, skip the missed dose and take the next dose at the usual time.
2.2 Dosage Modifications for Adverse Reactions
Table 1 presents the dosage modification for specific adverse reactions.
For other severe or life-threatening adverse reactions, withhold Zydelig until resolution. If resuming Zydelig after interruption for other severe or life-threatening toxicities, reduce the dosage to 100 mg orally twice daily. Permanently discontinue Zydelig for recurrence of other severe or life-threatening Zydelig-related toxicity upon rechallenge.
Table 1 Dosage Modifications for Adverse Reactions Abbreviations: ANC: absolute neutrophil count; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BID, twice daily; ULN, upper limit of normal; CMV, cytomegalovirus; DRESS, drug reaction with eosinophilia and systemic symptoms; PCR: polymerase chain reaction; PJP: Pneumocystis jirovecii pneumonia; SJS: Stevens-Johnson syndrome; TEN: toxic epidermal necrolysis ALT/AST >3–5 × ULN >5–20 × ULN >20 × ULN [see Warnings and Precautions (5.1)] Maintain Zydelig dose. Monitor at least weekly until ≤1 × ULN. Withhold Zydelig.Monitor at least weekly until ALT/AST are ≤1 × ULN, then may resume Zydelig at 100 mg BID. Discontinue Zydelig permanently. Bilirubin >1.5–3 × ULN >3–10 × ULN >10 × ULN [see Warnings and Precautions (5.1)] Maintain Zydelig dose. Monitor at least weekly until ≤1 × ULN. Withhold Zydelig.Monitor at least weekly until bilirubin is ≤1 × ULN, then may resume Zydelig at 100 mg BID. Discontinue Zydelig permanently. Diarrhea Moderate diarrhea: increase of 4–6 stools per day over baseline; severe diarrhea: increase of ≥7 stools per day over baseline. Moderate diarrhea Severe diarrhea or hospitalization Life-threatening diarrhea [see Warnings and Precautions (5.2)] Maintain Zydelig dose. Monitor at least weekly until resolved. Withhold Zydelig.Monitor at least weekly until resolved, then may resume Zydelig at 100 mg BID. Discontinue Zydelig permanently. Pneumonitis Any symptomatic pneumonitis [see Warnings and Precautions (5.3)] Discontinue Zydelig in patients with any severity of symptomatic pneumonitis. Infections Grade 3 or higher sepsis or pneumonia [see Warnings and Precautions (5.4)] Interrupt Zydelig until infection has resolved. Evidence of CMV infection or viremia Interrupt Zydelig in patients with evidence of active CMV infection of any grade or viremia (positive PCR or antigen test) until the viremia has resolved. If Zydelig is resumed, monitor patients by PCR or antigen test for CMV reactivation at least monthly. Evidence of PJP infection Interrupt Zydelig in patients with suspected PJP infection of any grade.Permanently discontinue Zydelig if PJP infection is confirmed. Intestinal Perforation Evidence of intestinal perforation [see Warnings and Precautions (5.5)] Permanently discontinue Zydelig in patients who experience intestinal perforation. Severe Cutaneous Reactions Suspected/Confirmed SJS, TEN, DRESS, or other severe or life-threatening (Grade ≥3) cutaneous reactions [see Warnings and Precautions (5.6)] Interrupt Zydelig in patients with suspected SJS, TEN, or DRESS until the etiology of the reaction has been determined.Permanently discontinue Zydelig in patients with confirmed SJS, TEN, or DRESS, or other severe or life-threatening (Grade ≥3) cutaneous reactions. Hypersensitivity Reactions Evidence of hypersensitivity reactions [see Warnings and Precautions (5.7)] Permanently discontinue Zydelig in patients who develop serious hypersensitivity reactions. Neutropenia ANC 1.0 to <1.5 Gi/L ANC 0.5 to <1.0 Gi/L ANC <0.5 Gi/L [see Warnings and Precautions (5.8)] Maintain Zydelig dose. Maintain Zydelig dose. Monitor ANC at least weekly. Interrupt Zydelig. Monitor ANC at least weekly until ANC ≥0.5 Gi/L, then may resume Zydelig at 100 mg BID. Thrombocytopenia Platelets 50 to <75 Gi/L Platelets 25 to <50 Gi/L Platelets <25 Gi/L [see Adverse Reactions (6.1)] Maintain Zydelig dose. Maintain Zydelig dose. Monitor platelet counts at least weekly. Interrupt Zydelig. Monitor platelet count at least weekly. May resume Zydelig at 100 mg BID when platelets ≥25 Gi/L.
No dosage modification is recommended for lymphocytosis, which has been observed in some patients taking Zydelig. This observed lymphocytosis is a pharmacodynamic effect and should not be considered progressive disease in the absence of other clinical findings.
3dosage Forms And Strengths
Tablets:
- 100 mg: orange, oval-shaped, film-coated tablet debossed with "GSI" on one side and "100" on the other side.
- 150 mg: pink, oval-shaped, film-coated tablet debossed with "GSI" on one side and "150" on the other side.
Tablets: 100 mg, 150 mg. (3 )
4 Contraindications
Zydelig is contraindicated in patients with a history of serious hypersensitivity reactions to idelalisib, including anaphylaxis, or patients with a history of toxic epidermal necrolysis with any drug [see Warnings and Precautions (5.6, 5.7)] .
History of serious hypersensitivity reactions to idelalisib, including anaphylaxis, or history of toxic epidermal necrolysis with any drug. (4 )
5 Warnings And Precautions
- Severe Cutaneous Reactions: Monitor patients for the development of severe cutaneous reactions. Permanently discontinue Zydelig if confirmed. (
2.2 ,5.6 )- Hypersensitivity Reactions: Permanently discontinue Zydelig and institute appropriate supportive measures. (
2.2 ,5.7 )- Neutropenia: Monitor blood counts. Interrupt Zydelig until resolution and resume at reduced dose. (
2.2 ,5.8 )- Embryo-fetal Toxicity: May cause fetal harm. Advise females of reproductive potential of potential risk to a fetus and to use effective contraception. (
5.9 ,8.1 ,8.3 )5.1 Hepatotoxicity
Fatal and/or serious hepatotoxicity occurred in 16% of patients treated with Zydelig in combination with rituximab or with unapproved combination therapies. Elevations in ALT or AST greater than 5 times the upper limit of normal have occurred [see Adverse Reactions (6.1)]. These findings were generally observed within the first 12 weeks of treatment and were reversible with dose interruption. After resumption of treatment at a lower dose, 26% of patients had recurrence of ALT and AST elevations. Discontinue Zydelig for recurrent hepatotoxicity.
Avoid concurrent use of Zydelig with other drugs that may cause liver toxicity.
Monitor ALT and AST in all patients every 2 weeks for the first 3 months of treatment, every 4 weeks for the next 3 months, then every 1 to 3 months thereafter. Monitor weekly for liver toxicity if the ALT or AST rises above 3 times the upper limit of normal until resolved. Withhold Zydelig if the ALT or AST is greater than 5 times the upper limit of normal, and continue to monitor AST, ALT and total bilirubin weekly until the abnormality is resolved [see Dosage and Administration (2.2)].
5.2 Severe Diarrhea or Colitis
Severe diarrhea or colitis (Grade 3 or higher) occurred in 20% of patients treated with Zydelig in combination with rituximab or with unapproved combination therapies [see Adverse Reactions (6.1)]. Diarrhea can occur at any time. Avoid concurrent use of Zydelig and other drugs that cause diarrhea. Diarrhea due to Zydelig responds poorly to antimotility agents. Median time to resolution ranged between 1 week and 1 month across trials, following interruption of Zydelig therapy and in some instances, use of corticosteroids [see Dosage and Administration (2.2)].
5.3 Pneumonitis
Fatal and serious pneumonitis occurred in patients treated with Zydelig [see Adverse Reactions (6.1)]. Clinical manifestations included interstitial infiltrates and organizing pneumonia. In randomized clinical trials of combination therapies, pneumonitis occurred in 4% of patients treated with Zydelig compared to 1% on the comparator arms. Time to onset of pneumonitis ranged from <1 to 15 months. Monitor patients on Zydelig for pulmonary symptoms. In patients taking Zydelig who present with pulmonary symptoms such as cough, dyspnea, hypoxia, interstitial infiltrates on a radiologic exam, or a decline by more than 5% in oxygen saturation, interrupt Zydelig until the etiology has been determined.
If symptomatic pneumonitis or organizing pneumonia is diagnosed, initiate appropriate treatment with corticosteroids and permanently discontinue Zydelig [see Dosage and Administration (2.2)].
5.4 Infections
Fatal and/or serious infections occurred in 48% of patients treated with Zydelig in combination with rituximab or with unapproved combination therapies [see Adverse Reactions (6.1)]. The most common infections were pneumonia, sepsis, and febrile neutropenia. Treat infections prior to initiation of Zydelig therapy. Monitor patients on Zydelig for signs and symptoms of infection, and interrupt Zydelig for Grade 3 or higher infection [see Dosage and Administration (2.2)].
Serious or fatal Pneumocystis jirovecii pneumonia (PJP) or cytomegalovirus (CMV) occurred in <1% of patients treated with Zydelig. Provide PJP prophylaxis during treatment with Zydelig. Interrupt Zydelig in patients with suspected PJP infection of any grade, and permanently discontinue Zydelig if PJP infection of any grade is confirmed. Regular clinical and laboratory monitoring for CMV infection is recommended in patients with history of CMV infection or positive CMV serology at the start of treatment with Zydelig. Interrupt Zydelig in the setting of positive CMV PCR or antigen test until the viremia has resolved. If Zydelig is subsequently resumed, patients should be monitored by PCR or antigen test for CMV reactivation at least monthly [see Dosage and Administration (2.2)].
5.5 Intestinal Perforation
Fatal and serious intestinal perforation occurred in Zydelig-treated patients. At the time of perforation, some patients had moderate to severe diarrhea. Advise patients to promptly report any new or worsening abdominal pain, chills, fever, nausea, or vomiting. Discontinue Zydelig permanently in patients who experience intestinal perforation.
5.6 Severe Cutaneous Reactions
Fatal cases of Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) have occurred in patients treated with Zydelig. Cases of drug reaction with eosinophilia and systemic symptoms (DRESS) have also occurred [see Adverse Reactions (6.2)]. Zydelig is contraindicated in patients with a history of toxic epidermal necrolysis [see Contraindications (4)]. If SJS, TEN, or DRESS is suspected, interrupt Zydelig until the etiology of the reaction has been determined. If SJS, TEN, or DRESS is confirmed, permanently discontinue Zydelig [see Dosage and Administration (2.2)].
Other severe or life-threatening (Grade ≥3) cutaneous reactions, including dermatitis exfoliative, rash, rash erythematous, rash generalized, rash macular, rash maculo-papular, rash papular, rash pruritic, exfoliative rash, and skin disorder, have been reported in patients treated with Zydelig. Monitor patients for the development of other severe or life-threatening cutaneous reactions and permanently discontinue Zydelig [see Dosage and Administration (2.2)].
5.7 Hypersensitivity Reactions
Serious hypersensitivity reactions, including anaphylaxis, have been reported in patients on Zydelig. Zydelig is contraindicated in patients with a history of serious hypersensitivity reactions to idelalisib, including anaphylaxis [see Contraindications (4)]. In patients who develop serious hypersensitivity reactions, permanently discontinue Zydelig [see Dosage and Administration (2.2)] and institute appropriate supportive measures.
5.8 Neutropenia
Grade 3 or 4 neutropenia occurred in 58% of patients treated with Zydelig in combination with rituximab or with unapproved combination therapies [see Adverse Reactions (6.1)]. Monitor blood counts at least every 2 weeks for the first 6 months of therapy, and at least weekly in patients while neutrophil counts are less than 1.0 Gi/L. Interrupt Zydelig until resolution and resume at reduced dose [see Dosage and Administration (2.2)].
5.9 Embryo-fetal Toxicity
Based on findings in animals and its mechanism of action, Zydelig may cause fetal harm when administered to a pregnant woman. In animal reproduction studies, administration of idelalisib to pregnant rats during organogenesis caused decreased fetal weight and congenital malformations at systemic exposures 12 times those reported in patients at the recommended dose of 150 mg twice daily.
Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with Zydelig and for 1 month after the last dose [see Use in Specific Populations (8.1, 8.3)].
6adverse Reactions
The following clinically significant adverse reactions are described elsewhere in the labeling.
- Hepatotoxicity [see Warnings and Precautions (5.1)]
- Severe Diarrhea or Colitis [see Warnings and Precautions (5.2)]
- Pneumonitis [see Warnings and Precautions (5.3)]
- Infections [see Warnings and Precautions (5.4)]
- Intestinal Perforation [see Warnings and Precautions (5.5)]
- Severe Cutaneous Reactions [see Warnings and Precautions (5.6)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.7)]
- Neutropenia [see Warnings and Precautions (5.8)]
- The most common adverse reactions (incidence ≥30%) in patients treated with Zydelig in combination trials are diarrhea, pneumonia, pyrexia, fatigue, rash, cough, and nausea. (
6.1 )- Common laboratory abnormalities are neutropenia, ALT elevations and AST elevations. (
6.1 )
To report SUSPECTED ADVERSE REACTIONS, contact Gilead Sciences, Inc. at 1-800-GILEAD-5 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The pooled safety population described in the WARNINGS AND PRECAUTIONS reflect exposure to Zydelig at a dosage of 150 mg twice daily in 110 patients administered in combination with rituximab in Study 312-0116, and in combination with other drugs in 380 patients. Among 490 patients who received Zydelig, 74% were exposed for 6 months or longer and 50% were exposed for one year or longer. In this pooled safety population, the most common (> 30%) adverse reactions were diarrhea, pneumonia, pyrexia, fatigue, rash, cough, and nausea. Common laboratory abnormalities were neutropenia, ALT elevations and AST elevations.
Summary of Clinical Trials in Chronic Lymphocytic Leukemia
The safety data reflect exposure to Zydelig from two randomized, double-blind clinical trials (Studies 312-0116 and 312-0115) in 634 patients with relapsed CLL [see Clinical Studies (14.1)] and one randomized, open-label trial in 259 patients with relapsed CLL (Study 312-0119).
Zydelig with Rituximab (Study 312-0116)
Patients with relapsed CLL received up to 8 doses of rituximab (R) with (n=110) or without Zydelig (n=108)150 mg twice daily. The median duration of exposure to Zydelig was 8 months.
Serious adverse reactions were reported in 65 (59%) patients treated with Zydelig + R The most frequent serious adverse reactions reported for patients treated with Zydelig + R were pneumonia (23%), diarrhea (10%), pyrexia (9%), sepsis (8%), and febrile neutropenia (5%).
Adverse reactions that led to discontinuation of Zydelig occurred in 19 (17%) patients. The most common adverse reactions that led to treatment discontinuations were hepatotoxicity and diarrhea/colitis.
Forty-two (38%) patients had dose interruptions and sixteen (15%) patients had dose reductions due to adverse reactions or laboratory abnormalities. The most common reasons for dose interruptions or reductions were pneumonia, diarrhea or colitis, rash, and elevated transaminases.
Table 2 and Table 3 summarize common adverse reactions and laboratory abnormalities reported for Zydelig + R and placebo + R arms.
Table 2 Adverse Reactions Reported in ≥5% of Patients with CLL and Occurred at ≥2% Higher Incidence in Patients Receiving Zydelig in Study 312-0116 Zydelig + RN=110 (%) Placebo + RN=108 (%) Adverse Reaction Any Grade Grade ≥3 Any Grade Grade ≥3 General disorders and administration site conditions   pyrexia 44 (40) 3 (3) 20 (19) 1 (1)   chills 27 (25) 2 (2) 17 (16) 0   pain 8 (7) 0 1 (1) 0 Gastrointestinal disorders   diarrhea Diarrhea includes the following preferred terms: diarrhea, colitis. 35 (32) 12 (11) 20 (19) 0   nausea 30 (27) 1 (1) 25 (23) 0   abdominal pain Abdominal pain includes the following preferred terms: abdominal pain, abdominal pain upper, abdominal pain lower. 20 (18) 1 (1) 17 (16) 2 (2)   vomiting 17 (15) 0 9 (8) 0   gastroesophageal reflux disease 11 (10) 1 (1) 0 0   stomatitis 7 (6) 2 (2) 1 (1) 0 Respiratory, thoracic, and mediastinal disorders   pneumonia Pneumonia includes the terms: pneumonia, pneumonitis, lung infection, lung infiltration, pneumocystis jiroveci pneumonia, pneumonia legionella, lung infection pseudomonal, pneumonia fungal, respiratory tract infection, lower respiratory tract infection, and lower respiratory tract infection bacterial. 33 (30) 23 (21) 20 (19) 14 (13) Skin and subcutaneous tissue disorders   rash Rash includes the following preferred terms: dermatitis exfoliative, drug eruption, rash, rash erythematous, rash generalized, rash macular, rash maculo-papular, rash papular, rash pruritic, rash morbilliform, and exfoliative rash. 27 (25) 4 (4) 7 (6) 1 (1) Metabolism and Nutrition Disorders   decreased appetite 18 (16) 2 (2) 12 (11) 2 (2)   dehydration 7 (6) 3 (3) 0 0 Infections and infestations   sepsis Sepsis includes the terms: sepsis, septic shock, neutropenic sepsis, and sepsis syndrome 10 (9) 10 (9) 4 (4) 4 (4)   sinusitis 9 (8) 0 6 (6) 0   urinary tract infection 9 (8) 1 (1) 4 (4) 2 (2)   bronchitis 8 (7) 1 (1) 5 (5) 1 (1)   oral herpes 6 (5) 1 (1) 3 (3) 0 Psychiatric disorders   insomnia 10 (9) 0 7 (6) 0 Musculoskeletal and connective tissue disorders   arthralgia 9 (8) 1 (1) 4 (4) 0 Nervous system disorders   lethargy 6 (5) 0 2 (2) 0
Table 3 Hematologic and Hepatic Laboratory Abnormalities Reported in ≥10% of Patients with CLL and Occurred at ≥5% Higher Incidence in Patients Receiving Zydelig in Study 312-0116 Zydelig + RN=110 (%) Placebo + RN=108 (%) Laboratory Parameter Any Grade Grade 3–4 Any Grade Grade 3–4 Hematology abnormalities   neutropenia 71 (65) 46 (42) 61 (56) 33 (31)   leukopenia 34 (31) 9 (8) 25 (23) 9 (8)   lymphocytopenia 23 (21) 11 (10) 13 (12) 4 (4) Serum chemistry abnormalities   ALT increased 43 (39) 10 (9) 13 (12) 1 (1)   AST increased 31 (28) 6 (5) 16 (15) 0
After closure of Study 312-0116, 71 patients continued treatment with Zydelig on an extension study (Study 312-0117). The median duration of exposure was 18 months. Serious adverse reactions occurred in 48 (68%) patients. The most frequent serious adverse reactions reported were pneumonia (30%), diarrhea (15%), and pyrexia (11%).
The most frequent adverse reactions were pneumonia (51%), pyrexia (46%), and cough (45%). The most frequent Grade 3 or greater adverse reactions were pneumonia (30%), diarrhea (15%), and sepsis (10%).
Zydelig with Ofatumumab (Study 312-0119)
In Study 312-0119, 259 patients with relapsed CLL received up to 12 doses of ofatumumab with or without Zydelig 150 mg orally twice daily. Zydelig in combination with ofatumumab is not indicated for the treatment of relapsed CLL. The median duration of exposure to Zydelig was 13.9 months.
Serious adverse reactions were reported in 133 (77%) patients treated with Zydelig + ofatumumab. The most frequent serious adverse reactions reported were pneumonia (14%), pyrexia (13%), and diarrhea (12%).
Adverse reactions that led to discontinuation of Zydelig occurred in 71 (41%) patients.
One hundred and ten (64%) patients had dose interruptions and 42 (24%) patients had dose reductions due to adverse reactions or laboratory abnormalities. The most common reasons for dose discontinuations, reductions, or interruptions were diarrhea and colitis.
The most common adverse reactions were diarrhea (55%), pyrexia (38%), nausea (34%), and fatigue (34%).
Zydelig with Bendamustine and Rituximab (Study 312-0115)
In Study 312-0115, patients with relapsed CLL received up to 6 cycles of bendamustine and rituximab (BR) with or without Zydelig 150 mg orally twice daily. Zydelig in combination with bendamustine and rituximab is not indicated for the treatment of relapsed CLL. The median duration of exposure to Zydelig was 18.2 months.
Serious adverse reactions were reported in 147 (71%) patients treated with Zydelig + BR. The most frequent serious adverse reactions reported for patients treated with Zydelig + BR were febrile neutropenia (21%), pneumonia (17%), pyrexia (12%), and diarrhea (6%).
Adverse reactions that led to discontinuation of Zydelig occurred in 68 (33%) patients. The most common adverse reactions that led to treatment discontinuations were pneumonia, diarrhea, and pyrexia.
One hundred twenty-two (59%) patients treated with Zydelig + BR had dose interruptions and 34 (16%) patients had dose reductions due to adverse reactions. The most common reasons for dose interruptions or reductions were increased ALT and diarrhea.
The most common adverse reactions were neutropenia (64%), pyrexia (43%), and diarrhea (41%).
Summary of Clinical Trials in Indolent Non-Hodgkin Lymphoma
The safety data reflect exposure to Zydelig from three open-label clinical trials (Studies 101-09, 101-02, and 101-10 in 146 patients with indolent non-Hodgkin lymphoma (iNHL) treated with Zydelig 150 mg orally twice daily. Zydelig is not indicated for the treatment of iNHL. The median duration of exposure was 6.1 months (range 0.3 to 26.4 months).
Serious adverse reactions were reported in 73 (50%) patients. The most frequent serious adverse reactions that occurred were pneumonia (15%), diarrhea (11%), and pyrexia (9%).
Adverse reactions resulted in interruption or discontinuation for 78 (53%) patients. The most common reasons for interruption or discontinuations were diarrhea (11%), pneumonia (11%), and elevated transaminases (10%).
The most common adverse reactions were neutropenia (53%), ALT increased (50%), diarrhea (47%), AST increased (41%), fatigue (30%), nausea and cough (29% each), anemia and pyrexia (28% each), abdominal pain and thrombocytopenia (26% each), and pneumonia (25%).
Summary of Discontinued Clinical Trials in Indolent Non-Hodgkin Lymphoma and First-Line CLL
Zydelig is not indicated for patients with indolent non-Hodgkin lymphoma or previously untreated CLL either as monotherapy or in combination with rituximab or BR. Safety data described below reflect exposure to Zydelig in three randomized, double-blind clinical trials (Studies 312-0123, 313-0124, and 313-0125) in patients with CLL and iNHL.
In Study 312-0123 (NCT01980888), 311 patients with previously untreated CLL received up to 6 cycles of BR with or without Zydelig 150 mg twice daily.
In Study 313-0124 (NCT01732913), 295 patients with previously treated iNHL [FL 66%, marginal zone lymphoma (MZL) 19%, SLL 9%, lymphoplasmacytic lymphoma (LPL)/Waldenstrom macroglobulinemia (WM) 6%] received 8 doses of R with or without Zydelig 150 mg twice daily. Patients had a median of one prior therapy.
In Study 313-0125 (NCT01732926), 475 patients with previously treated iNHL (FL 63%, MZL 15%, SLL 11%, LPL/WM 11%) received up to 6 cycles of BR with or without Zydelig 150 mg twice daily. Patients had a median of two prior therapies.
These three studies were terminated early due to a higher incidence of fatal and/or serious adverse reactions observed in patients treated with Zydelig in combination with R or BR. The most frequent serious adverse reactions were in the system organ classes of infections and infestations, blood and lymphatic system disorders, and gastrointestinal disorders.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of Zydelig. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Skin and Subcutaneous Disorders - Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and drug reaction with eosinophilia and systemic symptoms (DRESS)
7 Drug Interactions
- Strong CYP3A Inhibitors: Additional monitoring required if alternative therapy is not available. (
7.1 )- Strong CYP3A Inducers: Avoid coadministration of strong CYP3A inducers. (
7.1 )- CYP3A Substrates: Avoid coadministration of sensitive CYP3A substrates. (
7.2 )7.1 Effects of Other Drugs on Zydelig
Table 6 uls the potential effects of the coadministration of strong CYP3A modulators on Zydelig.
Table 6 Drug Interactions with Zydelig that affect Idelalisib Concentrations Strong CYP3A Inhibitors Clinical Impact
- Coadministration with strong CYP3A inhibitors may increase idelalisib concentrations [see Clinical Pharmacology (12.3)].
- Increased idelalisib concentrations may increase the risk of exposure related adverse reactions.
Prevention or Management
- Use other drugs that are not strong CYP3A inhibitors.
- If unable to use alternative drugs, monitor patients more frequently for Zydelig adverse reactions [see Adverse Reactions (6.1)].
Strong CYP3A Inducers Clinical Impact
- Coadministration with strong CYP3A inducers may decrease idelalisib concentrations [see Clinical Pharmacology (12.3)].
- Decreased idelalisib concentrations may reduce efficacy.
Prevention or Management Avoid coadministration of Zydelig with strong CYP3A4 inducers. 7.2 Effects of Zydelig on Other Drugs
The coadministration of Zydelig with a CYP3A substrate may increase the concentrations of this CYP3A substrate. Avoid coadministration of Zydelig with sensitive CYP3A substrates [see Clinical Pharmacology (12.3)].
8 Use In Specific Populations
Lactation: Advise not to breastfeed. (8.2 )
8.1 Pregnancy
Risk Summary
Based on findings in animal studies and the mechanism of action [see Clinical Pharmacology (12.1)], Zydelig may cause fetal harm when administered to a pregnant woman.
There are no available data in pregnant women to inform the drug-associated risk. In animal reproduction studies, administration of idelalisib to pregnant rats during organogenesis resulted in decreased fetal weight and congenital malformations in rats at maternal exposures (AUC) 12 times those reported in patients at the recommended dosage of 150 mg twice daily (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage of clinically recognized pregnancies 2–4% and 15–20%, respectively.
Data
Animal Data
In an embryo-fetal development study in rats, pregnant animals receiving oral doses of idelalisib during the period of organogenesis (implantation to closure of the hard palate), embryo-fetal toxicities were observed at the mid- and high-doses that also resulted in maternal toxicity, based on reductions in maternal body weight gain. Adverse findings at idelalisib doses ≥ 75 mg/kg/day included decreased fetal weights, external malformations (short tail), and skeletal variations (delayed ossification and/or unossification of the skull, vertebrae, and sternebrae). Additional findings were observed at 150 mg/kg/day dose of idelalisib and included urogenital blood loss, complete resorption, increased post-implantation loss, and malformations (vertebral agenesis with anury, hydrocephaly, and microphthalmia/anophthalmia). The dose of 75 and 150 mg/kg/day of idelalisib in rats resulted in exposures (AUC) of approximately 12 and 30 times, respectively, the human exposure at the recommended dose of 150 mg twice daily.
8.2 Lactation
Risk Summary
There are no data on the presence of idelalisib or its metabolites in human milk or its effects on the breastfed child or on milk production. Because of the potential for serious adverse reactions in the breastfed child, advise women not to breastfeed during treatment with Zydelig and for 1 month after the last dose.
8.3 Females and Males of Reproductive Potential
Zydelig may cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)].
Pregnancy
Pregnancy testing is recommended for females of reproductive potential prior to starting Zydelig.
Contraception
Females
Advise females of reproductive potential to use effective contraception during treatment with Zydelig and for 1 month after the last dose.
Males
Advise males with female partners of reproductive potential to use effective contraception during treatment with Zydelig and for 3 months after the last dose [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
Safety and effectiveness of Zydelig in pediatric patients have not been established.
8.5 Geriatric Use
Of the 490 patients with relapsed CLL who were treated with Zydelig in combination trials, 271 (55%) were 65 years of age and older. When comparing patients 65 years of age or older to younger patients with CLL, older patients had a higher incidence of discontinuation due to an adverse reaction (36% vs 28%), higher incidence of serious adverse reactions (73% vs 67%), and higher incidence of death (13% vs 9%).
8.6 Hepatic Impairment
No dose adjustment is recommended for patients with ALT or AST or bilirubin > upper limit of normal (ULN); however, limited safety and efficacy data are available for patients with baseline AST or ALT > 2.5 × ULN or bilirubin > 1.5 × ULN. Monitor patients with baseline hepatic impairment for adverse reactions [see Warnings and Precautions (5)]. Follow dosage modifications for adverse reactions [see Dosage and Administration (2.2)].
11 Description
Idelalisib is a kinase inhibitor. The chemical name for idelalisib is 5-fluoro-3-phenyl-2-[(1S)-1-(9H-purin-6-ylamino)propyl]quinazolin-4(3H)-one. It has a molecular formula of C22H18FN7O and a molecular weight of 415.42 g/mol. Idelalisib has the following structural formula:

Idelalisib is a white to off-white solid with a pH-dependent aqueous solubility ranging from <0.1 mg/mL at pH 5–7 to over 1 mg/mL at pH 2 under ambient conditions.
Zydelig (idelalisib) tablets are for oral use. Each tablet contains either 100 mg or 150 mg of idelalisib with the following inactive ingredients: microcrystalline cellulose, hydroxypropyl cellulose, croscarmellose sodium, sodium starch glycolate, magnesium stearate and a tablet coating. The tablet coating consists of polyethylene glycol, talc, polyvinyl alcohol, and titanium dioxide and of FD&C Yellow #6/Sunset Yellow FCF Aluminum Lake (for the 100 mg tablet) and red iron oxide (for the 150 mg tablet).
12 Clinical Pharmacology
12.1Mechanism of Action
Idelalisib is an inhibitor of phosphatidylinositol 3-kinase, PI3Kδ, which is expressed in normal and malignant B-cells. Idelalisib induced apoptosis and inhibited proliferation in cell lines derived from malignant B-cells and in primary tumor cells. Idelalisib inhibits several cell signaling pathways, including B-cell receptor (BCR) signaling and the CXCR4 and CXCR5 signaling, which are involved in trafficking and homing of B-cells to the lymph nodes and bone marrow. Treatment of lymphoma cells with idelalisib resulted in inhibition of chemotaxis and adhesion, and reduced cell viability.
12.2Pharmacodynamics
Cardiac Electrophysiology
At a dose 2.7 times the maximum recommended dose, Zydelig did not prolong the QT/QTc interval (i.e., ≤10 ms).
12.3Pharmacokinetics
Idelalisib exposure increased in a less than dose-proportional manner over a dose range of 50 mg to 350 mg twice daily (0.3 to 2.3 times the approved recommended dosage).
Following 150 mg twice daily administration of idelalisib, average (% coefficient of variation) maximum concentrations (Cmax) and area under the curve (AUC) at steady-state were 1861 (43%) ng/mL and 10598 (41%) ng∙h/mL for idelalisib.
Absorption
The median time to peak concentration (Tmax) was observed at 1.5 hours.
Food Effect
The administration of a single dose of Zydelig with a high-fat meal (900 calories: 525 calories fat, 250 calories carbohydrates, and 125 calories protein) increased idelalisib AUC 1.4-fold relative to fasting conditions.
Distribution
Protein binding of idelalisib is ≥ 84% with no concentration dependence.
The mean blood-to-plasma ratio was 0.7.
The apparent central volume of distribution at steady state is 23 L (%CV ~85%). Idelalisib is a substrate of P-glycoprotein (P-gp) and BCRP in vitro.
Elimination
The population apparent systemic clearance at steady-state is 14.9 L/hr (%CV ~ 38%). The population terminal elimination half-life of idelalisib is 8.2 hours.
Metabolism
Idelalisib is metabolized via aldehyde oxidase and CYP3A with additional minor metabolism by UGT1A4.
Excretion
Following a single 150 mg dose of radiolabeled idelalisib, 78% of the radioactivity was excreted in feces and 14% was excreted in the urine. Idelalisib is not a substrate of OATP1B1, OATP1B3, OAT1, OAT3, or OCT2.
Specific Populations
Age (18 to 91 years), sex, race (White, and non-Whites), renal impairment (creatinine clearance ≥ 15 mL/min) and weight (38 to 148 kg) had no effect on idelalisib exposure.
Patients with Hepatic Impairment
The mean AUC increased up to 1.7-fold in patients with hepatic impairment (defined as ALT or AST or bilirubin values ≥ ULN) compared to patients with normal hepatic function. There is limited information on idelalisib exposure in patients with baseline AST or ALT > 2.5 × ULN or bilirubin > 1.5 × ULN [see Specific Populations (8.6)].
Drug Interaction Studies
Effect of Other Drugs on Idelalisib
The coadministration of rifampin (strong CYP3A inducer and P-gp inducer) to healthy subjects decreased the mean idelalisib AUC by 75% and the mean Cmax by 58% [see Drug Interactions (7.1)].
The coadministration of ketoconazole (strong CYP3A inhibitor and P-gp inhibitor) to healthy subjects increased the mean idelalisib AUC by 1.8-fold. No changes in the mean Cmax were observed [see Drug Interactions (7.1)].
In vitro studies suggest that idelalisib inhibits CYP2C8, CYP2C19, and UGT1A1 and induces CYP2B6.
Effect of Idelalisib on Other Drugs
The mean Cmax of midazolam increased by 2.4-fold and the mean AUC of midazolam increased by 5.4-fold when midazolam (sensitive CYP3A substrate) was coadministered with Zydelig [see Drug Interactions (7.2)].
No changes in exposure to rosuvastatin (OATP1B1 and OATP1B3 substrate) or digoxin (P-glycoprotein substrate) were observed when coadministered with Zydelig.
13 Nonclinical Toxicology
13.1Carcinogenesis, Mutagenesis, Impairment of Fertility
Idelalisib was not carcinogenic in a 26-week study in transgenic mice when administered daily by oral gavage at doses up to 500 mg/kg/day in males and 1000 mg/kg/day in females. Idelalisib was not carcinogenic in a 2-year study in rats when administered daily by oral gavage at exposures 0.40/0.62-fold (male/female), compared to the exposure in patients with hematologic malignancies administered the recommended dose of 150 mg twice daily.
Idelalisib did not induce mutations in the bacterial mutagenesis (Ames) assay and was not clastogenic in the in vitro chromosome aberration assay using human peripheral blood lymphocytes. Idelalisib was genotoxic in males in the in vivo rat micronucleus study at a high dose of 2000 mg/kg.
Idelalisib may impair fertility in humans. In a fertility study, treated male rats (25, 50, or 100 mg/kg/day of idelalisib) were mated with untreated females. Decreased epididymidal and testicular weights were observed at all dose levels and reduced sperm concentration at the mid- and high doses; however, there were no adverse effects on fertility parameters. The low dose in males resulted in an exposure (AUC) that is approximately 50% of the exposure in patients at the recommended dose of 150 mg twice daily.
In a separate fertility study, treated female rats (25, 50, or 100 mg/kg/day of idelalisib) were mated with untreated males. There were no adverse effects on fertility parameters; however, there was a decrease in the number of live embryos at the high dose. The high dose in females resulted in an exposure (AUC) that is approximately 17-fold the exposure in patients at the recommended dose of 150 mg twice daily.
13.2 Animal Toxicology and/or Pharmacology
Toxicities observed in animals and not reported in patients include cardiac toxicity (cardiomyopathy, inflammation, and increased heart weight) and pancreatic findings (inflammation, hemorrhage, and low-incidence acinar degeneration and hyperplasia). These findings were observed in Sprague-Dawley rats in toxicology studies at exposures (AUCs) higher than those reported in patients at the recommended dose of 150 mg twice daily. Cardiac inflammation was mainly seen in a 28-day study in rats, the other findings were observed in the 13-week and/or 6-month studies.
14 Clinical Studies
Zydelig was evaluated in a randomized, double-blind, placebo-controlled study GS-US-312-0116 (referred to as 312-0116) (NCT01539512) in 220 patients with relapsed CLL who required treatment and were unable to tolerate standard chemoimmunotherapy due to coexisting medical conditions, reduced renal function as measured by creatinine clearance < 60 mL/min, or NCI CTCAE Grade ≥ 3 neutropenia or Grade ≥ 3 thrombocytopenia resulting from myelotoxic effects of prior therapy with cytotoxic agents. Patients were randomized 1:1 to receive 8 doses of rituximab (first dose at 375 mg/m2, subsequent doses at 500 mg/m2 every 2 weeks for 4 infusions and every 4 weeks for an additional 4 infusions) in combination with either an placebo taken orally twice daily or with Zydelig 150 mg taken orally twice daily until disease progression or unacceptable toxicity.
The median age was 71 years (range 47, 92) with 78% over 65, 66% were male, and 90% were White. The median time since diagnosis was 8.5 years. The median number of prior therapies was 3. Nearly all (96%) patients had received prior anti-CD20 monoclonal antibodies. The most common (>15%) prior regimens were: bendamustine + rituximab (BR) (98 patients, 45%), fludarabine + cyclophosphamide + rituximab (75 patients, 34%), single-agent rituximab (67 patients, 31%), fludarabine + rituximab (37 patients, 17%), and chlorambucil (36 patients, 16%). The median CIRS (Cumulative Illness Rating Scale) score was 8 (range 0–17), and 85% of patients had a score of >6. Median Karnofsky score was 80. Median estimated Creatinine Clearance (eCLcr) was 63.6 mL/min, with 41% of patients having an eCLcr of <60 mL/min. At screening, 19.5% of patients had a platelet count of <50 × 109/L, and 13.2% had an absolute neutrophil count (ANC) of <1 × 109/L.
The efficacy of Zydelig was based on progression free survival (PFS), as assessed by an independent review committee (IRC). The trial was stopped for efficacy following the first pre-specified interim analysis. Results of a second interim analysis continued to show a statistically significant improvement for Zydelig + R compared to placebo + R for the major efficacy outcome measure of PFS (HR: 0.18, 95% CI [0.10, 0.32], p <0.0001).
At the final analysis, with a median follow-up of 8.3 months for the Zydelig + R group, and 5.6 months for the placebo + R group, the median PFS for the Zydelig + R group was 19.4 months (95% CI: 12.3, Not Reached) versus 6.5 months (95% CI: 4.0, 7.3) for the placebo + R group (HR: 0.15, 95% CI [0.09, 0.24], p < 0.0001).
Updated efficacy results are shown in Table 7 and the Kaplan-Meier curve for PFS is shown in Figure 1.
Table 7 Efficacy Results from Study 312-0116 Zydelig + RN = 110 Placebo + RN = 110 PFS: progression-free survival; NR: not reached; ORR: overall response rate; PR: partial response; DOR: duration of response PFS Median (months) (95% CI) 19.4 (12.3, NR) 6.5 (4.0, 7.3) Hazard ratio (95% CI) 0.15 (0.09, 0.24) P-value < 0.0001 The p value for PFS was based on stratified log-rank test. ORR ORR defined as the proportion of patients who achieved a complete response (CR) or PR. All PRs achieved; none of the patients achieved a CR. (All PRs) 92 (83.6%) 17 (15.5%) 95% CI 75.4, 90.0 9.3, 23.6 Odds Ratio (95% CI) 27.8 (13.4, 57.5) P-value <0.0001 DOR Median (months) (95% CI) NR (12, NR) 6.2 (2.8, 6.5)
Figure 1 Kaplan-Meier Plot of IRC-Assessed PFS for Study 312-0116

16 How Supplied/storage And Handling
Zydelig tablets supplied as follows:
Tablet Strength Package Configuration NDC No. Description of Tablet; Debossed on Tablet 150 mg High density polyethylene (HDPE) bottle with a polyester fiber coil, capped with a child-resistant closure. Each bottle contains 60 film-coated tablets. 61958-1702-1 Oval shaped; pink; "150" on one side and "GSI" on the other side 100 mg 61958-1701-1 Oval-shaped; orange; "100" on one side and "GSI" on the other side STORAGE AND HANDLING SECTION
Store between 20–30 °C (68–86 °F) with excursions permitted 15–30 °C (59–86 °F).
- Dispense only in original container.
- Do not use if seal over bottle opening is broken or missing.
17 Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Hepatotoxicity
Advise patients that Zydelig can cause significant elevations in liver enzymes, and that serial testing of serum liver tests (ALT, AST, and bilirubin) are recommended while taking Zydelig [see Warnings and Precautions (5.1)]. Advise patients to report symptoms of liver dysfunction including jaundice, bruising, abdominal pain, or bleeding.
Severe Diarrhea or Colitis
Advise patients that Zydelig may cause severe diarrhea or colitis and to notify their healthcare provider immediately if the number of bowel movements in a day increases by six or more [see Warnings and Precautions (5.2)].
Pneumonitis
Advise patients of the possibility of pneumonitis, and to report any new or worsening respiratory symptoms including cough or dyspnea [see Warnings and Precautions (5.3)].
Infections
Advise patients that Zydelig can cause serious infections that may be fatal. Advise patients to immediately report symptoms of infection (e.g. pyrexia) [see Warnings and Precautions (5.4)].
Intestinal Perforation
Advise patients of the possibility for intestinal perforation and to notify their healthcare provider immediately if they experience severe abdominal pain [see Warnings and Precautions (5.5)].
Severe Cutaneous Reactions
Advise patients that Zydelig may cause severe cutaneous reactions and to notify their healthcare provider immediately if they develop a severe skin reaction [see Warnings and Precautions (5.6)].
Hypersensitivity Reactions
Advise patients that anaphylaxis can occur during treatment with Zydelig and to notify their healthcare provider immediately if they experience a hypersensitivity reaction, including anaphylaxis [see Warnings and Precautions (5.7)].
Neutropenia
Advise patients of the need for periodic monitoring of blood counts. Advise patients to notify their healthcare provider immediately if they develop a fever or any signs of infection [see Warnings and Precautions (5.8)].
Embryo-Fetal Toxicity
Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.9), Use in Specific Populations (8.1)].
Advise females of reproductive potential to use effective contraception during treatment with Zydelig and for 1 month after the last dose [see Use in Specific Populations (8.3)].
Advise males with female partners of reproductive potential to use effective contraception during treatment with Zydelig and for 3 months after receiving the last dose [see Use in Specific Populations (8.3)].
Lactation
Advise women not to breastfeed during treatment with Zydelig and for 1 month after the last dose [see Use in Specific Populations (8.2)].
Instructions for Taking Zydelig
Advise patients to take Zydelig exactly as prescribed and not to change their dose or to stop taking Zydelig unless they are told to do so by their healthcare provider. Zydelig may be taken with or without food. Zydelig tablets should be swallowed whole. Advise patients that if a dose of Zydelig is missed by less than 6 hours, to take the missed dose right away and take the next dose as usual. If a dose of Zydelig is missed by more than 6 hours, advise patients to wait and take the next dose at the usual time [see Dosage and Administration (2.1)].
Manufactured and distributed by:
Gilead Sciences, Inc.
Foster City, CA 94404
GSI and Zydelig are trademarks or registered trademarks of Gilead Sciences, Inc., or its related companies. All other trademarks referenced herein are the property of their respective owners.
© 2022 Gilead Sciences, Inc. All rights reserved.
205858-GS-006-PI
Spl Medguide Section
This Medication Guide has been approved by the U.S. Food and Drug Administration. Revised: 2/2022 MEDICATION GUIDEZYDELIG® (zye-DEL-ig)(idelalisib)tablets What is the most important information I should know about Zydelig?Zydelig can cause serious side effects that can lead to death, including:
- Liver problems. Abnormal liver blood test results are common during treatment with Zydelig. Zydelig can cause severe liver problems. Your healthcare provider will do blood tests before and during your treatment with Zydelig to check for liver problems. Tell your healthcare provider right away if you get any of the following symptoms of liver problems:
- yellowing of your skin or the white part of your eyes (jaundice)
- dark or brown (tea colored) urine
- pain in the upper right side of your stomach area (abdomen)
- bleeding or bruising more easily than normal
If you have any of the above serious side effects during treatment with Zydelig, your healthcare provider may completely stop your treatment, stop your treatment for a period of time, or change your dose of Zydelig. See "What are the possible side effects of Zydelig?" for more information about side effects.
- Severe diarrhea. Diarrhea is common during treatment with Zydelig and can sometimes be severe. Tell your healthcare provider right away if the number of bowel movements you have in a day increases by six or more. Ask your healthcare provider about medicines you can take to treat your diarrhea.
- Lung problems (pneumonitis). Your healthcare provider may do tests to check your lungs if you have breathing problems during treatment with Zydelig. Tell your healthcare provider right away if you get new or worsening cough, shortness of breath, difficulty breathing, or wheezing. Your healthcare provider may treat you with a corticosteroid medicine if you develop lung problems.
- Infections. Zydelig can cause serious infections that may lead to death. Tell your healthcare provider right away if you have a fever or any signs of an infection during treatment with Zydelig.
- Tear in intestinal wall (perforation). Tell your healthcare provider or get medical help right away if you get new or worsening stomach area (abdomen) pain, chills, fever, nausea, or vomiting.
- Severe skin reactions. Tell your healthcare provider right away if you get any of the following symptoms during treatment with Zydelig:
- painful sores or ulcers on your skin, lips, or in your mouth
- severe rash with bulers or peeling skin
- rash with itching
- fever
- enlarged lymph nodes
What is Zydelig? Zydelig is a prescription medicine used to treat people with chronic lymphocytic leukemia (CLL), in combination with rituximab, when CLL comes back after prior cancer treatment and when rituximab treatment alone may be used due to other health problems.Zydelig should not be used as the first medicine to treat anyone, including people with CLL, small lymphocytic lymphoma (SLL), follicular lymphoma (FL), and other slow growing (indolent) non-Hodgkin lymphomas.Zydelig should not be used in combination with bendamustine and rituximab, or in combination with rituximab to treat people with FL, SLL, and other indolent non-Hodgkin lymphomas.It is not known if Zydelig is safe and effective in children. Do not take Zydelig if you:
- have had a serious allergic reaction to idelalisib.
- have had a severe skin reaction called toxic epidermal necrolysis (TEN) to any drug.
Before taking Zydelig, tell your healthcare provider about all of your medical conditions, including if you: Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Zydelig and certain other medicines may affect each other. Know the medicines you take. Keep a ul of your medicines and show it to your healthcare provider and pharmacist when you get a new medicine.
- have liver problems
- have lung problems
- have an infection
- are pregnant or plan to become pregnant. Zydelig may harm your unborn baby. Females who are able to become pregnant should have a pregnancy test before starting treatment with Zydelig.
- Females who are able to become pregnant should use effective birth control (contraception) during treatment with Zydelig and for 1 month after the last dose of Zydelig. Talk to your healthcare provider about birth control methods that may be right for you. Tell your healthcare provider right away if you become pregnant or think you are pregnant during treatment with Zydelig.
- Males with female partners who are able to become pregnant should use effective birth control (contraception) during treatment with Zydelig and for 3 months after the last dose.
- are breastfeeding or plan to breastfeed. It is not known if Zydelig passes into your breast milk. Do not breastfeed during your treatment with Zydelig and for 1 month after the last dose.
How should I take Zydelig?
- Take Zydelig exactly as your healthcare provider tells you to take it.
- Your healthcare provider may change your dose of Zydelig or tell you to stop taking Zydelig. Do not change your dose or stop taking Zydelig without first talking to your healthcare provider.
- Take Zydelig 2 times a day.
- You may take Zydelig with or without food.
- Take Zydelig tablets whole.
- Do not miss a dose of Zydelig. If you miss a dose of Zydelig by less than 6 hours, take the missed dose right away. Then take your next dose as usual. If you miss a dose of Zydelig by more than 6 hours, wait and take the next dose of Zydelig at your usual time.
What are the possible side effects of Zydelig? Zydelig can cause serious side effects, including:
- See "What is the most important information I should know about Zydelig?"
- Serious allergic reactions, including a severe reaction known as anaphylaxis. Tell your healthcare provider or get medical help right away if you have signs or symptoms of a serious allergic reaction during treatment with Zydelig, including:
- swelling of the face, lips, or tongue
- trouble breathing or swallowing
- feeling dizzy or faint
- rash or hives
- cough
- a fast heartbeat
- Low white blood cell count (neutropenia). Neutropenia is common during treatment with Zydelig and can sometimes be severe. Your healthcare provider will check your blood counts regularly during treatment with Zydelig. Tell your healthcare provider right away if you have a fever or any signs of an infection during treatment with Zydelig.
The most common side effects of Zydelig when used in combination with rituximab include:
- pneumonia
- fever
- tiredness
- rash
- cough
- nausea
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.These are not all the possible side effects of Zydelig. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. How should I store Zydelig? Keep Zydelig and all medicines out of reach of children.
- Store Zydelig between 68°F to 86°F (20°C to 30°C).
- Keep Zydelig in its original container.
- Do not use Zydelig if the seal over the bottle opening is broken or missing.
General information about the safe and effective use of Zydelig. Medicines are sometimes prescribed for purposes other than those uled in a Medication Guide. Do not use Zydelig for a condition for which it was not prescribed. Do not give Zydelig to other people, even if they have the same symptoms you have. It may harm them. You can ask your healthcare provider or pharmacist for information about Zydelig that is written for health professionals. What are the ingredients in Zydelig? Active ingredient: idelalisib Inactive ingredients: microcrystalline cellulose, hydroxypropyl cellulose, croscarmellose sodium, sodium starch glycolate, and magnesium stearate. The tablet coating contains polyethylene glycol, talc, polyvinyl alcohol, titanium dioxide and FD&C Yellow #6 or Sunset Yellow FCF Aluminum Lake (for the 100 mg tablet) and red iron oxide (for the 150 mg tablet).Manufactured and distributed by: Gilead Sciences, Inc. Foster City, CA 94404©2022 Gilead Sciences, Inc. All rights reserved For more information, call 1-800-445-3235 or go to www.Zydelig.com.205858-GS-005-MG
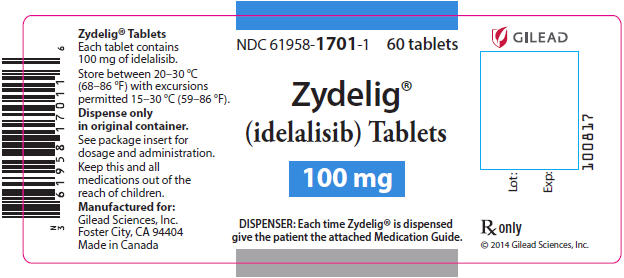
Principal Display Panel - 100 Mg Tablet Bottle Label
NDC 61958-1701-1 60 tablets
Zydelig® (idelalisib) Tablets
100 mg
DISPENSER: Each time Zydelig® is dispensedgive the patient the attached Medication Guide.
Principal Display Panel - 150 Mg Tablet Bottle Label
NDC 61958-1702-1 60 tablets
Zydelig® (idelalisib) Tablets
150 mg
DISPENSER: Each time Zydelig® is dispensedgive the patient the attached Medication Guide.

DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site